Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1291
Peer-review started: July 26, 2021
First decision: October 22, 2021
Revised: November 4, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: February 6, 2022
Processing time: 182 Days and 3.3 Hours
Primary choroidal lymphoma is usually an indolent B-cell lymphoma and rarely progresses to extraocular sites. Herein, we report a case of primary choroidal lymphoma diagnosed as diffuse large B-cell lymphoma (DLBL), which progressed to the brain parenchyma after 4 mo.
A 78-year-old man presented with diminution of vision in his right eye. A choroidal lesion suspected of metastatic lesion was observed in the right eye by ophthalmologic examination. To discover the primary tumor, imaging investigations were performed but no malignant lesion was detected. After 4 mo, the patient returned to the clinic presenting with neurological symptoms. Brain magnetic resonance imaging revealed an abnormal contrast-enhancing mass in the left cerebellum. A stereotactic biopsy was performed, and DLBL was confirmed. The patient received the high dose methotrexate-based chemotherapy and he achieved complete remission.
Primary choroidal lymphoma is usually known to have a benign clinical course without systemic involvement. We present a rare case of primary choroidal lymphoma diagnosed as DLBL that progressed to the brain parenchyma within months.
Core Tip: Primary choroidal lymphoma is a rare subset of primary intraocular lymphoma and shows a benign clinical course with no systemic involvement. Our case report involves a primary choroidal lymphoma demonstrating rare extraocular progression within months.
- Citation: Jang HR, Lim KH, Lee K. Primary central nervous system lymphoma presenting as a single choroidal lesion mimicking metastasis: A case report. World J Clin Cases 2022; 10(4): 1291-1295
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1291.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1291
Primary intraocular lymphoma (PIOL) is a rare subset of primary central nervous system lymphoma (PCNSL) and includes vitreoretinal, choroidal, and iridal lymphomas [1]. Among PIOLs, primary choroidal lymphoma is a very rare disease, and only a small number of cases have been reported in the literature. Previously reported primary choroidal lymphomas were usually low-grade B-cell lymphomas, which rarely progressed to the central nervous system[2,3]. Herein, we report a very rare case of primary choroidal lymphoma diagnosed as diffuse large B-cell lymphoma (DLBL), which initially presented as a unilateral choroidal lesion mimicking metastasis.
A 78-year-old male came to the hospital presenting with a diminution of vision in his right eye.
His blurred vision had been aggravated for several weeks.
The patient had no relevant medical history, such as that of diabetes mellitus or hypertension. In the past, the patient had undergone short-term treatment for occupational pneumoconiosis resulting from his work as a coal miner for > 10 years.
No special history of personal and family.
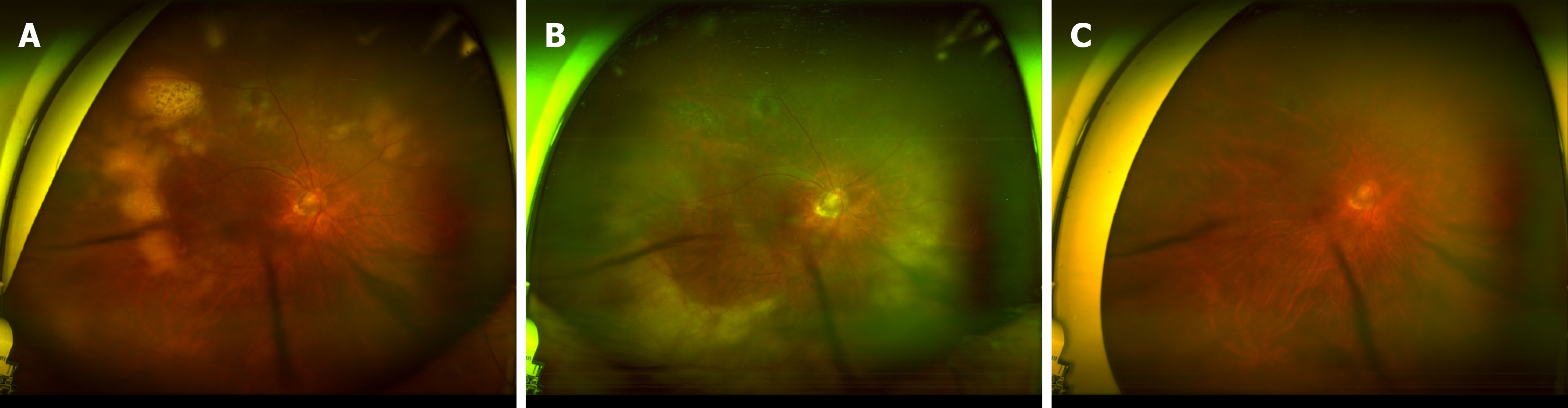
An ophthalmological examination revealed exudative subretinal detachment with a choroidal lesion suspicious of metastasis in the right eye (Figure 1A).
Lactate dehydrogenase was moderately elevated at 387 U/L (normal range: 119-229 U/L).
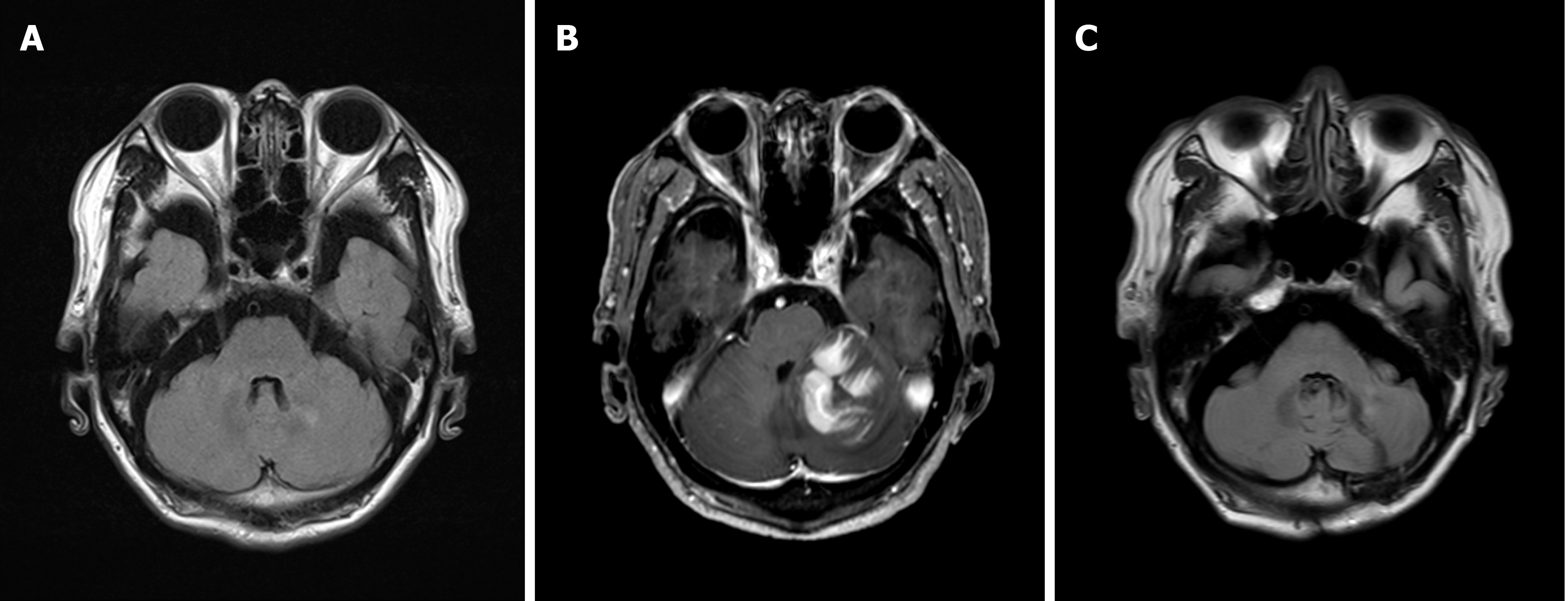
To identify the primary tumor, the patient was referred to the Department of Hemato-oncology at our institute. Brain magnetic resonance imaging (MRI) (Figure 2A) and computed tomography (CT) of the neck, chest, and abdomen-pelvis showed no malignant lesions.
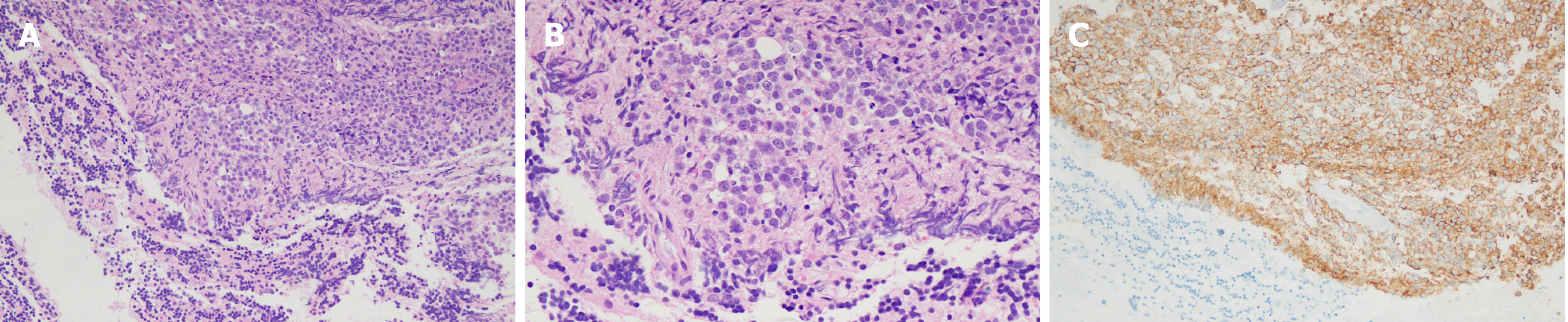
Four months later, the patient revisited the clinic because of dysarthria, headache, and right-sided weakness. No apparent aggravation of visual acuity was observed. The same findings of ophthalmoscopy as at the first visit were confirmed (Figure 1B). Brain MRI showed a single, irregular, contrast-enhancing mass in the left cerebellum (Figure 2B). The patient underwent a stereotactic biopsy of the mass and was diagnosed with DLBL (Figure 3). Further imaging, including CT and positron emission tomography/CT, revealed no systemic involvement. There was no evidence of lymphoma involvement in the cerebrospinal fluid and bone marrow.
The patient received high-dose methotrexate (HD-MTX)-based chemotherapy, which comprised methotrexate (3.5 g/m2), vincristine (1.4 mg/m2, capped at 2 mg), and prednisolone (100 mg/d), with the addition of procarbazine (100 mg/m2) in the first, third, and fifth cycles. Intrathecal injection was not given in this patient because there was no evidence of lymphoma involvement in the CSF test before and after the first cycle of HD-MTX based chemotherapy.
After completing six cycles of HD-MTX-based chemotherapy, the patient’s neur
Intraocular lymphoma is extremely rare and accounts for approximately 1.86% of intraocular malignancies[4]. Intraocular lymphoma is a heterogeneous group of malignancies located in different tissues, including the vitreous, retina, choroid, ciliary body, and iris, within the eye. It also refers to forms of primary or secondary to central nervous system lymphoma or disseminated systemic disease[3,5].
Primary intraocular lymphoma is considered a subset of PCNSL, and it progresses to the central nervous system in 15%-25% of PCNSL cases[3]. Primary vitreoretinal lymphoma is the most common intraocular lymphoma, followed by uveal lymphoma.
Choroidal lymphoma is a subset of uveal lymphoma. It can be subdivided into primary and secondary lymphoma based on the presence of systemic lymphoma at the time of ocular presentation. Primary choroidal lymphomas are defined as the absence of prior systemic lymphomas or concurrent extraocular lymphomas [6]. Several studies have reported clinical differences between primary and secondary choroidal lymphomas[2,7].
Primary choroidal lymphomas are mainly low grade B-cell lymphomas such as extranodal marginal zone B-cell lymphoma, are usually unilateral, and typically do not progress to the central nervous system parenchyma. Secondary choroidal lymphoma is characterized by the presence of previously known cancer or concurrent systemic lymphomas at the initial ocular presentation.
In contrast to primary choroidal lymphomas, secondary choroidal lymphomas are more likely to demonstrate bilateral involvement and preexistent lymphomas. More than half of secondary choroidal lymphomas have been confirmed as high-grade B-cell lymphomas, such as DLBL[2,8].
Unlike the previously reported cases of primary choroidal lymphoma, this case was characterized by the pathological findings of DLBL and disease progression to the brain parenchyma within a few months. In most of the previous cases of primary choroidal lymphoma, management involved local treatment or observation, whereas in our case, HD-MTX-based chemotherapy was administered, and the treatment response was complete remission.
Primary choroidal lymphoma is generally known to have a benign clinical course without systemic involvement. We reported a rare case of primary choroidal lymphoma diagnosed as DLBL, characterized by an aggressive clinical course that progressed to the brain parenchyma within a few months.
The authors thank the Department of Radiology, Kangwon National University Hospital, Kangwon National University School of Medicine.
Provenance and peer review: Unsolicited manuscript; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dou AX, Montemurro N S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Tang LJ, Gu CL, Zhang P. Intraocular lymphoma. Int J Ophthalmol. 2017;10:1301-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Mashayekhi A, Shukla SY, Shields JA, Shields CL. Choroidal lymphoma: clinical features and association with systemic lymphoma. Ophthalmology. 2014;121:342-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Chan CC, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, Cassoux N, Touitou V, Smith JR, Batchelor TT, Pulido JS. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16:1589-1599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 323] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 4. | Reddy EK, Bhatia P, Evans RG. Primary orbital lymphomas. Int J Radiat Oncol Biol Phys. 1988;15:1239-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Konstantinidis L, Damato B. Intraocular Metastases--A Review. Asia Pac J Ophthalmol (Phila). 2017;6:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Coupland SE, Foss HD, Hidayat AA, Cockerham GC, Hummel M, Stein H. Extranodal marginal zone B cell lymphomas of the uvea: an analysis of 13 cases. J Pathol. 2002;197:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Exp Ophthalmol. 2008;36:564-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 207] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 8. | Doycheva D, Zierhut M, Süsskind D, Bartz-Schmidt KU, Deuter C. [Diagnostics and treatment of choroidal lymphoma]. Ophthalmologe. 2015;112:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |