Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1689
Peer-review started: August 31, 2021
First decision: November 17, 2021
Revised: November 22, 2021
Accepted: January 8, 2022
Article in press: January 8, 2022
Published online: February 16, 2022
Processing time: 163 Days and 13.9 Hours
Orbital hemorrhage can be classified as traumatic or spontaneous depending on its cause. Spontaneous orbital hemorrhage refers to an internal orbital hemorrhage without apparent cause. Therefore, we aimed to describe a case of an orbital hematoma after a severe cough the night before due to inhalation of cooking oil fumes.
A 46-year-old woman was referred to our hospital with a complaint of exophthalmos accompanied with blurred vision, pain, binocular diplopia, and dizziness lasting for 5 h noted on waking in the morning. She also experienced nausea and vomiting due to high pressure of orbit and dizziness. Based on the auxiliary examination and her medical history, the patient was finally diagnosed with bulbar conjunctival vascular lesion combined with spontaneous retrobulbar hematoma. The patient was administered tobramycin and dexamethasone eye ointment, and applied pressure dressing on the left eye to stop the bleeding. Simultaneously, we administered intravenous etamsylate, oral Yunnan Baiyao capsule, intravenous mannitol to reduce orbital pressure, and intravenous dexamethasone injection at 10 mg/dL combined with neurotrophic therapy to reduce tissue edema. Among them, the Yunnan Baiyao capsule is a traditional Chinese herbal medicine to remove stasis and stop bleeding; thus, it promotes blood circulation and relieves pain resulting in reduced edema of the lesion site. The symptoms did not improve significantly during the first 2 d of treatment. We speculate that high orbital pressure and binocular diplopia induced frequent nausea and vomiting in the patient, causing increased pressure on the superior vena cava and leading to repeated orbital bleeding. After the second day, the symptoms started gradually improving.
This case further emphasizes the importance of comprehensive, detailed medical history and careful ophthalmic examination of the patient.
Core Tip: Orbital hemorrhage can be classified as traumatic or spontaneous according to its cause. Spontaneous orbital hemorrhage is an extremely rare and vision-threatening condition that may occur due to a variety of systemic predisposing factors. This case report suggests that patients with malformed periorbital vasculature should be alert for the risk of spontaneous intraorbital hemorrhage. In previous literature, we found reports of retrobulbar hematomas caused by sneezing or vomiting. However, to our knowledge, this is the first reported case of apparent bulbar conjunctival vascular malformation combined with retrobulbar hematoma caused by severe coughing.
- Citation: Lei JY, Wang H. Bulbar conjunctival vascular lesion combined with spontaneous retrobulbar hematoma: A case report. World J Clin Cases 2022; 10(5): 1689-1696
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1689.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1689
Orbital hemorrhage can be classified as traumatic or spontaneous depending on its cause. Spontaneous orbital hemorrhage refers to internal orbital hemorrhage without apparent cause with sudden onset, manifesting as proptosis, ophthalmoplegia, ocular distension, pain, increased intraocular pressure, vision loss, diplopia, loss of pupillary reflexes, and optic disc or retinal pallor[1]. Spontaneous orbital hemorrhage is an extremely rare and vision-threatening condition. It may occur due to various systemic predisposing factors such as hypertension, atherosclerosis, intraorbital vascular malformation, and hematologic diseases (abnormal platelet aggregation, hemophilia, and deficiency of human coagulation factor IX). Hass et al[2] reported that the Valsalva maneuver (when caused by vomiting and coughing) is another uncommon etiologic factor. Orbital hemangioma is the most common benign orbital tumor involving one eye, accounting for 24% of orbital tumors. It usually occurs in the muscle cone and is caused by congenital vascular anomalies and can be diagnosed using magnetic resonance imaging (MRI) or computed tomography (CT). Treatment aims to lower the intraorbital pressure and protect the optic nerve from damage. Pharmacotherapy may be considered in cases with minor retrobulbar hemorrhage; however, if the pain in the patient's eye or head is intolerable, or corneal function and vision are significantly affected, surgery is required[1].
Therefore, we report a patient with bulbar conjunctival vascular malformation combined with a spontaneous retrobulbar hematoma that was mistaken for anemia when admitted to a local hospital.
A 46-year-old woman was referred to our hospital on February 16, 2021, for left eye protrusion combined with blurred vision, pain, binocular diplopia, and dizziness lasting for 5 h noted on waking in the morning. She also experienced nausea and vomiting due to high intraocular pressure and dizziness.
The patient recalled having a severe cough the night before the hospital visit, due to inhalation of cooking oil fumes. Upon initial admission to a local hospital, her complete blood count suggested anemia, and her left eye subconjunctival vascular malformation was mistaken as being caused by a hemorrhage. The local hospital discovered a retrobulbar hematoma and suspected that it was caused by a blood system disease; therefore, she was referred to our hospital for a systematic examination.
The patient had a history of heavy menstrual bleeding, lasting approximately 15 d. She denied other medical and surgical histories.
The patient’s personal and family histories were negative.
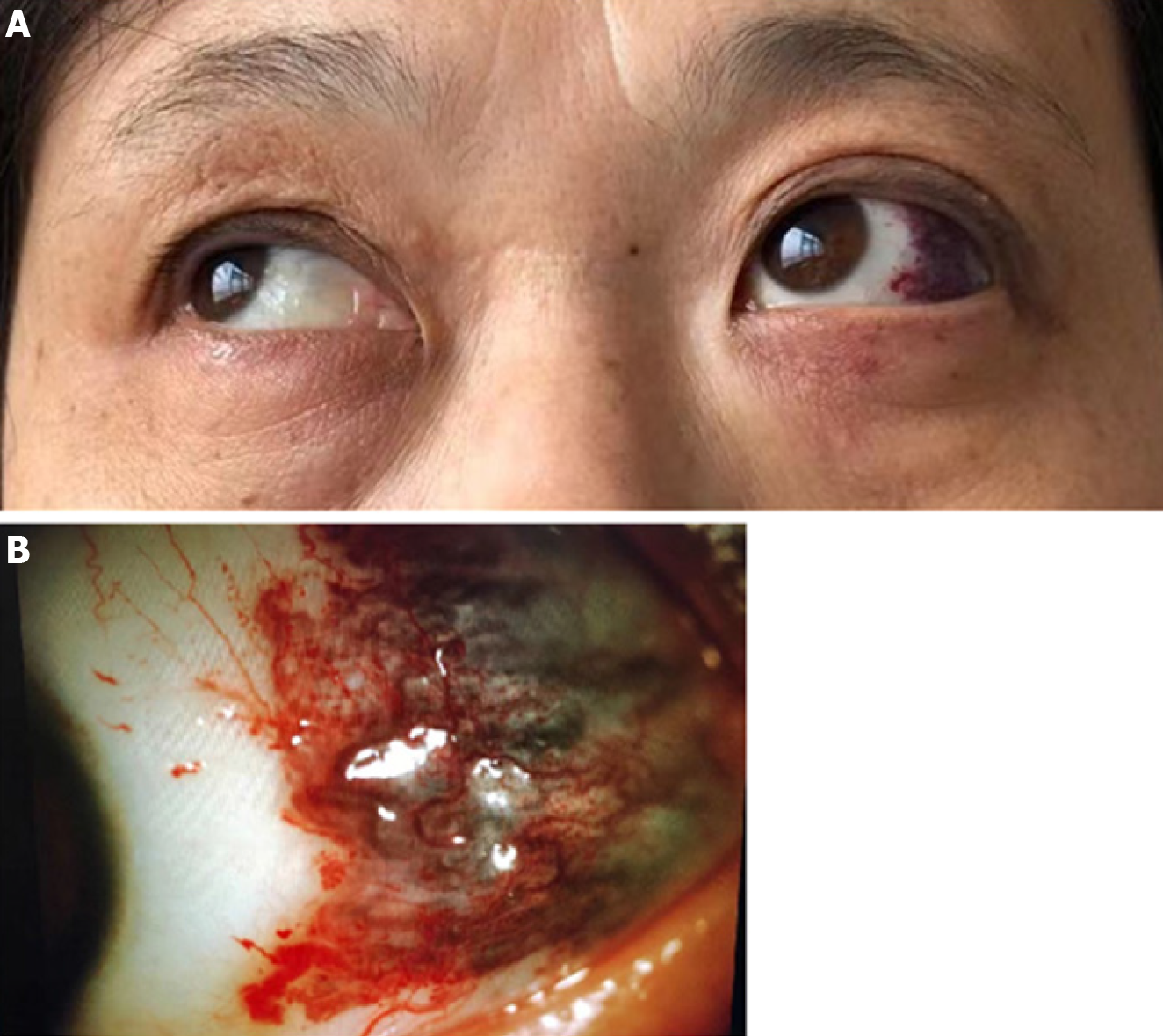
The visual acuity of the right eye was 0.04 (-7.00/-0.75 × 100 = 0.8), the left eye was 0.08 (-7.50/-2.00 × 65 = 0.3). The bilateral intraocular pressure was 19 mmHg and 21 mmHg, respectively. There was no redness or swelling in the left eyelid, but the lift was limited, and the upper eyelid covered the upper half of the pupil. The left eyeball protruded forward and was lowered (Figure 1A), the eye movements were limited to up gaze. Slit-lamp examination revealed that her left conjunctiva was not congestible, and curled blood vessels were seen under the conjunctiva on the temporal side, with a dark purple color and a range of approximately 1 cm × 1 cm (Figure 1B). Pupillary reflexes were insensitive, and no obvious abnormalities were observed in the fundus. The exophthalmos of the right and left eye were 14.5 mm and 23 mm, respectively, and the distance between the lateral margin of both orbitals was 100 mm.
Screening showed a hemoglobin concentration of 76 g/L, hematocrit of 29.1%, mean erythrocyte volume of 67.2 fL, a ferritin level of 4.69 ng/mL, and coagulation profile was within normal limits.
Gynecological B-ultrasound examination revealed multiple uterine fibroids.
A CT scan indicated left eye protrusion, and orbital near the bottom side showed a clumpy high-density mass (88 HU); the cross-section of this shadow was approximately 2.3 cm × 1.5 cm. No obvious disruption of the orbital wall bone structure was observed.
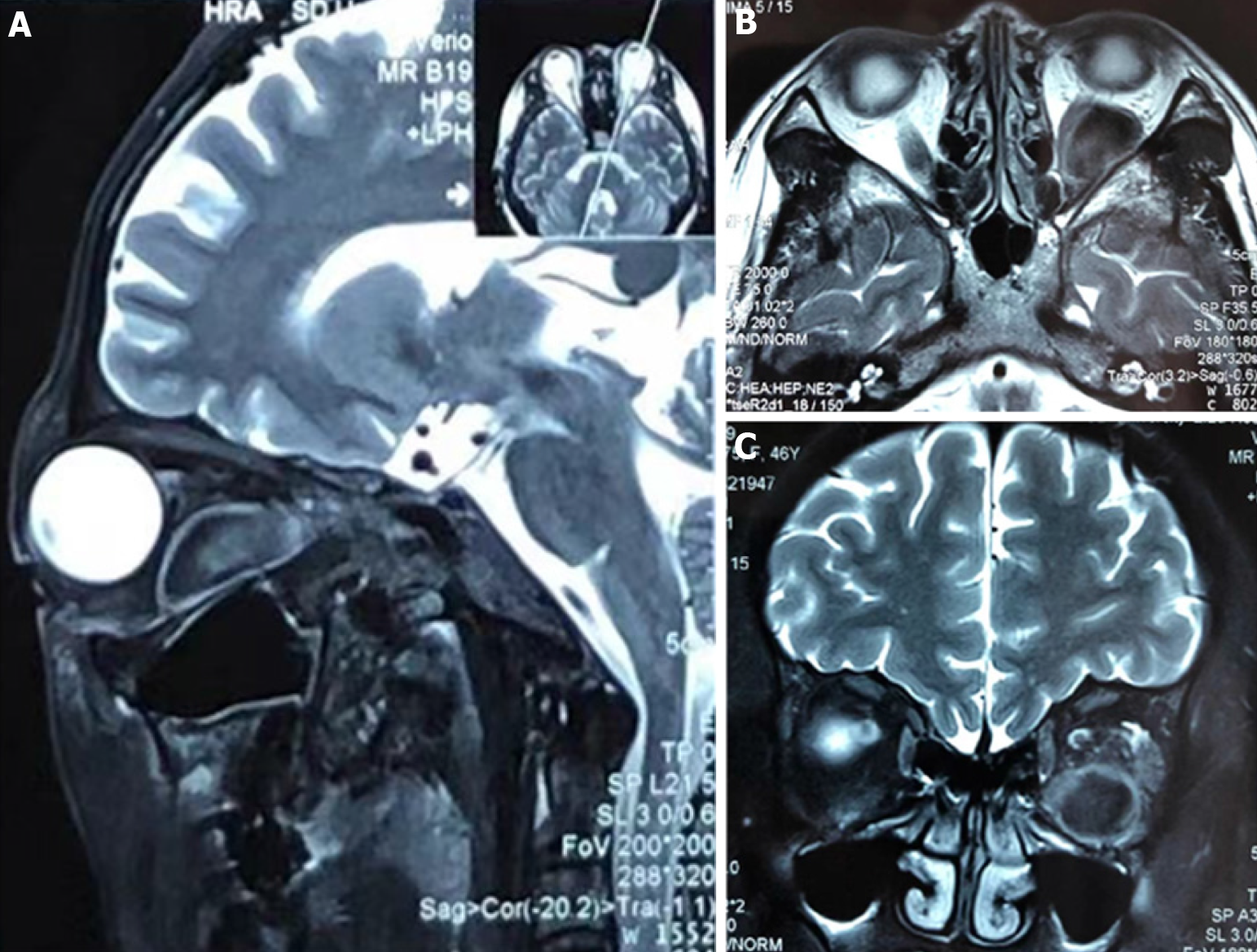
MRI scans of the orbits showed protrusion of the left eye and an elliptical long-short T1 Long-short T2 signal focus was observed in the lateral optic nerve of the left orbital muscle cone, with smooth edges and low signal on diffusion-weighted imaging. The left hyperdense retrobulbar mass displaced the optic nerve superomedially (Figure 2).
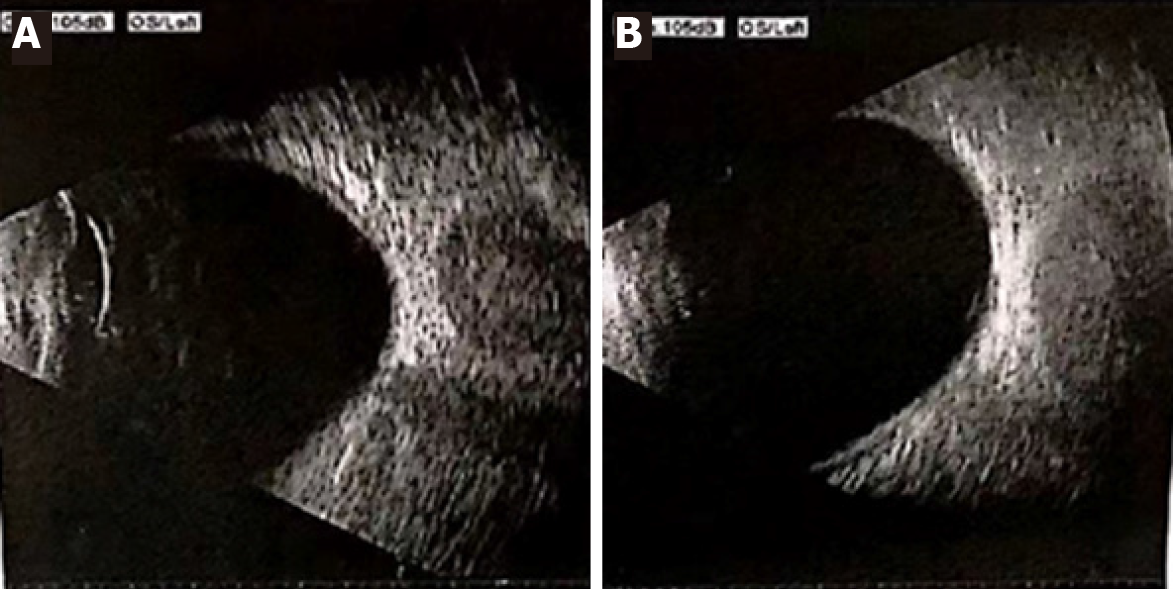
Ocular ultrasound showed uneven echo of the posterior eyeball mass of the left eye that disappeared while the gain reduced, suggestive of goiter of the left orbit (Figure 3).
Based on the auxiliary examination and medical history, the diagnoses were as follows: (1) Spontaneous retrobulbar hematoma; (2) Bulbar conjunctival vascular lesion; (3) Anemia; (4) Myopia of both eyes; and (5) Multiple uterine fibroids.
The patient received tobramycin and dexamethasone eye ointment, and the left eye was bandaged with pressure. Simultaneously, intravenous etamsylate, oral Yunnan Baiyao capsule, intravenous mannitol to reduce orbital pressure, and intravenous dexamethasone injection at 10 mg/dL combined with neurotrophic therapy to reduce tissue edema, were administered.
Two days after the initial treatment, symptoms had not improved significantly. The high orbital pressure was suspected of having induced frequent nausea and vomiting of the patient, increasing the pressure on the superior vena cava, leading to repeated orbital bleeding. However, her symptoms started to improve after the second day gradually. Considering that the visual acuity and corneal function were not significantly affected and the high risk of surgical treatment, we continued with a conservative (wait and see) treatment. After seven days, the visual acuity of the left eye was 0.08 (-5.25/-2.00 × 80 = 0.8), and the intraocular pressure in both eyes was 19 mmHg and 20 mmHg, respectively. The exophthalmos of the left eye was less severe than at the beginning of hospitalization; the right eye was 14.5 mm, and the left was 18 mm, and the distance between the lateral margin of both orbitals was 100 mm. Visual field examination revealed a visual field defect below the temporal of the left eye (Figure 4). MRI revealed a small reduction in the size of the lesion (1.8 cm × 1.3 cm). Prior to discharge, improvements were observed in the patient’s visual acuity and exophthalmos.
Orbital hemorrhage can be classified as traumatic or spontaneous according to its cause. In 2000, Sullivan et al[3] reviewed the records of 115 patients diagnosed with non-traumatic orbital hemorrhage and found that underlying vascular anomalies were present in 104 (90%), usually younger patients. Acute onset painful proptosis, associated with lid swelling or mass, was the most common presentation. Among these patients, only 7% underwent surgery for optic nerve compression, while 89% had complete or partial spontaneous resolution of the hemorrhage.
When the patient was first admitted to a local hospital, laboratory findings suggested anemia. Furthermore, the left eye subconjunctival vascular malformation was mistaken as being caused by the hemorrhage, supported by the orbital CT, which revealed an orbital hematoma in the left eye. Therefore, a spontaneous retrobulbar hematoma was suspected caused by a blood system disease and was then referred to our hospital for a systematic examination to determine the cause. When referred to our hospital, careful eye examination and comprehensive auxiliary examination revealed that the abnormal change under the conjunctiva of the left eye was a vascular malformation. In addition, we found that her anemia was due to multiple uterine fibroids; therefore, we concluded that the orbital hematoma was related to the malformed subconjunctival vessels and that there might have been similar malformed vessels in the intraorbital area before bleeding.
In this case, we found that the patient had a congenital venous vascular mass of the temporal bulbar subconjunctival malformation of the left eye. She recalled having a severe cough the night before due to the inhalation of cooking oil fumes. Therefore, it was considered more likely that the orbital hematoma was caused by rupture of the malformed intraorbital vessels rather than anemia. Due to the abnormal congenital development of these malformed vessels, the structure of their walls is defective; hence, they become weaker after luminal congestion. Any factor that causes increased internal jugular venous pressure may lead to rupture and bleeding of the vessels. In 2018, the International Society for the Study of Vascular Anomalies divided vascular anomalies into tumors and malformations. Vascular tumors were divided into three subtypes: benign, locally aggressive or borderline and malignant. Vascular malformations were divided into simple vascular malformation, mixed vascular malformation, well-known macrovascular malformation, vascular malformation combined with other lesions, vascular changes not yet classified and PIK3CA-related overgrowth spectrum[4]. Strictly speaking, to determine the origin of the vascular tissue of the patient's subconjunctival and intraorbital anomalies, a histopathological study is necessary. However, after conservative treatment, the patient's condition was controlled and to avoid further bleeding, pathological samples were not taken.
The onset of spontaneous orbital hemorrhage is usually sudden and can manifest as proptosis, ophthalmoplegia, pain, pressure, vision loss, diplopia, loss of pupillary reflexes, optic disc, retinal pallor, nausea, and vomiting[2,5]. The clinical presentation of our patient was therefore typical and comprehensive.
The Valsalva maneuver has been reported to be a cause of non-traumatic orbital hemorrhage. In 2004, Hass et al[2] investigated the incidence of orbital hemorrhage following cosmetic eyelid surgery and found that among 26433 patients, 149 developed orbital hemorrhage. This development was most common within the first 3 h after surgery and related to hypertension, perioperative aspirin use, postoperative vomiting, and increased physical activity. Liovic et al[6] reported a case of a 24-year-old female patient with nontraumatic subperiosteal orbital hemorrhage in the 25th week of pregnancy, presenting with painless left globe proptosis and blurred vision after vomiting. Considering that the patient was pregnant and without any signs of optic nerve compression, conservative treatment was adopted.
In the present case, the patient's symptoms did not improve significantly within the first 2 days of treatment. High orbital pressure was thought to induce frequent nausea and vomiting in the patient, which increased the intra-abdominal and intrathoracic pressure, which in turn increased the pressure in the superior vena cava. Since orbital veins do not contain valves, increased pressure in the superior vena cava would cause a rapid increase in orbital vessel pressure and lead to repeated orbital bleeding[1].
Both CT and MRI can be used to observe orbital structures and identify lesion types; however, while MRI is better than CT for enabling faster detection of vascular lesions, CT is the first choice for head and face emergencies (such as retrobulbar hemorrhage[7]).
There are three main options for the treatment of spontaneous retrobulbar hematoma[7]. First, conservative treatment is preferred if the hematoma scope is small and the early stage of the disease has little effect on visual function. Conservative treatments, such as hemostasis, corticosteroids, mannitol, and other treatments can be provided to reduce edema, orbital pressure and subsequently relieve the compression of the optic nerve and blood vessels. It is important to observe the patient's condition closely, and if there is a clear etiology, such as hypertension or blood system disease, the cause should be treated. Second, puncture of hematoma is preferred for a simple hematoma with high ocular prolapse, eye pain, unbearable headache, serious corneal function, and vision endangering. This procedure is performed under ultrasound guidance or after CT scan positioning, after which pressurized bandages are applied for several days. The main purpose of the pressure dressing is to prevent a sudden decrease in orbital pressure after the puncture, as this may lead to vascular dilatation and rebleeding. Third, orbital decompression is for orbital hematoma complicated with vascular lesions. Surgical treatment should be performed as early as possible to resolve the orbital lesions while the hematoma is being treated. For simple old hematomas with coagulated blood that are difficult to puncture or have a deep location, anterior or lateral wall orbital surgery is often needed. In the case of fresh active bleeding during the operation, adequate hemostasis should be performed, and attention should be paid to protecting the orbital tissue from injury. A drainage bar should be placed 24–48 h after the operation. Sharma et al[8] suggested that all non-traumatic spontaneous orbital hemorrhage cases should be urgently assessed for orbital compartment syndrome or optic nerve compression. Urgent lateral cantholysis and division of the orbital septum are necessary.
In our case, considering that the patient's visual acuity recovered significantly after conservative treatment, with a gradual decrease of the ocular protrusion; while also considering that both ultrasound-guided puncture hematoma and surgical treatment have greater risks, we decided to continue the conservative treatment.
Spontaneous retrobulbar hematoma should be differentiated from the following diseases: (1) traumatic intraorbital hemorrhage, most patients have a clear history of trauma, with a rapidly protruding eyeball often accompanied by facial tissue swelling, periorbital fracture, eyelid enclosure, disturbance of eye movement, and diplopia[9]; (2) intraorbital cystic tumors, which include epidermoid cysts, dermoid cysts, and cystic schwannomas. On CT, intraorbital cystic tumors present regular or irregular low-density shadows in homogeneous soft tissue density, while the intraorbital hematoma appears as a soft tissue mass. Enhanced CT or MRI should be performed when the differential diagnosis is difficult. On enhanced CT, the tumors are mostly enhanced overall, while on MRI, long T1 and T2 signals can be seen[10]; (3) orbital cellulitis, a secondary infection of the adjacent orbital tissues, in which sinus infection, especially in the ethmoid sinus, is the most common source of periorbital infection. Other sources include oral, tooth, gingival, or maxillofacial infections[11]. Spontaneous orbital hemorrhage often has no apparent predisposing factor; therefore, it may be misdiagnosed as orbital cellulitis if bleeding progresses rapidly; and (4) sinus mucous cysts, which are primarily found in the frontal and ethmoid sinuses. If the cyst bone wall is weak or disappears, then once the cyst ruptures, cystic fluid easily flows into the orbit, causing rapid protrusion of the eyeball. If the cyst is large, it can protrude directly into the orbit. In addition to the intraorbital mass, the mass connected to the sinus cyst can also be detected through imaging examination. The signal or density of both masses was similar, and the sinus cavity of the affected sinus was enlarged[12].
This case report suggests that patients with malformed periorbital vasculature should be alert for the risk of spontaneous intraorbital hemorrhage. In previous literature, we found reports of retrobulbar hematomas caused by sneezing or vomiting[2]. However, to the best of our knowledge, this is the first reported case of apparent bulbar conjunctival vascular malformation combined with retrobulbar hematoma caused by severe coughing.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nuño JSZ S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Deveer M, Cullu N, Beydilli H, Sozen H, Yeniceri O, Parlak S. Spontaneous Retrobulbar Haematoma. Case Rep Radiol. 2015;2015:796834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Hass AN, Penne RB, Stefanyszyn MA, Flanagan JC. Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthalmic Plast Reconstr Surg. 2004;20:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 89] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Sullivan TJ, Wright JE. Non-traumatic orbital haemorrhage. Clin Exp Ophthalmol. 2000;28:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | International Society for the Study of Vascular Anomalies. ISSVA Classification of Vascular Anomalies 2018. [accessed 2019 Jan]. Available from: https://www.issva.org/classification. |
| 5. | Richardson K, Perry M, White S. Post-traumatic eye observations M.C. Bater, P.L. Ramchandani, P.A. Brennan, Br. J. Oral Maxillofac. Surg. 43 (2005) 410-416. Br J Oral Maxillofac Surg. 2007;45:173-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Liovic M, Sekelj S, Janjetovic Z, Vukovic Arar Z. A case of nontraumatic subperiosteal orbital hemorrhage following vomiting in pregnancy. Int J Ophthalmol. 2020;13:1675-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Atalla ML, McNab AA, Sullivan TJ, Sloan B. Nontraumatic subperiosteal orbital hemorrhage. Ophthalmology. 2001;108:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Sharma N, O’Hagan S. Non-traumatic orbital haemorrhage as a complication of emergence from anaesthesia. Anaesth Rep. 2014;2:49-51. [DOI] [Full Text] |
| 9. | Murchison AP, Bilyk JR, Savino PJ. Traumatic Cranial Neuropathies. In: Black E, Nesi F, Calvano C, Gladstone G, Levine M, editors. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. New York: Springer, 2012: 165-197. [DOI] [Full Text] |
| 10. | Smoker WR, Gentry LR, Yee NK, Reede DL, Nerad JA. Vascular lesions of the orbit: more than meets the eye. Radiographics. 2008;28:185-204; quiz 325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 107] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Baiu I, Melendez E. Periorbital and Orbital Cellulitis. JAMA. 2020;323:196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Işık AÜ, Arslan S, Arslan E, Baykal S. A giant frontoethmoid mucocele with intracranial extension. Scott Med J. 2015;60:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |