Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1716
Peer-review started: October 11, 2021
First decision: November 7, 2021
Revised: December 18, 2021
Accepted: January 5, 2022
Article in press: January 5, 2022
Published online: February 16, 2022
Processing time: 122 Days and 17.8 Hours
Vedolizumab, a newer class of integrin antagonist biological agents, has been applied to treat patients with moderate-to-severe Crohn’s disease (CD) and ulcerative colitis (UC), especially for patients who are refractory to traditional therapies and tumor necrosis factor antagonists. However, some rare but life-threatening adverse effects warrant pharmacovigilance. We describe the first fatal case of vedolizumab-associated severe diffuse interstitial lung disease in China.
We present a case of new-onset diffuse parenchymal lung disease developing under treatment with vedolizumab in a patient with UC. After two doses of vedolizumab, he developed persistent fever and progressively worsening dyspnea. Extensive workups, including bronchoalveolar lavage, transbronchial lung biopsy and metagenomic next-generation sequencing, identified no infectious causes, and other potential causes (such as tumors and cardiogenic pulmonary edema) were also excluded. As a result, a diagnosis of vedolizumab-related interstitial lung disease was established. Unfortunately, although corticosteroids and empiric antibiotics were administered, the patient eventually died of respiratory failure.
Vedolizumab-related interstitial lung disease in patients with UC is rare but potentially lethal. Gastroenterologists and pulmonologists should be aware of vedolizumab-related adverse drug reactions.
Core Tip: Vedolizumab is the treatment of choice for patients with moderate-to-severe ulcerative colitis who are refractory to tumor necrosis factor antagonists. However, some rare but potentially lethal drug-associated adverse effects warrant pharmacovigilance. We present a case of new-onset diffuse parenchymal lung disease development under treatment with vedolizumab in a patient with ulcerative colitis. After two doses of vedolizumab, he developed persistent fever, progressively worsening dyspnea and eventually died of respiratory failure. The patient was eventually diagnosed with vedolizumab-related interstitial lung disease, in spite of the few case reports found after reviewing the literature. We aim to raise gastroenterologists’ and pulmonologists’ vigilance to this uncommon adverse event.
- Citation: Zhang J, Liu MH, Gao X, Dong C, Li YX. Vedolizumab-associated diffuse interstitial lung disease in patients with ulcerative colitis: A case report. World J Clin Cases 2022; 10(5): 1716-1722
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1716.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1716
Vedolizumab is a fully humanized monoclonal antibody. It is currently the only intestinal selective biological agent in the field of inflammatory bowel disease (IBD) that targets α4β7 gastrointestinal integrin receptors and blocks the receptor’s interaction with mucosal addressin cell adhesion molecule-1, thereby inhibiting the migration of T lymphocytes into the intestinal parenchymal tissue in order to reduce inflammation[1]. In March 2020, vedolizumab produced by Takeda Pharmaceutical Company was approved for marketing in China for the first time. Although the clinical effectiveness of this brand has been continuously verified and recognized[2], safety and adverse events have also attracted negative attention. Here, we describe one fatal case of vedolizumab-associated severe interstitial lung disease in a patient with ulcerative colitis (UC). We also reviewed the existing literature in English and found only seven case reports of vedolizumab-associated lung diseases, mainly in patients with IBD.
A 61-year-old Chinese male was initially admitted to the gastroenterology department of our hospital with chief complaints of recurrent abdominal pain, diarrhea, mucopurulent hematochezia and weight loss.
The patient was diagnosed with UC 12 years prior to admission, and he had been treated with multiple conventional therapies, including, oral and topical aminosalicylates, dexamethasone enema, oral corticosteroids, selective leukocyte absorption treatment and intestinal flora adjustment treatment. In spite of these treatments, he experienced frequent flare-ups and was admitted to the hospital 3 times over the past 9 mo. Due to these failed conventional therapies, the patient was administered adalimumab 160 mg by subcutaneous injection. However, the symptoms continued with 10 to 20 bowel movements daily, and the modified Truelove and Witts severity index suggested moderately to severely active UC. As a result, the patient was started on vedolizumab. After the first dose of vedolizumab (300 mg intravenous infusion), fever at 39 °C and fatigue occurred the next day. He was treated with intravenous mezlocillin, foscarnet sodium, and ornidazole, but the fever persisted. The second dose of vedolizumab was administered 2 wk later, and the patient responded well regarding his intestinal symptoms; however, he presented with new-onset dyspnea at rest and nonproductive cough 2 d after the second vedolizumab treatment. Half a month later, the patient was admitted to the Department of Respiratory and Intensive Care Unit (RICU) due to severe dyspnea.
There was no significant medical history.
Upon arrival to the RICU, a body temperature of 36.8 degrees Celsius, a blood pressure of 128/90 mmHg, a heart rate of 97 beats/min, and a respiratory rate of 28 times/min were noted. The remaining physical examination was unremarkable except for diffuse inspiratory crackles in both lungs.
Lab data revealed the following: white blood cells 11.10 × 109/L, neutrophils 68.6%, lymphocytes 23.2%, hemoglobin 130 g/L and platelets 328 × 109/L. Serum C-reactive protein was increased at 111 mg/L (normal range ≤ 8 mg/L), erythrocyte sedimentation rate at 64 mm/h (normal range ≤ 15 mm/h), fecal calprotectin at 250.9 ug/g (normal range 0-50 ug/g) and procalcitonin was normal at 0.07 ng/mL (normal range ≤ 0.5 ng/mL). A fecal occult blood test showed positive occult blood with 0-1 white blood cells per high-power field. Stool cultures for Salmonella, Shigella and Campylobacter were all negative. Arterial blood gas analysis showed that pO2 was 41 mmHg breathing ambient air. Extensive microbiology assays (blood and sputum culture, 1,3-beta-D-glucan, galactomannan testing, aspergillus antibody, cryptococcal capsular polysaccharide antigen, mycoplasma antibody, human immunodeficiency virus antibody, cytomegalovirus, Epstein–Barr virus, A and B influenza virus PCR assays, and, antibodies of Toxoplasma gondii, rubella, herpes simplex virus and legionella) identified no infectious causes. Serologic examination included rheumatoid factor, antinuclear antibody panel, ds-DNA antibodies, anti-extractable nuclear antigen antibodies, myositis antibody panel, antineutrophil cytoplasmic antibody panel, and immunoglobulin, which were not elevated to pathologic levels. Cardiogenic pulmonary edema was excluded due to normal myocardial enzymes, B-type natriuretic peptide, echocardiogram and echocardiography. Some tumor markers, including, carcinoma embryonic antigen, cytokeratin 19 fragment and neuron-specific enolase, were increased at 7.68 ng/mL (normal range 0-5 ng/mL), 12.37 ng/mL (normal range 0-5 ng/mL) and 26.61 ng/mL (normal range 0-24 ng/mL), respectively, while alpha-fetoprotein and carcinoma antigen 125 and 199 were in the normal range. Bronchoalveolar lavage (BAL) and transbronchial lung biopsy (TBLB) were also performed. Cultures from the BAL were negative for bacteria, mycobacteria and fungi. Samples from the BAL and the peripheral blood were sent together for metagenomic next-generation sequencing (mNGS). This sequencing uses an untargeted DNA/RNA sequencing method to detect all potential pathogens, including, bacteria, fungi, viruses, and parasites[3]. In brief, the negative results of both mNGS and multiple microbiological cultures together effectively excluded infection.
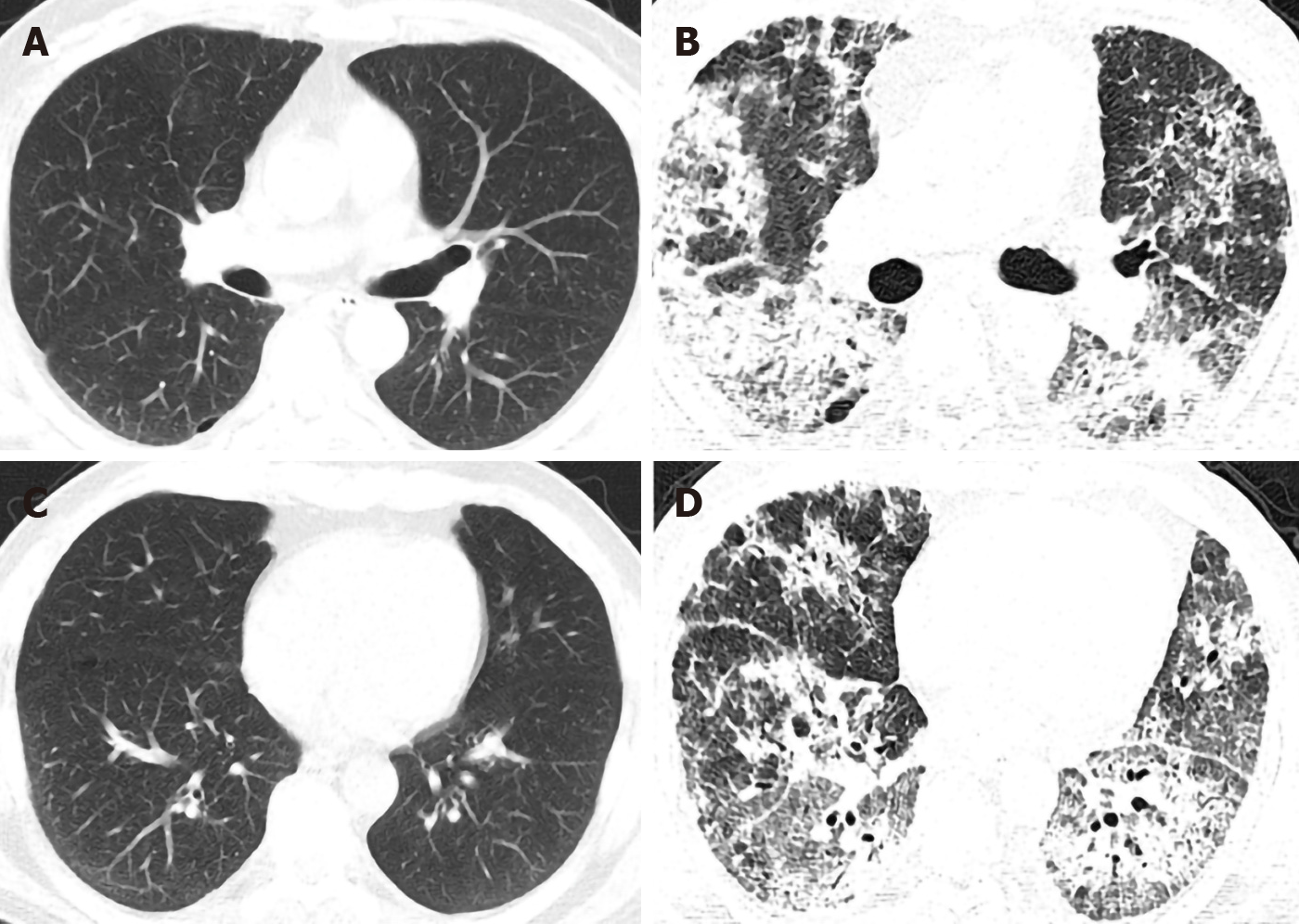
On high-resolution computed tomography (HRCT), new-onset diffuse infiltrates, interlobular thickening and fibrosis were noted compared to a HRCT from one month prior (Figure 1).
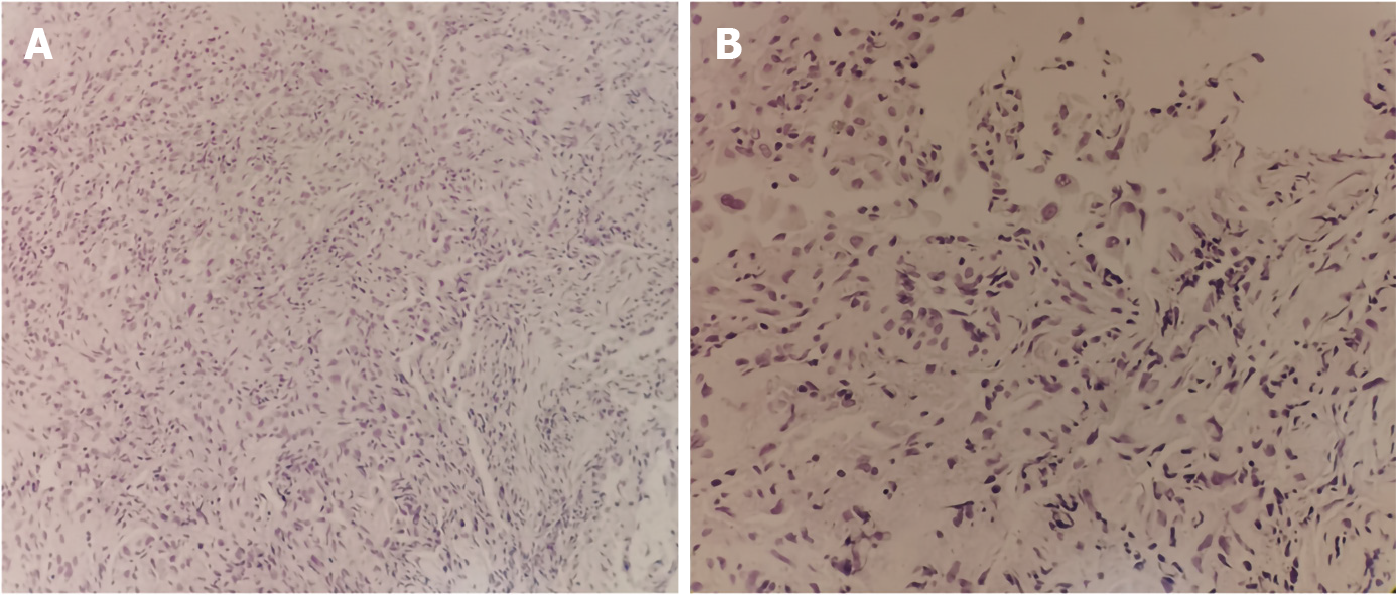
On histopathology, irregular glandular structures in the hyperplastic fibrous tissue were noted with scattered lymphocytes infiltrated in the interstitium. Intranuclear vacuoles, nuclear fragmentation, binuclear cells were seen (Figure 2). No tumor cells were noted and immunohistochemistry showed that adenoid structures were positive for cytokeratin AE1/AE3; epithelial cells were positive for the epidermal growth factor receptor (EGFR), p53 and negative for vimentin; positive immunostaining for Ki67 in some larger epithelial cells accounted approximately 15%; negative immunostaining for desmin was detected.
A diagnosis of vedolizumab-associated interstitial lung disease was made. The Naranjo adverse drug reaction scale [4] was calculated to be 6 (causality: probable).
Vedolizumab was discontinued, and the patient was started on methylprednisolone 80 mg/day. Three days later, intubation and mechanical ventilation was initiated due to refractory hypoxia. The anti-infective treatment was adjusted to linezolid, meropenem, caspofungin, compound sulfamethoxazole tablets and foscarnet sodium without any response.
Unfortunately, after nine days of hospitalization, the patient died due to respiratory failure.
The efficacy and safety of vedolizumab in patients with moderate to severe IBD have been confirmed in several pivotal clinical trials[5,6]. An integrated study analyzed 2830 IBD patients who used vedolizumab from 2009 to 2013 and showed that vedolizumab did not increase their risk of infection or malignancy, and the most common adverse events were nasopharyngitis, abdominal pain, headache and joint pain[7]. However, in the past 4 years, 7 cases of noninfectious lung injury related to vedolizumab have been reported, including 4 cases of UC and 3 cases of CD. In 2017, Sudheer et al[8] first reported a 58-year-old white man with UC who developed acute respiratory distress syndrome requiring intubation and mechanical ventilation after receiving 3 doses of vedolizumab. By withholding vedolizumab and applying the steroid, the patient was successfully discharged home. Another case was described by Eva et al[9] of a 52-year-old female with UC who suffered from new onset dyspnea and dry cough with chest CT showing diffuse ground-glass opacities. She was being treated with intravenous vedolizumab every 8 weeks for 2 years. Laboratory work did not identify infection, and the pathology of TBLB showed small bronchiole injury with debris and accumulation of mononuclear cells, macrophages and histiocytes. The fact that a complete resolution of symptoms and radiographic abnormalities was achieved by discontinuation of vedolizumab without any other treatments highly suggested vedolizumab-induced lung toxicity. Another recently published case has a similar clinical course as ours. A 39-year-old male diagnosed with UC presented with acute severe interstitial lung injury while receiving vedolizumab treatment[10]. While vedolizumab cessation and systemic steroid administration helped this patient, our patient was refractory to his therapy and finally passed away. Cucinotta et al[11] reported the off-label use of vedolizumab in a 13-year-old child with UC, and after three doses of vedolizumab, the child developed a persistent cough that resolved after vedolizumab discontinuation.
Strictly speaking, drug-induced pulmonary toxicity is not an extraintestinal manifestation of IBD[9,12]. Even so, over half of interstitial lung disease and granulomatous lung disease cases in IBD patients are drug-related; therefore, more differential diagnoses are necessary[13]. On that basis, we also reviewed 3 case reports of patients with CD. They presented with dyspnea, dry cough or fever with new-onset abnormal chest CT results (including pulmonary nodules, ground-glass opacities, pulmonary infiltrates or pleural effusions) after receiving 3-4 doses of vedolizumab[14-16]. On histopathology, lung biopsies from all 3 cases revealed noncaseating granulomatous inflammation. In terms of clinical outcome, 2 patients were successfully treated with prednisone, 1 patient failed systemic steroid treatment but was responsive to infliximab treatment, and complete resolution of pulmonary disease was achieved in all three cases.
In our case, we made a diagnosis of vedolizumab-induced lung injury for the following reasons. First, the patient had no respiratory symptoms or interstitial changes on his previous chest CT, even though his UC was actively relapsing during the past 9 months. Second, the new symptoms following the application of vedolizumab and new-onset diffuse parenchymal changes on CT highly suggested an adverse drug reaction. Third, the resolution of intestinal symptoms and the evolution of respiratory injury occurring directly after the administration of vedolizumab may be attributed to the drug mechanism of vedolizumab itself. One study suggested that vedolizumab could induce an upregulation of β1 expression on lymphocytes (which is an integrin component involved in pulmonary homing)[14], thereby facilitating the development of pulmonary inflammation and injury. Fourth, the abnormalities in the chest CT of our case were the most severe when compared to the above published cases. The reason our patient was not responsive to systemic corticosteroid treatment was due to the devastating damage of the lung tissue and the delay in time to a diagnosis. Last, in addition to conventional microbiological tests, we also utilized the advanced mNGS technique, which has a much higher sensitivity than that of conventional tests in mixed pulmonary infection diagnoses [17]. It has been reported that the sensitivity of mNGS for pathogen detection was 97.1%, with a negative predictive value of 94.1%[18]. Moreover, extensive anti-infective therapy aiming to cover all possible pathogens was administered without any improvement of symptoms. All the facts discussed above basically excluded the possibility of infection. To the best of our knowledge, this is the first fatal case of vedolizumab-associated interstitial lung disease reported in China. There was an additional death reported in which a 70-year-old man with a UC flare was being treated with prednisone and vedolizumab, but this patient had previously had mild chronic shortness of breath with chest CT showing bilateral interstitial fibrosis before receiving vedolizumab; therefore, we cannot confirm that it was vedolizumab-related[19].
Vedolizumab-related interstitial lung diseases in patients with IBD can be potentially fatal (as in our case presentation). Gastroenterologists and pulmonologists should raise their awareness regarding these cases. Timely diagnosis, early discontinuation of the offending drug and systemic corticosteroid treatment could prevent irreversible fibrosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nikolić M, Triantafillidis J S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Fischer A, Zundler S, Atreya R, Rath T, Voskens C, Hirschmann S, López-Posadas R, Watson A, Becker C, Schuler G, Neufert C, Atreya I, Neurath MF. Differential effects of α4β7 and GPR15 on the homing of effector and regulatory T cells from patients with UC to the inflamed gut in vivo. Gut. 2016;65:1642-1664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 2. | Baumgart DC, Bokemeyer B, Drabik A, Stallmach A, Schreiber S; Vedolizumab Germany Consortium. Vedolizumab induction therapy for inflammatory bowel disease in clinical practice--a nationwide consecutive German cohort study. Aliment Pharmacol Ther. 2016;43:1090-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 3. | Gu W, Miller S, Chiu CY. Clinical Metagenomic Next-Generation Sequencing for Pathogen Detection. Annu Rev Pathol. 2019;14:319-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 833] [Article Influence: 119.0] [Reference Citation Analysis (0)] |
| 4. | Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, Domecq C, Greenblatt DJ. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7061] [Cited by in RCA: 8196] [Article Influence: 186.3] [Reference Citation Analysis (0)] |
| 5. | Feagan BG, Rutgeerts P, Sands BE, Hanauer S, Colombel JF, Sandborn WJ, Van Assche G, Axler J, Kim HJ, Danese S, Fox I, Milch C, Sankoh S, Wyant T, Xu J, Parikh A; GEMINI 1 Study Group. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369:699-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1576] [Cited by in RCA: 1865] [Article Influence: 155.4] [Reference Citation Analysis (1)] |
| 6. | Sandborn WJ, Feagan BG, Rutgeerts P, Hanauer S, Colombel JF, Sands BE, Lukas M, Fedorak RN, Lee S, Bressler B, Fox I, Rosario M, Sankoh S, Xu J, Stephens K, Milch C, Parikh A; GEMINI 2 Study Group. Vedolizumab as induction and maintenance therapy for Crohn's disease. N Engl J Med. 2013;369:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1416] [Cited by in RCA: 1567] [Article Influence: 130.6] [Reference Citation Analysis (1)] |
| 7. | Colombel JF, Sands BE, Rutgeerts P, Sandborn W, Danese S, D'Haens G, Panaccione R, Loftus EV Jr, Sankoh S, Fox I, Parikh A, Milch C, Abhyankar B, Feagan BG. The safety of vedolizumab for ulcerative colitis and Crohn's disease. Gut. 2017;66:839-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 509] [Cited by in RCA: 610] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 8. | Nambiar S, Karippot A, Oliver T. Vedolizumab-Associated Acute Respiratory Distress Syndrome. Am J Ther. 2018;25:e592-e593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | De Backer E, Bode H, Baert F. New-Onset Diffuse Parenchymal Lung Disease in a 52-Year-Old Woman With Ulcerative Colitis. Gastroenterology. 2020;158:478-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Rizos ED, Antonogiannaki EM, Chatzidakis A, Kallieri M, Tsilogianni Z, Manali ED, Economopoulos N, Triantafyllou K, Papiris SA, Polymeros D. Vedolizumab-induced acute interstitial lung injury in a 39-year-old male with ulcerative colitis. Eur J Gastroenterol Hepatol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Cucinotta U, Dipasquale V, Costa S, Pellegrino S, Ramistella V, Romano C. Vedolizumab-associated pulmonary manifestations in children with ulcerative colitis. J Clin Pharm Ther. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Lu DG, Ji XQ, Liu X, Li HJ, Zhang CQ. Pulmonary manifestations of Crohn's disease. World J Gastroenterol. 2014;20:133-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Eliadou E, Moleiro J, Ribaldone DG, Astegiano M, Rothfuss K, Taxonera C, Ghalim F, Carbonnel F, Verstockt B, Festa S, Maia L, Berrozpe A, Zagorowicz E, Savarino E, Ellul P, Vavricka SR, Calvo M, Koutroubakis I, Hoentjen F, Salazar LF, Callela F, Cañete Pizarro F, Soufleris K, Sonnenberg E, Cavicchi M, Wypych J, Hommel C, Ghiani A, Fiorino G; ECCO CONFER COMMITTEE. Interstitial and Granulomatous Lung Disease in Inflammatory Bowel Disease Patients. J Crohns Colitis. 2020;14:480-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Lissner D, Glauben R, Allers K, Sonnenberg E, Loddenkemper C, Schneider T, Siegmund B. Pulmonary Manifestation of Crohn's Disease Developed Under Treatment With Vedolizumab. Am J Gastroenterol. 2018;113:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Myc LA, Girton MR, Stoler MH, Davis EM. Necrobiotic Pulmonary Nodules of Crohn's Disease in a Patient Receiving Vedolizumab. Am J Respir Crit Care Med. 2019;199:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Abu Shtaya A, Cohen S, Kogan Y, Shteinberg M, Sagool O. Crohn's Disease with Atypical Extra-Intestinal Manifestations Developing Under Treatment with Vedolizumab. Eur J Case Rep Intern Med. 2021;8:002265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Wang J, Han Y, Feng J. Metagenomic next-generation sequencing for mixed pulmonary infection diagnosis. BMC Pulm Med. 2019;19:252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 160] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 18. | Fang X, Mei Q, Fan X, Zhu C, Yang T, Zhang L, Geng S, Pan A. Diagnostic Value of Metagenomic Next-Generation Sequencing for the Detection of Pathogens in Bronchoalveolar Lavage Fluid in Ventilator-Associated Pneumonia Patients. Front Microbiol. 2020;11:599756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 19. | Collins HW, Frye JW. Interstitial Lung Disease in a 70-Year-Old Man with Ulcerative Colitis. ACG Case Rep J. 2018;5:e28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |