Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1598
Peer-review started: July 15, 2021
First decision: October 18, 2021
Revised: January 7, 2022
Accepted: January 11, 2022
Article in press: January 11, 2022
Published online: February 16, 2022
Processing time: 210 Days and 17.2 Hours
The jejunal nutrition tube has increasingly been used in clinical practice, and the results in frequent complications.
We present the case of a 74-year-old male patient who had been admitted to the intensive care unit for aspiration pneumonia and respiratory failure. When confirming the position of the jejunal tube by X-ray, we found that the feeding tube had been placed into the chest. The complications was a disaster, though the misplacement of jejunal feeding tube are uncommon.
We introduced a way of ultrasound-guided jejunum feeding tube placement to avert the disaster, which was convenient and economical.
Core Tip: We report a case of a patient who has a serious complication during the catheterization of the jejunal tube and introduce a way of using of bedside ultrasound to guide the placement of the jejunal tube to avert the disaster, which was convenient and economical.
- Citation: Jiang YP, Zhang S, Lin RH. Uncommon complication of nasoenteral feeding tube: A case report. World J Clin Cases 2022; 10(5): 1598-1601
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1598.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1598
Early enteral nutrition in critically ill patients who cannot eat by mouth is widely recommended by the clinical practice guidelines of nutrition[1]. For patients at high risk of aspiration and who were intolerant of oral or gastric feeding the advice is to place a post-pyloric feeding tube[2,3]. Complication of jejunal feeding tubes are rare. A recent report revealed that a jejunal tube caused gastrointestinal perforation[4]. In this case report, we will present a case where a jejunal feeding tube was placed into the chest and provide a brief overview of a method to avoid the complication of placing a jejunal feeding tube. Written informed consent was obtained from the patient’s family for publication of this manuscript and any accompanying images.
A 74-year-old male patient who with a history of chronic obstructive pulmonary disease (COPD) was admitted to the intensive care unit (ICU) for aspiration pneumonia and respiratory failure.
He had a prolonged course of treatment and a nasoduodenal feeding tube blind placed at the bedside.
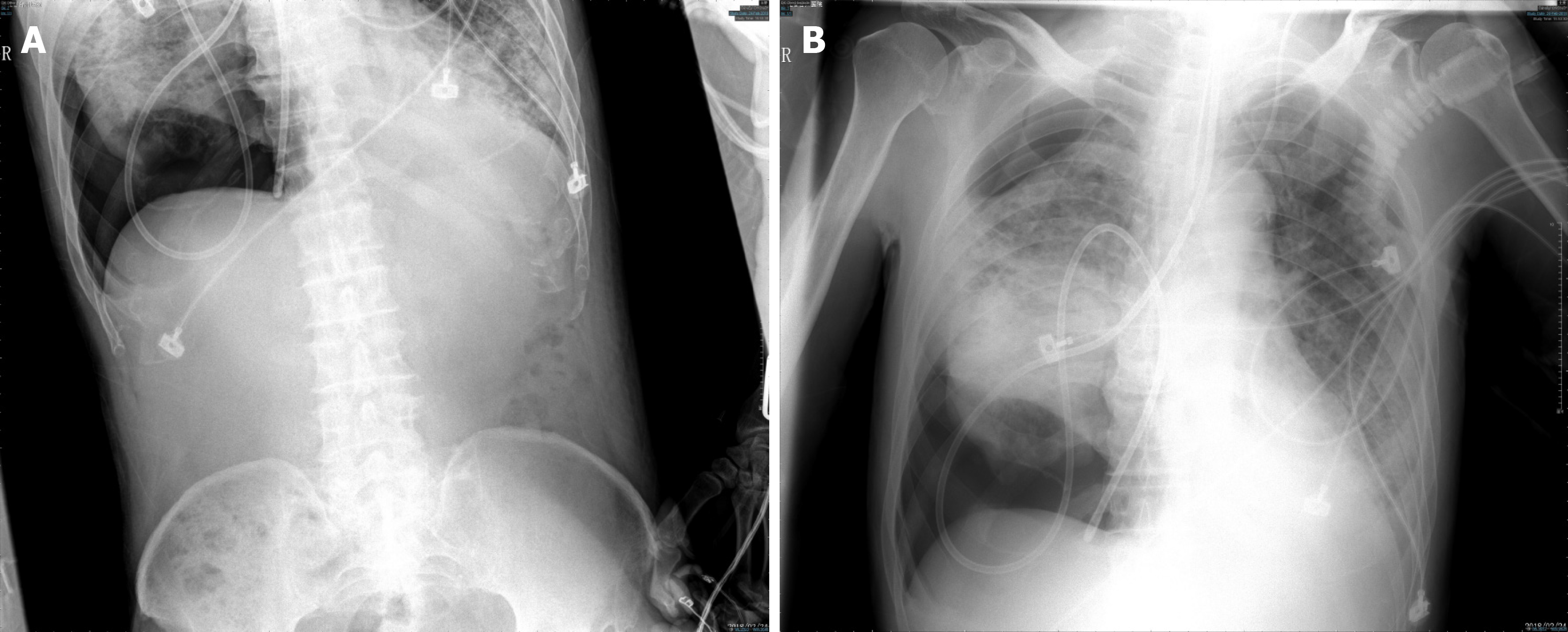
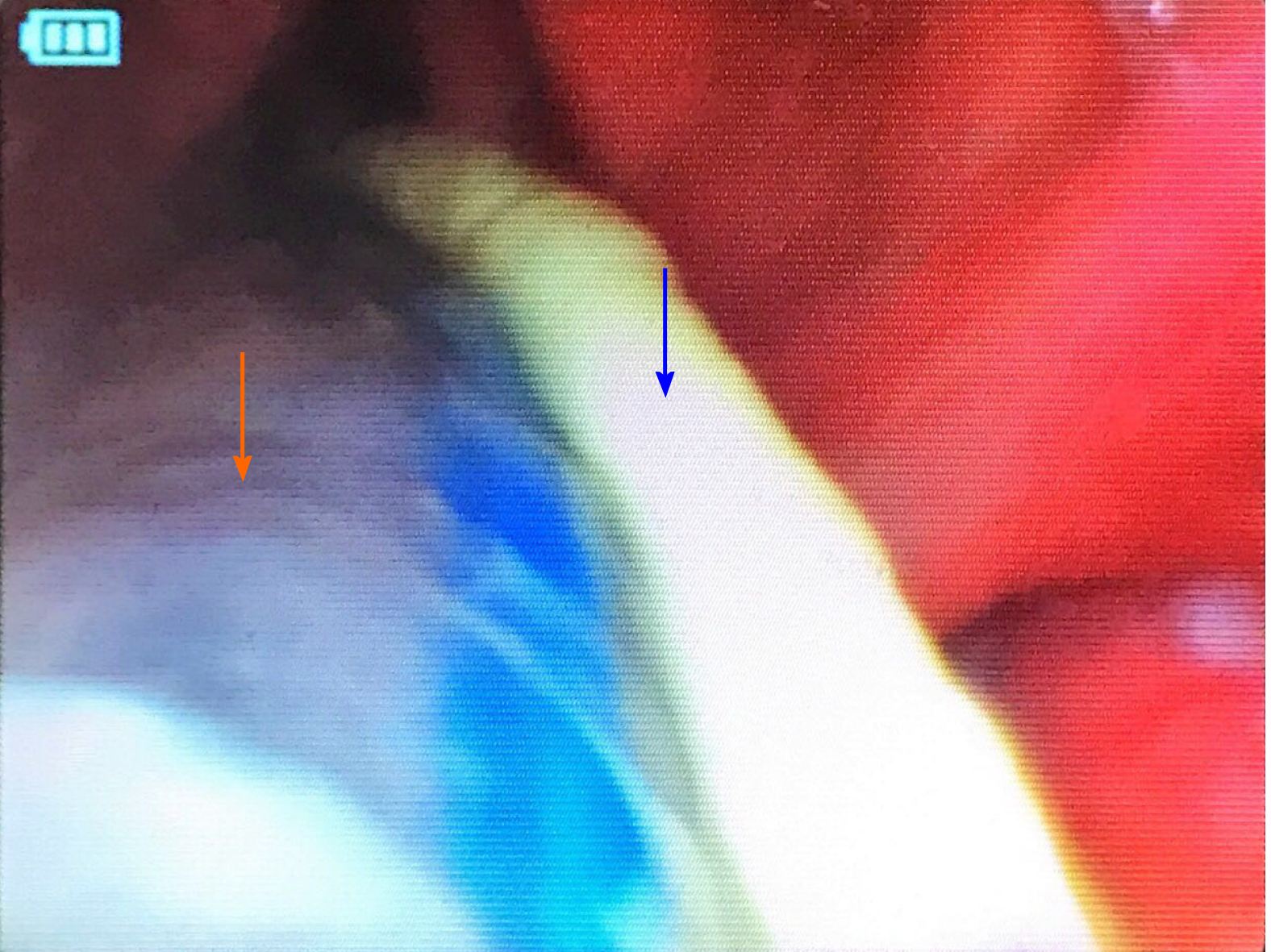
A chest X-ray revealed that the position of the nasoduodenal feeding tube was in the chest (Figure 1A). An abdominal X-ray also made it clear that the nasoduodenal feeding tube was not placed in the abdomen (Figure 1B). Visual laryngoscopy revealed that the tube entered the airway together with the windpipe (Figure 2).
The patient suffered from pneumothorax due to tracheal pleura leakage, which occurred when the feeding tube was immediately removed.
We administered chest drainage in the middle of the clavicle and second ribs.
However, the patient died as a result of the aggravation of the lung infection.
The most commonly used non-invasive method of enteral nutrition is a nasogastrojejunal tube. The jejunal nutrition tube has increasingly been used in clinical practice, and the results in frequent complications[4,5]. The traditional method of intubation depends on the operator experience, X-ray, and gastroscope. Nasogastrojejunal tube insertion based on a minimally invasive catheterization procedure, combined with ultrasound guidance, is becoming more prevalent[6]. The use of bedside ultrasound to guide the placement of the jejunal tube is safe, convenient and economical. One of the common complications of indwelling jejunal tubes is the misplaced airway as reported in this case. How can we avoid it? When the cannula is about 30 cm, we need to observe the patient's response and ventilator condition. Even neck ultrasound determines access to the esophagus. If the patient has a severe cough response or a leak and a high pressure alarm, it may suggest that the tube has entered the airway. When the tube is placed around 50 cm, we need to complete a test of pumping. If you can hear the gas over water (bubble sound), then the catheter head has entered the stomach. If not, the patient should be reintubated.
The complication of blind bedside jejunal feeding tube placement was a disaster. Ultrasound guidance under visualization can avoid serious complications. Practitioners need to pay attention to patient response and the ventilator during catheterization.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical Care Medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Soares RLS S-Editor: Li JH L-Editor: A P-Editor: Li JH
| 1. | Reintam Blaser A, Starkopf J, Alhazzani W, Berger MM, Casaer MP, Deane AM, Fruhwald S, Hiesmayr M, Ichai C, Jakob SM, Loudet CI, Malbrain ML, Montejo González JC, Paugam-Burtz C, Poeze M, Preiser JC, Singer P, van Zanten AR, De Waele J, Wendon J, Wernerman J, Whitehouse T, Wilmer A, Oudemans-van Straaten HM; ESICM Working Group on Gastrointestinal Function. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2017;43:380-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 414] [Article Influence: 59.1] [Reference Citation Analysis (0)] |
| 2. | Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3352] [Cited by in F6Publishing: 3784] [Article Influence: 540.6] [Reference Citation Analysis (0)] |
| 3. | Taylor BE, McClave SA, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C; Society of Critical Care Medicine; American Society of Parenteral and Enteral Nutrition. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016;44:390-438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 347] [Cited by in F6Publishing: 390] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 4. | Fakih HAM, Daouk S, Runnstrom M, Ataya A. A nasoenteral feeding tube barking up the wrong tree. Intensive Care Med. 2017;43:930-931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Stefani A, Ruggiero C, Aramini B, Scamporlino A. An unusual drain in the pleural cavity: iatrogenic pneumothorax due to pulmonary misplacement of a nasogastric tube. Intensive Care Med. 2018;44:2290-2291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Li Y, Ye Y, Mei Y, Ruan H, Yu Y. Semi-automated ultrasound guidance applied to nasogastrojejunal tube replacement for enteral nutrition in critically ill adults. Biomed Eng Online. 2018;17:21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |