Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1645
Peer-review started: August 23, 2021
First decision: October 22, 2021
Revised: November 4, 2021
Accepted: January 11, 2022
Article in press: January 11, 2022
Published online: February 16, 2022
Processing time: 172 Days and 4.5 Hours
Synovial chondromatosis is a disease originating from the synovium and characterized by the presence of metaplastic cartilaginous nodules in synovial cavities. The exact prevalence of synovial chondromatosis remains unknown, and the involvement of the shoulder joint is very rare. Synovial chondromatosis accompanied by subluxation of the humeral head without a history of trauma is rarely encountered, and to our knowledge, no published reports describe this condition.
We present two cases of synovial chondromatosis in the shoulder joint, accompanied by subluxation of the humeral head, in two arthroscopically managed adult patients. We performed arthroscopic labrum fixation and removal of the loose body from the shoulder joint. To identify primary and secondary categories, pathological analysis was arranged. Clinical and radiographic evaluations at the 1-mo follow-up were satisfactory.
The biomechanical function of the shoulder joint requires attention, especially following the detection of loose bodies, as observed with synovial chondroma occurring in rare sites. Arthroscopic management is successful in patients with synovial chondromatosis combined with shoulder subluxation.
Core Tip: Synovial chondromatosis accompanied with subluxation of the humeral head without a history of trauma is rarely encountered and, to our knowledge, there are no reports yet of this condition. We report two cases that had synovial chondromatosis accompanied with subluxation of the humeral head and it is the first to describe. Arthroscopic management was successful in patients with synovial chondromatosis combined with subluxation of the shoulder. Biomechanical working of the shoulder joint should not be ignored in synovial chondromatosis diagnosis, especially with the emergence of loose bodies such as in synovial chondroma occurring in rare sites.
- Citation: Tang XF, Qin YG, Shen XY, Chen B, Li YZ. Arthroscopic surgery for synovial chondroma of the subacromial bursa with non-traumatic shoulder subluxation complications: Two case reports. World J Clin Cases 2022; 10(5): 1645-1653
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1645.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1645
Synovial chondromatosis is a disease of unknown etiology, originating from the synovium and characterized by the presence of metaplastic cartilaginous nodules in synovial cavities, bursa, or tendon sheaths[1-3]. Synovial chondromatosis commonly presents in young to middle-aged men[4], and usually involves large joints, including the knee, hip, and elbow, but can occur in any synovial joint throughout the body. The disease most commonly affects the knee joint, followed by the hip and elbow; however, the occurrence of synovial chondromatosis in either the shoulder or ankle joints is extremely rare[3,5,6].
A diagnosis of synovial chondromatosis is often delayed due to initially mild and nonspecific symptoms[7]. If the intra-articular fragments are not adequately calcified, synovial chondromatosis can go undetected for years[8]. The complaints associated with synovial chondromatosis typically include joint pain, joint swelling, decreased mobility, and loose bodies[9]. However, synovial chondromatosis accompanied by subluxation of the humeral head in the absence of any history of trauma is rare and, to our knowledge, has not yet been reported in the literature, and the mechanism of subluxation has not ever been analyzed.
The most commonly recommended treatment for synovial chondromatosis is the surgical removal of loose bodies to ameliorate the associated symptoms. Currently, an arthroscopic approach is recommended for most shoulder pathologies[10,11]. The primary advantages of using arthroscopic approaches include decreased morbidity, synchronous visualization, and the ability to treat both intra- and extra-articular pathologies. Hypertrophic synovia and multiple loose bodies are typical arthroscopic findings[12,13].
In this report, we present two cases of synovial chondromatosis in the shoulder joint accompanied by subluxation of the humeral head treated with arthroscopic management in adult patients and discuss the potential underlying mechanisms involved in disease development.
Case one: A 56-year-old woman experienced severe right shoulder pain and decreased range of motion for 3 d without any history of trauma.
Case two: A 56-year-old woman experienced severe left shoulder pain with limited mobility for 3 mo, which worsened over the past 4 d, without any history of trauma prior to presence at our hospital.
Case one: As reported by the patient, the right shoulder pain was accompanied by limited mobility and significant swelling due to slight external force over the previous 3 d. The pain and swelling continued to increase without systemic treatment, and the patient was referred to our hospital for further treatment. After physical examination, imaging examinations, and a review of the patient’s medical history, the patient was diagnosed with right shoulder joint dislocation.
Case two: The patient described left shoulder joint pain without an obvious cause and limited joint movement, which started 3 mo prior to presentation. Conservative treatments, such as acupuncture and therapeutic massage at a local hospital, did not provide symptom relief, and the pain had become aggravated over the past 4 d without any trauma.
Case one: The patient’s medical history was unremarkable, and she was in generally good health.
Case two: The patient’s medical history showed a 3-year history of hypertension, reaching as high as 160/100 mmHg, without regular oral antihypertensive medication, resulting in poorly controlled hypertension.
Case one: The physical examination revealed obvious swelling in the right shoulder, with an empty glenoid cavity and obvious deformity. Tenderness was detected in the spinous process of the cervical spine and in front of and above the right shoulder. Mobility was limited, and the Dugas sign was positive.
Case two: Physical examination revealed obvious swelling of the left shoulder joint, mild atrophy of surrounding muscles, positive tenderness in front of and above the left shoulder joint, positive Jobe sign, positive arm drop test, positive pain arc sign, and positive Dugas sign.
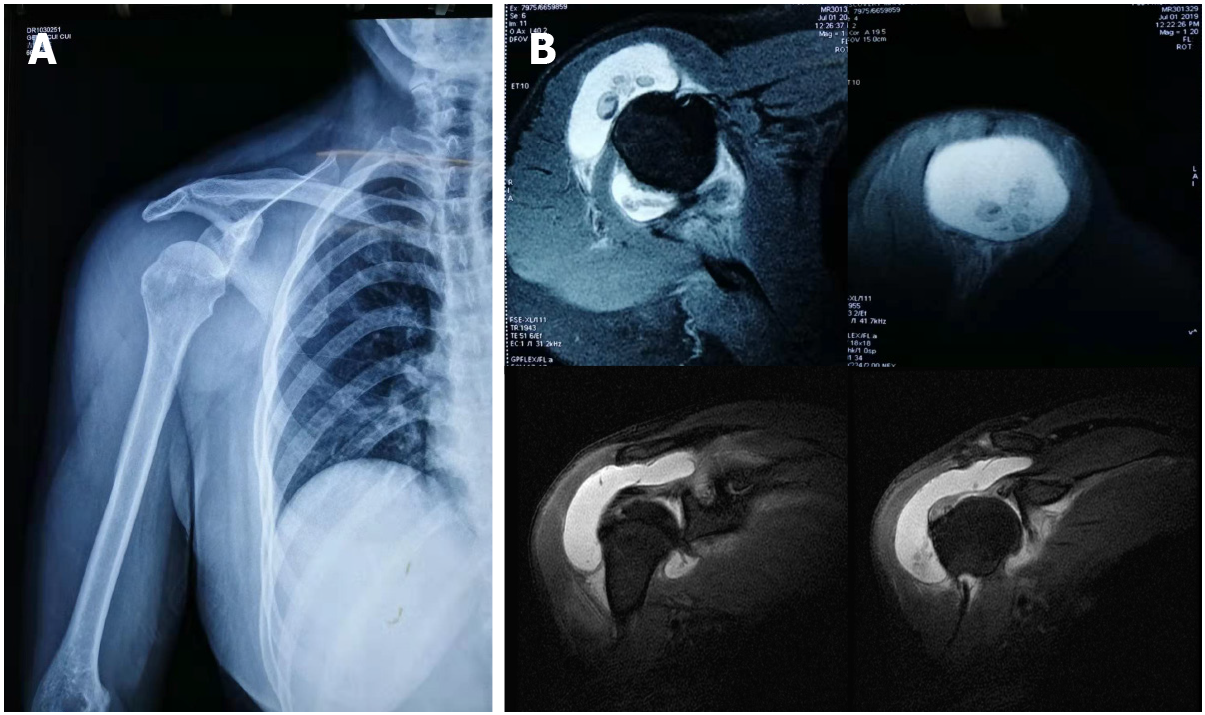
Case one: Radiographs showed subluxation of the shoulder joint (Figure 1A). Computed tomography (CT) indicated that the right humerus head was dislocated anteriorly and inferiorly. The joint space was narrowed, the shadow of the surrounding tissue was thick, and the shadow of the fluid density was visible within the joint cavity. A point-striped bone density shadow was observed near the pelvis of the right shoulder. Magnetic resonance imaging (MRI) examination of the shoulder joint indicated a quasi-circular, short T2 weighted signal in the shoulder cavity, with a large area of long T1 and long T2 liquid signals observed in the subacromial bursa (Figure 1B).
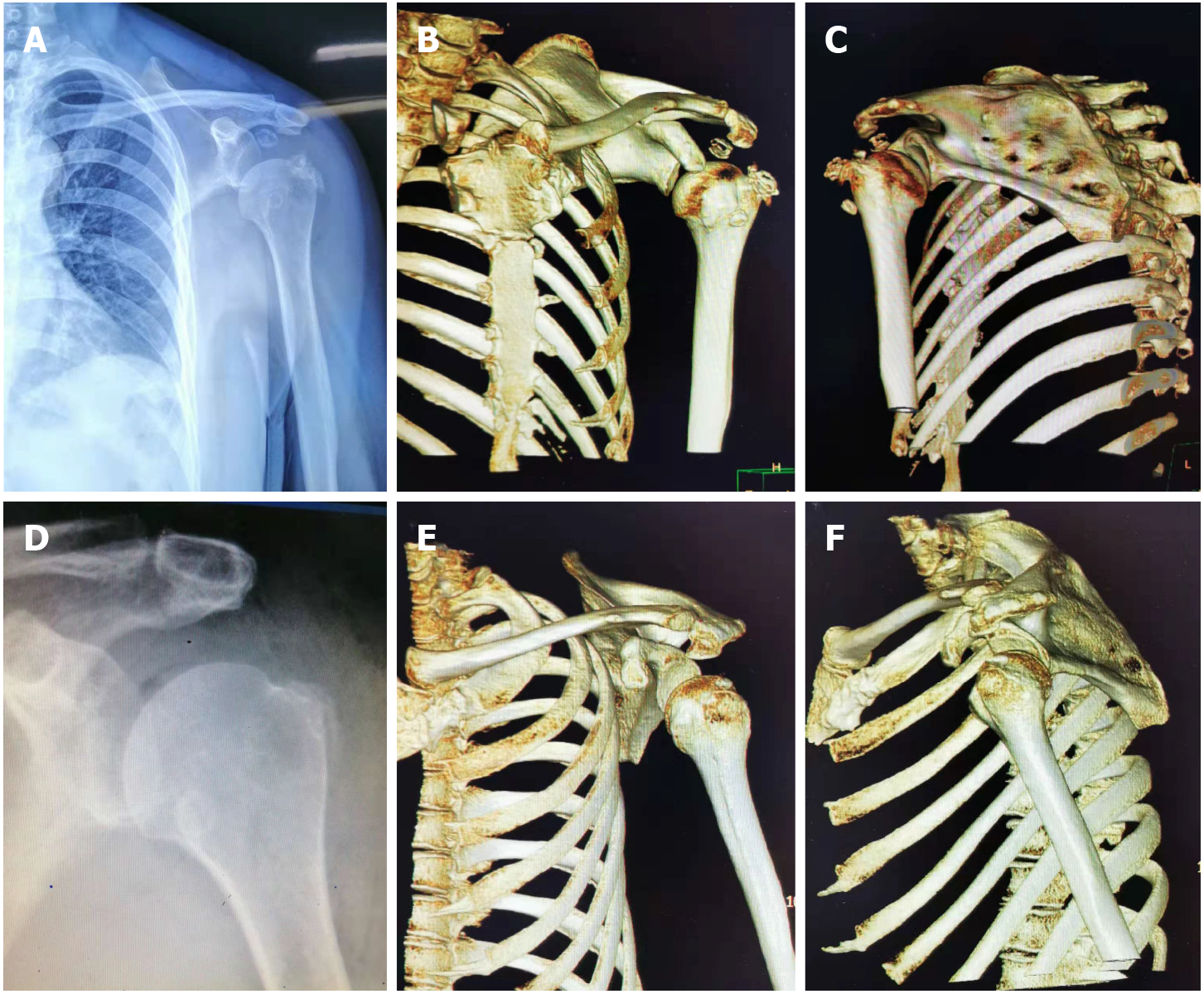
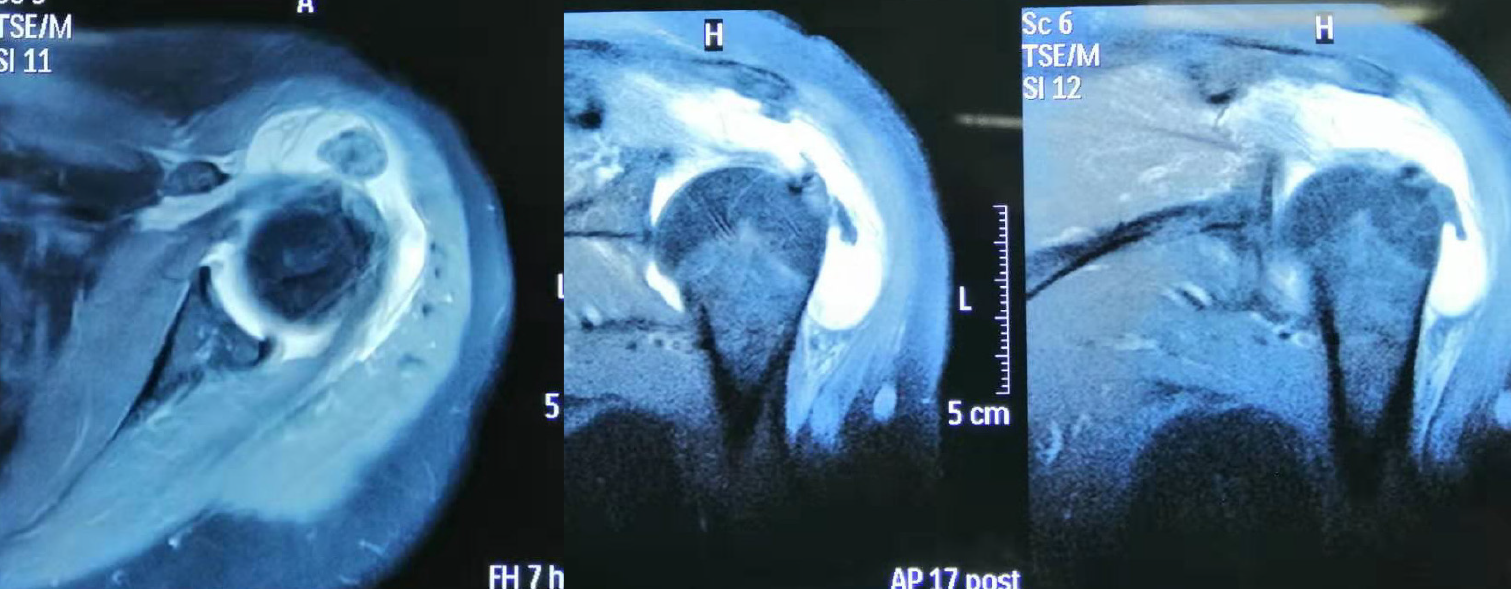
Case two: Radiography of the shoulder joint showed a dislocated left shoulder joint and the presence of multiple bone-like loose bodies within the glenohumeral joint space (Figure 2A). On three-dimensional CT, the left humeral head could be observed surrounded by sheet-like, low-density shadows. The CT value was approximately 25 HU, and the surrounding lipolysis remained clear, with multiple sheet-like, bone-like dense shadows visible. The head position was slightly lower than the normal anatomical relationship of the left humerus (Figure 2B and C). MRI examination of the shoulder joint showed a round, short T2-weighted signal, an irregular shape for the supraspinatus muscle, and patchy proton density–weighted image hyperintensity at the attachment point of the supraspinatus tendon in the joint cavity. Sheet-like long T1 and long T2 fluid signals in the subacromial space of the deltoid synovial sac were observed (Figure 3).
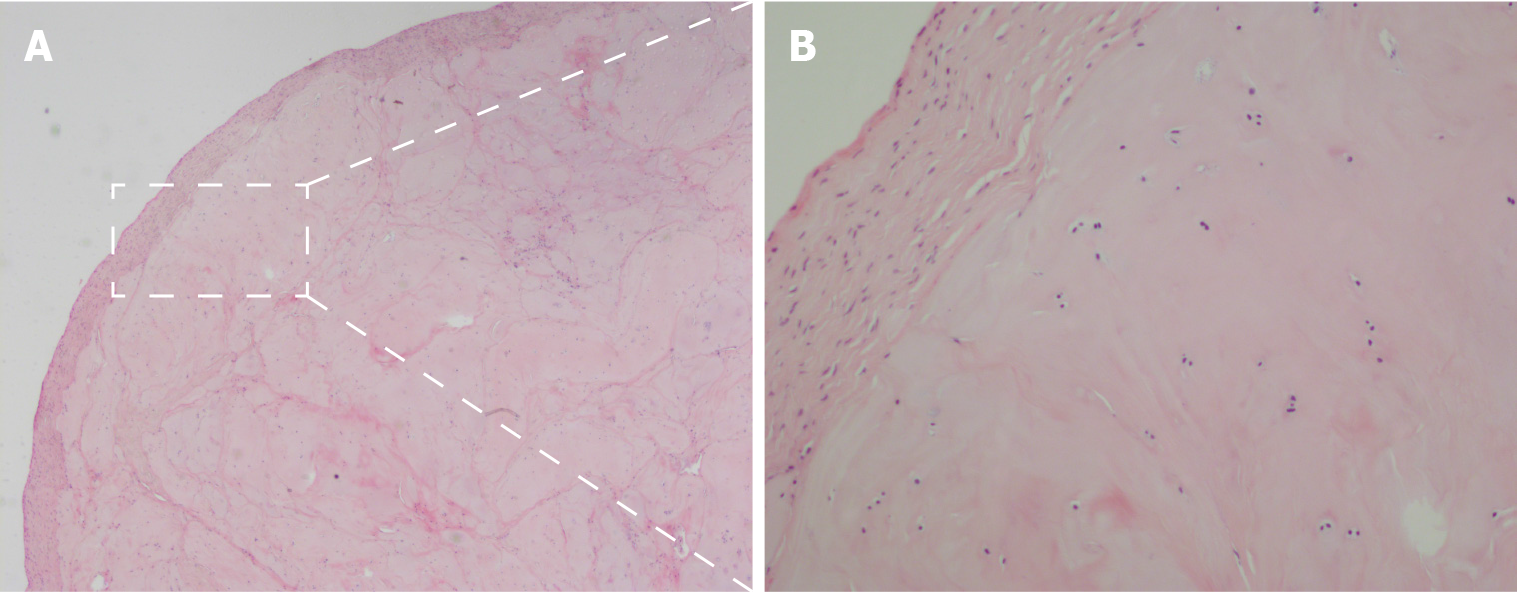
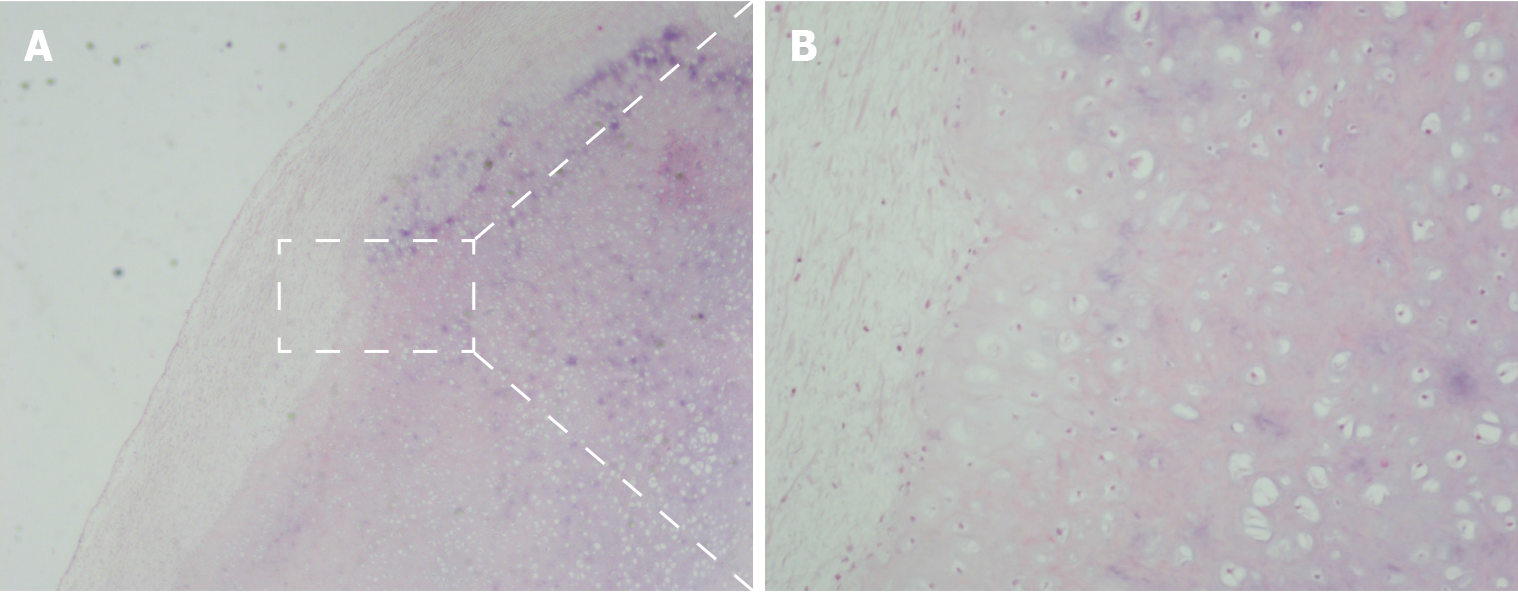
Case one: The pathological analysis showed right shoulder joint disease of the synovium and exfoliated cartilage. Hyperplastic cartilage tissue was submitted for inspection, which revealed degenerative local necrosis and ossification in some areas; the subacromial lesion synovium and loose bodies were submitted for inspection as suspected hyperplastic cartilage. The surface of the tissue was covered in a small amount of synovial membrane, consistent with synovial chondroma (Figure 4).
Case two: Upon pathological examination, the specimen was identified as a cartilaginous nodule surrounded by fibrous tissue with local calcification. Fragments of articular cartilage or subchondral lamellar bone were observed (Figure 5).
Case one: The final diagnosis was subluxation and synovial chondroma of the right shoulder joint.
Case two: Subluxation and synovial chondroma, along with calcified tendinitis of the left shoulder joint.
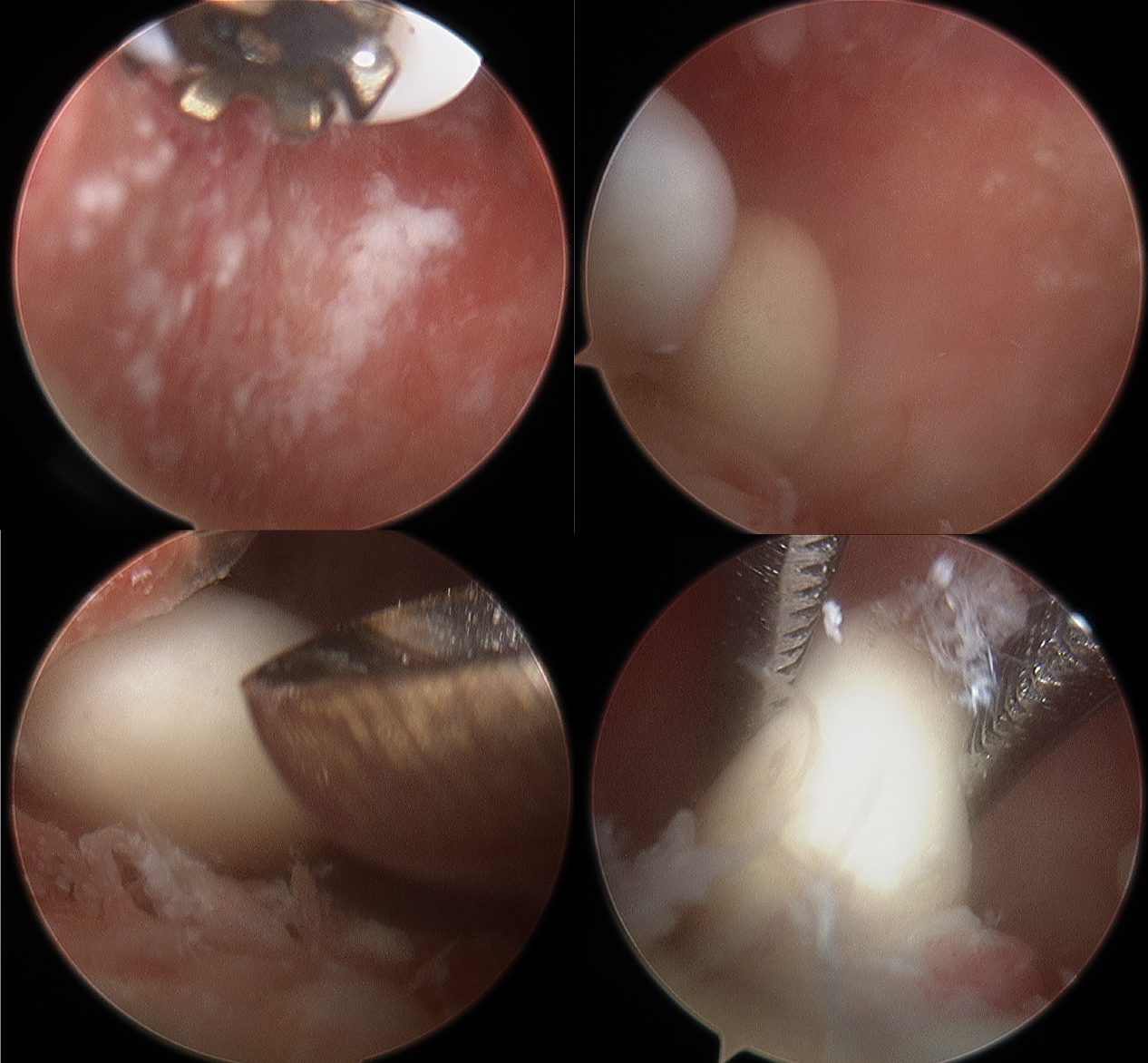
Case one: We performed arthroscopic labrum fixation and removal of the loose body from the shoulder joint. After successful anesthesia induction, the patient was placed in a left-sided lying position, the right limb was placed in an abduction position, and a traction weight of 4 kg was applied. The standard posterior approach was used for glenohumeral arthroscopy, which showed a large quantity of cartilaginous debris in the joint cavity (Figure 6). Arthroscopy revealed a free cartilage sheet, obvious synovial hyperplasia, massive exfoliation of the articular surface of the humeral head, scapular glenoid cartilage, degeneration of the long head of the biceps, an inferior anterior labrum, and separation of the joint capsule from the glenoid. During arthroscopy, both superior and anterior approaches were used to remove all free cartilage and exfoliate the cartilage from the articular head to proliferate the synovium. The anterior inferior joint capsule and labrum were loosened, and 2.9 mm anchors were implanted at the 5:30, 4:30, and 3:00 o’clock positions. The anterior inferior joint capsule and labrum were sutured by lifting and repositioning. The humeral head was located in the center of the joint, and the glenoid labrum was reset. The arthroscope was then moved to the subacromial space, which showed large amounts of synovial hyperplasia under the acromion, accompanied by cartilaginous fragments and free loose bodies, the proliferation of the subacromial capsule, and inflammatory changes. The proliferative synovial membrane, cartilage debris, and loose bodies were removed and sent for pathological examination. The joint cavity and subacromial space were washed with a large volume of normal saline. After checking the gauze and instruments, the incision was sutured, and the affected limb was suspended. After hanging and fixation, the operation was complete.
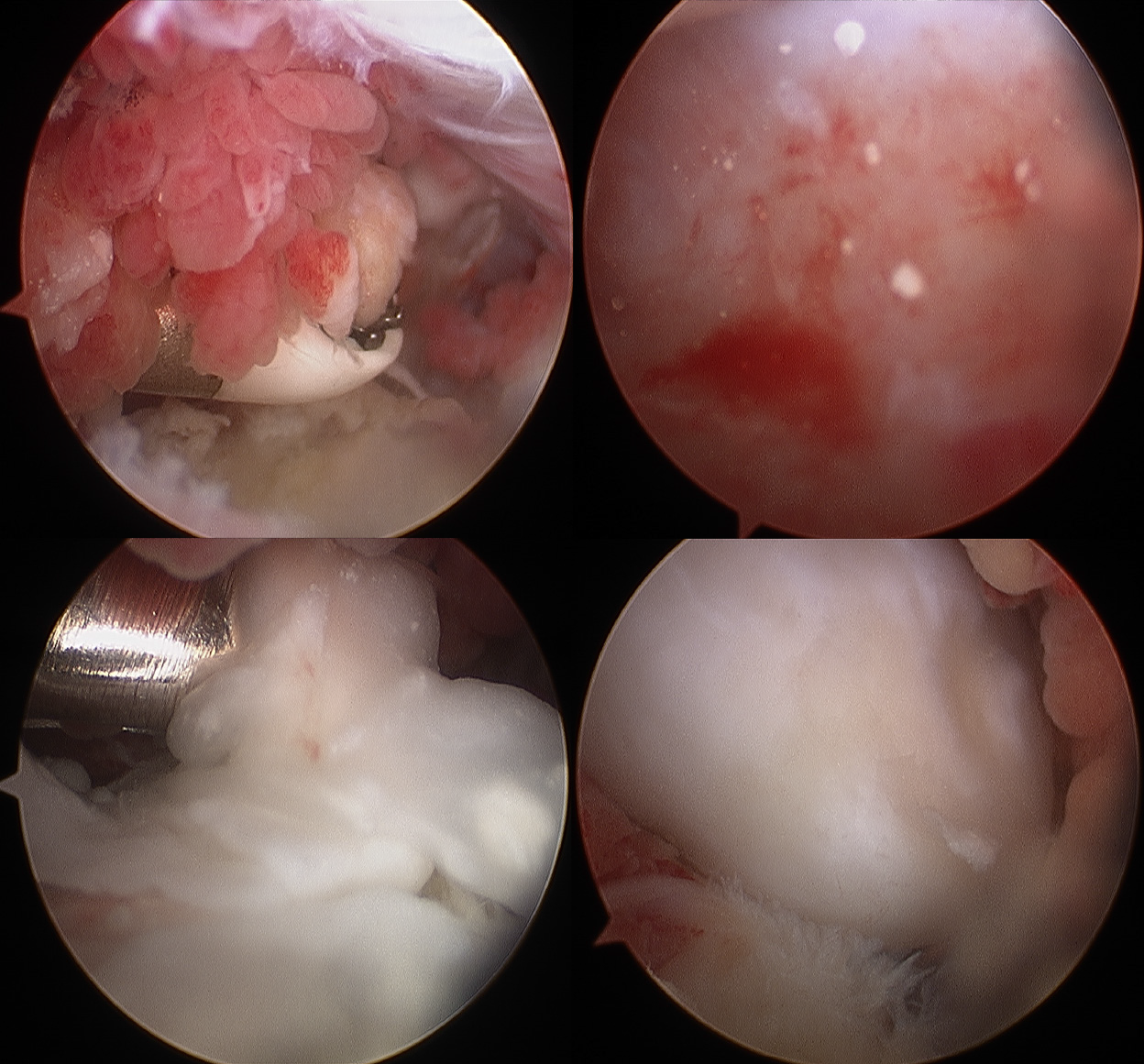
Case two: The loose bodies were removed from the shoulder joint under arthroscopic guidance through the following steps. After successful anesthesia induction, the patient was placed in the right decubitus and left limb abduction position, and a traction weight of 4 kg was applied. A standard posterior approach was utilized for glenohumeral arthroscopy after routine disinfection and draping were performed. Under arthroscopic guidance (Figure 7), the synovia of the joints were observed, featuring hyperplasia, with degeneration of the articular surface of the humeral head, scapula, biceps, and long head muscles; intact subscapularis, supraspinatus, and small round muscles; and degenerative lesions detected on the subspinal muscles. Two loose bodies were observed in the joint space, which were removed using nucleus pulposus forceps. An arthroscopic anterior approach was established to remove the synovial hyperplasia. The arthroscope was repositioned to the subacromial space, which revealed the hyperplasia of the outer edge of the front shoulder bone and subacromial bursa and inflammatory changes. After establishing a posterolateral approach, a synovial resection line was determined, and acromioplasty was performed. The joint cavity was washed with a large volume of physiological saline. After checking the gauze and instrument inventory, the incisions were sutured, covered with sterile dressing, and the limb was suspended.
Case one: Re-examination by postoperative radiography showed no loose bodies in the subacromial space. The humeral head returned to a normal anatomical relationship. The swelling and pain of the shoulder joint gradually disappeared, and shoulder joint function returned to normal. Range of movement exercises were started as soon as the patient was comfortable. At the 1-mo follow-up, the patient had pain-free range of movement in the right shoulder that was comparable to that in the left shoulder, with no remaining preoperative symptoms.
Case two: Postoperative radiographic re-examination showed no loose bodies in the subacromial space. The humeral head returned to its normal anatomical relationship (Figure 2D–F). The swelling and pain of the shoulder joint gradually disappeared, and shoulder joint function generally returned to normal. At the 1 mo follow-up, normal shoulder function was restored.
Synovial chondromatosis of the joints is a rare clinical condition with an unclear definition and diagnostic criteria[14], resulting in limited available knowledge regarding this condition. Synovial chondromatosis can be divided into primary and secondary categories[15]. Primary synovial chondromatosis involves no prior basic bone or joint lesions and is generally regarded as a benign neoplastic disease rather than synovial metaplasia, with a reported incidence of approximately 5%[16]. By contrast, secondary membrane chondromatosis typically occurs secondary to trauma, osteoarthritis, or rheumatoid arthritis[17,18]. Clinically, the signs and symptoms are nonspecific and may be suggestive of several pathological conditions. In most cases, the symptoms comprise pain or range of motion loss. Shoulder pain is one of the first symptoms, followed by the locking of the joint in some cases[18,19]. However, dislocation is not a typical feature. Both of our patients experienced a painful range of motion, with signs and symptoms typical of shoulder joint subluxation.
Most previously reported investigations have not described synovial chondromatosis accompanied by subluxation, and no previous literature reports have reported any clinical manifestations of joint subluxation; despite the presence of many loose bodies, no cases of joint dislocation have been reported. Koichi et al retrieved more than 200 loose bodies from a young female patient with a rare condition of secondary synovial chondromatosis in her right shoulder[20]. Hiroyuki extracted 17 free bodies from the subscapularis bursa of a confirmed case of synovial chondromatosis in a 12-year-old boy[21]. Therefore, we questioned the occurrence of shoulder dislocation in our patients, who were characterized by the presence of relatively few loose bodies. To our knowledge, previous case reports and studies have focused on the characteristic symptoms caused by loose bodies, such as joint pain, swelling, and limited mobility, without examining the biomechanical function of the shoulder joint. The emergence of loose bodies, such as those observed with synovial chondroma in unusual locations, disrupts the stabilization mechanism of the shoulder joint. The lever effect occurs during specific movements, resulting in shoulder joint dislocation.
The biomechanics of the glenohumeral joints depend on interactions between both static and dynamic stabilizing structures[22]. Static stabilizers include the bony anatomy, negative intra-articular pressure, glenoid labrum, and the glenohumeral ligaments, along with the joint capsule. The dynamic stabilizing structures include the rotator cuff muscles and other muscular structures surrounding the shoulder joint. The combined functions of these stabilizers serve to support multiple degrees of motion within the glenohumeral joint. When any one of these mechanisms fails, shoulder joint pathology, such as subluxation or dislocation, can occur[22,23].
Whether the observed synovial cartilage tumors observed in our patients represent primary or secondary hyperplasias and the order in which dislocation and synovial chondroma developed are other concerns. Histopathological identification is needed to differentiate between primary and secondary synovial chondromatosis[18]. According to Villacin et al[24], who delineated the histologic criteria for differentiating between primary and secondary synovial chondromatosis, in primary lesions, the chondrometaplasia foci in the synovium and loose bodies are characterized by a markedly disorganized pattern, with many binucleate, plump chondrocytes, and patchy, diffuse calcification. By contrast, in secondary lesions, fragments of articular cartilage or subchondral lamellar bone may be present in the loose bodies, and the pattern of calcification is zonal and ring-like, with uniform, evenly distributed chondrocytes[20,24]. Milgram suggested that primary synovial chondromatosis has three phases: (1) Active intrasynovial disease, without loose bodies; (2) transitional lesions, characterized by both active intrasynovial proliferation and loose bodies; and (3) multiple free bodies, without intrasynovial disease[25]. Combined with the operative findings of multiple loose bodies and the histologic absence of intrasynovial disease, patient 1 in our case report may have had phase 3 primary synovial chondromatosis, whereas patient 2 may have had a secondary synovial chondromatosis.
The treatment decision is made according to the patient’s age, symptoms, and the disease stage[6]. Preventing missed diagnoses and misdiagnoses and performing a differential diagnosis when loose bodies are detected are important concerns, especially when rotator cuff injuries are suspected. The differentiation between a loose body and an avulsion fracture is also necessary. If the intra-articular fragments are not adequately calcified, synovial chondromatosis can go undetected for years[26]. Obtaining a detailed medical history and performing complete physical examinations and MRI scans can contribute to the accurate diagnosis and treatment of synovial chondromatosis.
We believe that the biomechanical function of the shoulder joint should be considered, especially when loose bodies are detected, as observed with synovial chondroma occurring in rare sites. Arthroscopic management was successful in two patients with synovial chondromatosis combined with shoulder subluxation. In such conditions, subluxation is usually transient, and the humeral head returns spontaneously to its normal position after the operation.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Akbulut S S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Zhang H
| 1. | Blümlein H, Puls P, Schneider HM, Wunderlich T. [Benign and malignant chondromatosis of the joints. A contribution to the clinical aspects and histology of the disease]. Z Orthop Ihre Grenzgeb. 1980;118:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | McFarland EG, Neira CA. Synovial chondromatosis of the shoulder associated with osteoarthritis: conservative treatment in two cases and review of the literature. Am J Orthop (Belle Mead NJ). 2000;29:785-787. [PubMed] |
| 3. | Wiedemann NA, Friederichs J, Richter U, Bühren V. [Secondary synovial chondromatosis of the ankle joint]. Orthopade. 2011;40:807-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Davis RI, Hamilton A, Biggart JD. Primary synovial chondromatosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol. 1998;29:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 152] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Aydogan NH, Kocadal O, Ozmeric A, Aktekin CN. Arthroscopic treatment of a case with concomitant subacromial and subdeltoid synovial chondromatosis and labrum tear. Case Rep Orthop. 2013;2013:636747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Fukuda A, Uemura T, Nishimura A, Kato K, Sudo A. Arthroscopic Treatment of Primary Synovial Chondromatosis of the Subscapular Bursa: A Case Report. J Orthop Case Rep. 2020;9:40-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Sinikumpu JJ, Sinikumpu SP, Sirniö K, Näpänkangas J, Blanco Sequeiros R. Pediatric primary synovial chondromatosis of the shoulder, biceps tendon sheath and subcoracoid bursa. J Clin Orthop Trauma. 2020;11:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Miranda JJ, Hooker S, Baechler MF, Burkhalter W. Synovial chondromatosis of the shoulder and biceps tendon sheath in a 10-year-old child. Orthopedics. 2004;27:321-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Covall DJ, Fowble CD. Synovial chondromatosis of the biceps tendon sheath. Orthop Rev. 1994;23:902-905. [PubMed] |
| 10. | Jiménez-Martín A, Zurera-Carmona M, Santos-Yubero FJ, Pérez-Hidalgo S. Arthroscopic treatment of synovial chondromatosis, an unusual cause of shoulder pain. Reumatol Clin. 2014;10:416-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Ranalletta M, Bongiovanni S, Calvo JM, Gallucci G, Maignon G. Arthroscopic treatment of synovial chondromatosis of the shoulder: report of three patients. J Shoulder Elbow Surg. 2009;18:e4-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Duymus TM, Yucel B, Mutlu S, Tuna S, Mutlu H, Komur B. Arthroscopic treatment of synovial chondromatosis of the shoulder: A case report. Ann Med Surg (Lond). 2015;4:179-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Urbach D, McGuigan FX, John M, Neumann W, Ender SA. Long-term results after arthroscopic treatment of synovial chondromatosis of the shoulder. Arthroscopy. 2008;24:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Neumann JA, Garrigues GE, Brigman BE, Eward WC. Synovial Chondromatosis. JBJS Rev. 2016;4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Poyser E, Morris R, Mehta H. Primary synovial osteochondromatosis of the shoulder: a rare cause of shoulder pain. BMJ Case Rep. 2018;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Raval P, Vijayan A, Jariwala A. Arthroscopic Retrieval of over 100 Loose Bodies in Shoulder Synovial Chondromatosis: A Case Report and Review of Literature. Orthop Surg. 2016;8:511-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Díaz Fernández JF, Peraza Mc Liberty RA. Synovial osteochondromatosis of the shoulder: Case report and literature review. Reumatol Clin (Engl Ed). 2018;14:56-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Utashima D, Matsumura N, Suzuki T, Iwamoto T, Ogawa K. Clinical Results of Surgical Resection and Histopathological Evaluation of Synovial Chondromatosis in the Shoulder: A Retrospective Study and Literature Review. Clin Orthop Surg. 2020;12:68-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Shearer H, Stern P, Brubacher A, Pringle T. A case report of bilateral synovial chondromatosis of the ankle. Chiropr Osteopat. 2007;15:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Hamada J, Tamai K, Koguchi Y, Ono W, Saotome K. Case report: A rare condition of secondary synovial osteochondromatosis of the shoulder joint in a young female patient. J Shoulder Elbow Surg. 2005;14:653-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Katoh H, Ogawa K, Ikegami H, Inokuchi W, Toyama Y. Osteochondromatosis of the shoulder in a twelve-year-old boy. J Shoulder Elbow Surg. 2007;16:e15-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Lugo R, Kung P, Ma CB. Shoulder biomechanics. Eur J Radiol. 2008;68:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Ahmad CS, Wang VM, Sugalski MT, Levine WN, Bigliani LU. Biomechanics of shoulder capsulorrhaphy procedures. J Shoulder Elbow Surg. 2005;14:12S-18S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol. 1979;10:439-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 138] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am. 1977;59:792-801. [PubMed] |
| 26. | Isbell JA, Morris AC, Araoye I, Naranje S, Shah AB. Recurrent Extra- and Intra-articular Synovial Chondromatosis of the Ankle with Tarsal Tunnel Syndrome: A Rare Case Report. J Orthop Case Rep. 2017;7:62-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |