Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13216
Peer-review started: April 26, 2022
First decision: May 30, 2022
Revised: June 9, 2022
Accepted: August 1, 2022
Article in press: August 1, 2022
Published online: December 26, 2022
Processing time: 244 Days and 4.1 Hours
The B.1.617.2 (delta) variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first discovered in Maharashtra in late 2020 and has rapidly expanded across India and worldwide. It took only 2 mo for this variant to spread in Indonesia, making the country the new epicenter of the delta variant as of July 2021. Despite efforts made by accelerating massive rollouts of current vaccines to protect against infection, cases of fully-vaccinated people infected with the delta variant have been reported.
To describe the demographic statistics and clinical presentation of the delta variant infection after the second dose of vaccine in Indonesia.
A retrospective, single-centre case series of the general consecutive population that worked or studied at Faculty of Medicine, Universitas Indonesia with confirmed Delta Variant Infection after a second dose of vaccine from 24 June and 25 June 2021. Cases were collected retrospectively based on a combination of author recall, reverse transcription-polymerase chain reaction (RT-PCR), and whole genome sequencing results from the Clinical Microbiology Laboratory, Faculty of Medicine, Universitas Indonesia.
Between 24 June and 25 June 2021, 15 subjects were confirmed with the B.1.617.2 (delta) variant infection after a second dose of the vaccine. Fourteen subjects were vaccinated with CoronaVac (Sinovac) and one subject with ChAdOx1 nCoV-19 (Oxford-AstraZeneca). All of the subjects remained in home isolation, with fever being the most common symptom at the onset of illness
Although this case shows that after two doses of vaccine, subjects are still susceptible to the delta variant infection, currently available vaccines remain the most effective protection. They reduce clinical manifestations of COVID-19, decrease recovery time from the first positive swab to negative swab, and lower the probability of hospitalization and mortality rate compared to unvaccinated individuals.
Core Tip: The emergence of the B.1.617.2 (delta) variant has been attributed to an unexpected increase in coronavirus disease 2019 cases. This variant exhibits a high transmission rate and presents evidence of a more severe disease. Despite efforts made by accelerating massive rollouts of current vaccines and increasing vaccination doses, this delta variant has quickly spread in various countries. Two months after it spread through India, Indonesia has become the new epicenter of the delta variant. Therefore, the effectiveness of currently available vaccines in Indonesia has remained unknown because fully-vaccinated individuals have been infected with the delta variant.
- Citation: Karuniawati A, Syam AF, Achmadsyah A, Ibrahim F, Rosa Y, Sudarmono P, Fadilah F, Rasmin M. Case series in Indonesia: B.1.617.2 (delta) variant of SARS-CoV-2 infection after a second dose of vaccine. World J Clin Cases 2022; 10(36): 13216-13226
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13216.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13216
For nearly 2 years, the coronavirus disease 2019 (COVID-19) pandemic has been a major issue in human global health. In early March 2021, there were 116 million cases of infection worldwide, with 2.6 million global deaths. There was only modest genetic evolution at the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, mainly because of the global lack of immunity against this new pathogen[1]. In December 2020, the emergence of new SARS-CoV-2 variants was attributed to an unexpected increase in COVID-19 cases[2]. These new variants are the result of the remarkable capacity of RNA viruses to adapt to new hosts and environments[3]. They are able to develop a high number of mutations, mainly in the S protein, causing potential harm to human health.
The World Health Organization (WHO) has classified SARS-CoV-2 variants into two categories: variants of concern (VOC) and variants of interest[1]. VOC is a term that has been used by the WHO to describe SARS-CoV-2 variants that exhibit a high transmission rate in the context of high population immunity, evidence of a more severe disease, and reduced effectiveness of vaccines[2]. For example, the B.1.617.2 (delta) variant of SARS-CoV-2 was first discovered in Maharashtra in late 2020 and has rapidly expanded across India and worldwide, outcompeting other lineages, such as the B.1.617.1 (kappa) and B.1.1.7 (alpha) variants. This delta variant is six-fold less sensitive to serum neutralizing antibodies from a recovered individual, and eight-fold less sensitive to vaccine-elicited antibodies in vitro[4].
A key issue has surfaced of whether currently available COVID-19 vaccines are able to protect against infection of the new delta variant. A total of 19 current SARS-CoV-2 vaccines worldwide are based on the original strains. With the newly emerging variants, scientists have been challenged to establish response strategies to control the SARS-CoV-2 pandemic[1,5].
Despite efforts made by accelerating massive rollouts of current vaccines and increasing vaccine immunogenicity by increasing vaccination doses, the delta variant of COVID-19 has quickly spread in various countries such as Bangladesh, Iran, Iraq, Malaysia, Myanmar, South Korea, Japan, and Indonesia[5,6]. Two months after spreading through India, Indonesia has become the new epicenter of the delta variant as of July 2021, where only 5.5% of its citizens have been fully vaccinated. As of 15 July 2021, Indonesia had 56.767 new cases, with a test positivity rate of 26%, indicating that large numbers of cases are being missed, and reporting an average of 919 deaths a day over the past week[6]. The effectiveness of currently available vaccines in Indonesia, namely CoronaVac (Sinovac), BNT162b2 (Pfizer-BioNTech), and ChAdOx1 nCoV-19 (Oxford-AstraZeneca), has remained unknown because fully-vaccinated individuals have been infected with the B.1.617.2 (delta) variant[7].
Here, we report a case series describing the demographic statistics and clinical presentation of the first cluster of delta variant infection after a second dose of vaccine.
This study included patients who tested positive for the B.1.617.2 (delta) variant between 24 June and 25 June 2021 (based on data http://www.gisaid.org). The SARS-CoV-2 variant was collected retrospec
Subject data are presented as absolute values, percentages, mean ± SD, or median using SPSS 26 (IBM Corp, Armonk, NY, United States). Continuous and discrete variables are expressed as the mean ± SD or median depending on the results of the normality test. Categorical variables are expressed as n (%).
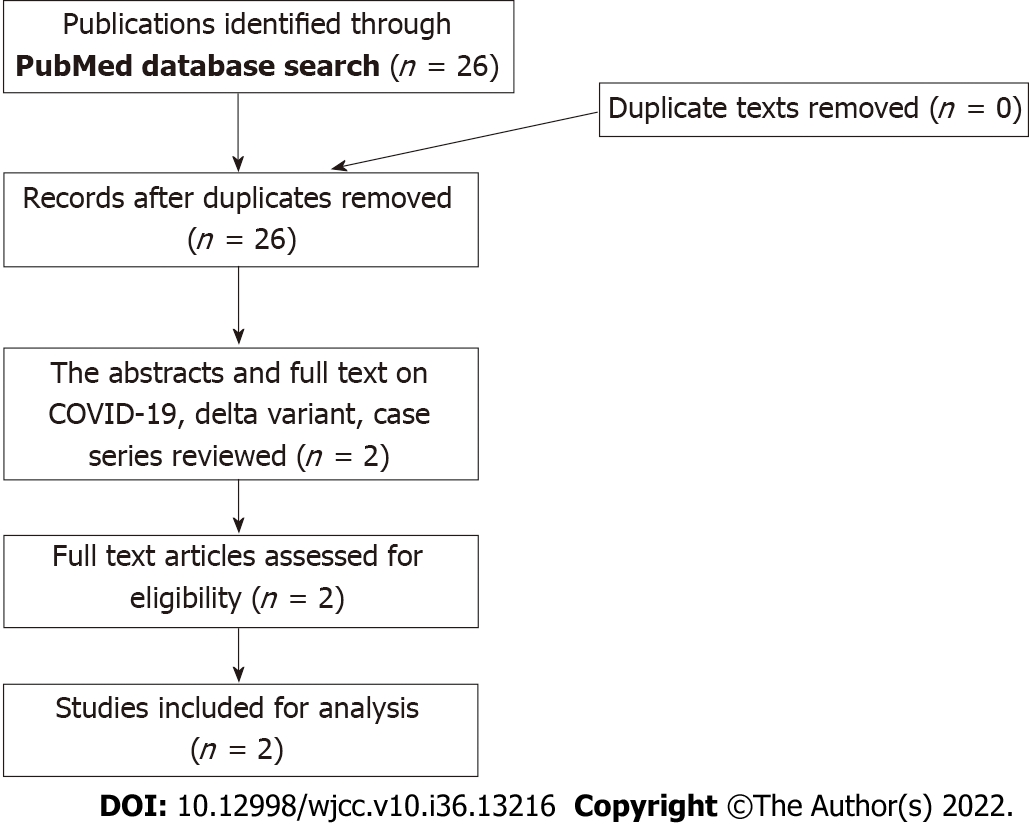
Sources: A comprehensive search of PubMed was performed for all studies published prior from March 2020 to April 2022, using the search terms “COVID-19”, “Delta Variant OR B.1.617.2 Variant” , “Fully vaccinated OR Full-Dose Vaccine”, and “Case Series” which yielded 26 results (Figure 1). A systematic review of these papers were performed, and after the full text of all articles were evaluated to determine whether results were included. There were no language restrictions. Two results were used for our paper (Table 1).
| Ref. | Publication date | Journal | Sample size | Subjects | Limitations |
| Park et al[22] | January 4, 2022 | Clinical Infection Disease | 108 | Delta Variant | Statistic of fully vaccinated sample not included, sample from different ethnic |
| Hu et al[23] | March 1, 2022 | Frontiers in Medicine | 156 | Delta Variant Fully Vaccinated | Sample from different ethnic |
We described the first 15 subjects with the B.1.617.2 (delta) variant SARS-CoV-2 collected from nasopharyngeal swabs between 24 and 25 June 2021 at the Clinical Microbiology Laboratory Universitas Indonesia. Table 2 shows the demographic statistics of the subjects enrolled. The mean age of the subjects was 29 years (± 5.097), and 10 were males. Of the 15 subjects, 2 (13.34%) had one or more coexisting medical conditions: chronic respiratory disease in 1, and obesity with a history of rhinitis allergy in 1. The mean body mass index (BMI) of subjects was 24.768 kg/m2 (± 3.531), which was statistically in a normal category according to the WHO and overweight at risk according to the Asian-Pacific BMI with a mean height of 167.00 cm (± 8.384) and a mean weight of 69.20 kg (± 11.706)[8]. Subjects were primarily employees working at Universitas Indonesia and included a total of 11 (73.34%) employees, 1 (6.67%) medical student, and 3 (20%) residents. Of the 15 subjects, 14 (93.34%) were vaccinated with CoronaVac (Sinovac), which was widely available in the first phase of vaccination in Indonesia.
| Demographic factor | All | |
| Subjects, n | 15 | |
| Age class, n (%) | ||
| 21-25 | 3 (20) | |
| 26-30 | 5 (33.34) | |
| 31-35 | 4 (26.67) | |
| 35-40 | 3 (20) | |
| Age in yr, mean ± SD | 29.87 ± 5.097 | |
| Sex | ||
| Male | 10 (66.67) | |
| Female | 5 (33.33) | |
| Height in cm, mean ± SD | 167.00 ± 8.384 | |
| Weight in kg, mean ± SD | 69.20 ± 11.706 | |
| Body mass index as kg/m2, mean ± SD | 24.768 ± 3.531 | |
| Occupation, n (%) | ||
| Employee | 11 (73.34) | |
| Medical students | 1 (6.67) | |
| Residents | 3 (20) | |
| Comorbidity, n (%) | 2 (13.34) | |
| Chronic respiratory disease | 1 (6.67) | |
| Obesity | 1 (6.67) | |
| Vaccination type, n (%) | ||
| CoronaVac (Sinovac) | 14 (93.34) | |
| ChAdOx1 nCoV-19 (Oxford-AstraZeneca) | 1 (6.67) | |
Table 3 shows the clinical characteristics of the subjects included in this case series. Of the 15 subjects enrolled, 1 (6.67%) was reinfected. The first infection occurred before the patient had the first vaccination, and reinfection occurred after the second dose of vaccine. Most subjects (7, 46.67%) were thought to be infected by their coworkers, followed by family in 3 (20%), patients in 3 (20%), and unknown sources in 2 (13.34%). Eleven subjects (73.34%) used a surgical mask during work and daily activity, three (20%) used an N95 mask, and one (6.67%) used a KN95 mask.
| Characteristic | All | |
| Reinfection, n (%) | 1 (6.67) | |
| Predicted source of infection, n (%) | ||
| Family | 3 (20) | |
| Patient | 3 (20) | |
| Coworker | 7 (46.67) | |
| Unknown | 2 (13.34) | |
| Mask usage during outside activity, n (%) | ||
| Surgical mask | 11 (73.34) | |
| N95 mask | 3 (20) | |
| KN95 mask | 1 (6.67) | |
| Symptoms, n (%) | ||
| Fever | 10 (66.67) | |
| Cough | 7 (46.67) | |
| Rhinorrhea | 9 (60) | |
| Headache | 5 (33.34) | |
| Sore throat | 2 (13.34) | |
| Anosmia | 8 (53.34) | |
| Ageusia/Dysgeusia | 4 (26.67) | |
| Diarrhea | 3 (20) | |
| Fatigue | 4 (26.67) | |
| Myalgia | 4 (26.67) | |
| Dyspnea | 1 (6.67) | |
| Nausea | 1 (6.67) | |
| Time in d of symptom duration, mean ± SD | 7.73 ± 5.444 | |
| Time in d of PCR conversion, mean ± SD | 17.93 ± 6.364 | |
| Time in d that elapsed from second dose of vaccine to a positive PCR result, median IQR | 87 (86-128.00) | |
| In-home isolation, n (%) | 15 (100) | |
| Drug treatment, n (%) | ||
| Vitamin C | 14 (93.34) | |
| Vitamin D | 12 (80) | |
| Paracetamol | 8 (53.34) | |
| Azithromycin | 5 (33.34) | |
| Oseltamivir | 1 (6.67) | |
| Favipiravir | 3 (20) | |
| Phytopharmaca | 1 (6.67) | |
Of the 15 subjects enrolled, 1 (6.67%) was asymptomatic and 14 (93.34%) were symptomatic. Among the symptomatic patients, the most common symptoms at the onset of illness were fever (10, 66.67%), defined as an axillary temperature of 37.5 °C or higher, rhinorrhea (9, 60%), anosmia (8, 53.34%), cough (7, 46.67%), headache (5, 33.34%), ageusia/dysgeusia (4, 26.67%), fatigue (4, 26.67%), myalgia (4, 26.67%), diarrhea (3, 20%), sore throat (2, 13.34%), dyspnea (1, 6.67%), and nausea (1, 6.67%). All of the subjects were in home isolation. The mean time for symptom duration was 7.73 d (± 5.444). The mean time from the first positive swab to a negative RT-PCR test for SARS-CoV-2 was 17.93 d (± 6.3464). The median time that elapsed from the second dose of vaccine to the first positive swab was 87 d [interquartile range (IQR): 86-128 d].
Each of the 15 subjects received pharmacological treatment. Vitamin C was used in 14 subjects (93.34%), vitamin D in 12 (80%), paracetamol in 8 (53.34%), azithromycin in 5 (33.34%), favipiravir in 3 (20%), oseltamivir in 1 (6.67%), and phytopharmaca (Andrographis paniculata, known as Sambiloto in Indonesia) in 1 (6.67%).
In this case series, we reported 15 subjects with confirmed infection with the B.1.617.2 (delta) variant of SARS-CoV-2 after a second dose of vaccine. From the statistics acquired, men are more prone to SARS-CoV-2 infection. Angiotensin-converting enzyme 2 (ACE2) is expressed in various human tissues. The expression levels are not significantly different between males and females, between young and old persons, nor among races, indicating that SARS-CoV-2 may equally infect persons of different sexes, ages, and races. The different host immune responses to infection may explain why males vs females and young vs old person persons infected with SARS-CoV-2 have distinct disease severity. Studies have found that the X chromosome and sex hormones play important roles in innate and adaptive immunity, which makes women less susceptible to viral infection[9]. Age also plays a key factor, as the body’s immunity declines with age. Aging has been linked to abnormally high cellular functioning, cellular hyperfunctions that may eventually lead to cellular exhaustion, and function loss in later stages[10]. However, in this case series, the subjects were of productive age (15-64 years), with a mean age of 29 years (± 5.097)[11]. Subjects with underlying diseases such as diabetes, hypertension, cardiovascular disease, chronic respiratory disease, and obesity also have increased risk of SARS-CoV-2 infection. A long-term history of diabetes, hypertension, and cardiovascular disease damages the vascular structure and is more likely to reduce the body’s immunity. When a subject has previous respiratory diseases that damaged their lung function such as lung tuberculosis or chronic obstructive pulmonary disease, they have lower resistance to the virus and are prone to developing acute respiratory distress syndrome[9]. Obesity or excess ectopic fat deposition may also be a unifying risk factor for SARS-CoV-2 infection, as it reduces protective cardiorespiratory reserve as well as potentiates the immune dysregulation that appears to mediate the progression to critical illness[12]. In this case series, 1 subject had a history of lung tuberculosis (6.67%) and 1 subject (6.67%) was obese according to the WHO BMI. However, the Asia-Pacific BMI has stated that BMI between 23.0 and 24.9 is considered overweight, which makes the subject in this case series more susceptible to SARS-CoV-2 infection, as the mean BMI was 24.768 kg/m2 (± 3.531)[9,12].
Of the 15 subjects, 14 individuals (93.34%) were confirmed to have a second dose of CoronaVac (Sinovac) and 1 individual (6.67%) had a second dose of ChAdOx1 nCoV-19 (Oxford-AstraZeneca). Both vaccines are widely available in Indonesia, as other vaccines such as BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna) have not arrived. According to a study in China, the vaccine effectiveness (VE) of two doses of CoronaVac was 59.0% (95%CI: 16.0%-81.6%) against the delta variant infection. However, a single dose vaccine of CoronaVac was not sufficiently protective against the delta variant[13]. However, ChAdOx1 nCoV-19 (Oxford-AstraZeneca) and BNT162b2 (Pfizer-BioNTech) vaccines had higher VE rates compared to CoronaVac (Sinovac). It has been reported that the VE after the second dose of Oxford-AstraZeneca vaccine is 67.0% (95%CI: 61.3%-71.8%) and 88.0% (95%CI: 85.3%-90.1%) with Pfizer-BioNTech. A single dose of Oxford-AstraZeneca or Pfizer-BioNTech vaccine was notably lower among people with the delta variant (30.55; 95%CI: 25.2%-35.7%)[14].
WGS data of the samples showed that the most common mutations found in the S protein domains were L452R, T478K, D614G, and P681R, which might affect the sensitivity in neutralizing monoclonal antibodies[15]. Research has shown that the L452R mutation can cause a decrease in the titer of vaccine-induced serum neutralizing antibody against the pseudovirus and recognition by antibodies while maintaining binding to ACE2[16]. P681R and D614G mutations also cause a partial decrease in neutralizing antibodies. A study by Saito et al[18] showed that the neutralizing antibodies of immune serum induced by BNT162b2 vaccine against D614G/P681R virus was significantly decreased[18]. The T478K mutation also exhibited a reduction in its neutralization sensitivity towards the post-vaccination sera. This phenomenon might explain the incidence of infection in vaccinated subjects.
From this case series, there was 1 subject (6.67%) who had been diagnosed twice with SARS-CoV-2 infection, before vaccination and after two doses of vaccine. A study by Altawalah[19] showed that the immune responses induced by COVID-19 vaccination are greater than those induced by natural SARS-CoV-2 infection. Therefore, individuals that have recovered from a confirmed COVID-19 infection are still prone to another reinfection. A study by Ebinger et al[20] also showed that the anti-S immunoglobulin G antibody response following a single vaccine dose in people who have recovered from confirmed prior COVID-19 infection is comparable to the antibody reaction following two doses of vaccine in people who have never been infected (P > 0.58). Thus, individuals who once had confirmed COVID-19 infection and also had a double dose regimen are expected to have better immunity against COVID-19. Reinfection in this case still remained unclear, but age, sex, and underlying diseases such as obesity, chronic respiratory disease, and cardiovascular disease could be independent risk factors that contribute to susceptibility to viral infection[10].
According to a study by Das et al[21], different types of masks have different effectiveness in protecting subjects against SARS-CoV-2. A surgical face mask has the lowest filtration rate of 60%-80% and can filter particles as small as 0.3 μm. The N95 face mask has the highest filtration rate (95%) compared to the other two; it can filter particles of 0.1-0.3 μm in size. The KN95 face mask has an 80%-95% filtration rate and can filter particles down to 0.3 μm. Since SARS-CoV-2 is a 0.1 μm enveloped virus, the N95 mask has a better probability of protecting against COVID-19 infection[21]. The current study showed that 11 (73.34%) of the 15 subjects who tested positive for COVID-19 were using surgical masks for daily usage. The correct use of N95/KN95 masks requires a fit test or seal test, which is sometimes not done properly. It was also noted that masks were used during their daily activities, and no subject had performed an aerosol-generating procedure before infection with COVID-19.
The common clinical manifestations of COVID-19 patients in this case series were fever in 10 (66.67%), rhinorrhea in 9 (60%), anosmia in 8 (53.34%), and cough in 7 (46.67%). A recent study by Park et al[22], also strengthen our findings, from a total of 108 delta variant subjects that were enrolled, common symptoms for the delta variant are fever (73.7%), myalgia (51.5%), cough (49.5%), sore throat (43.4%), and cephalgia (34.3%). In comparison, Myalgia was more common in the delta group (51.5%) than in the non-delta group (26.9%). Non-delta variant also showed significant symptoms of loss of taste (26.9%) and loss of smell (15.4%) compare to delta group with loss of taste (2.0%) and loss of smell (7.1%)[22]. Another study by Hu et al[23] with 156 full vaccinated delta variant patients that admitted at Yangzhou, China in 2021 also indicate that most common symptoms are cough (48.7%), fever (34.6%), sore throat (25.6%), fatigue (19.2%), and expectoration (8.3%). Another study also showed that between delta variant and alpha variant are quite similar, except patients with delta variant could become rapidly ill and have higher viral loads in the respiratory tract. Delta variant could also cause auditory impairment and gangrene from worse blood clots[24]. Viral infection triggers an inflammatory pathway in the human body. Various inflammatory factors produced by the inflammatory storm can cause systemic immune damage and manifest as high temperatures. It explains why the most common symptom was fever. SARS-CoV-2 also binds to the ACE2 receptor, which is mainly distributed in the respiratory tract, cardiovascular, kidneys, and colon. It causes multiple symptoms, such as dyspnea, cough, anosmia, ageusia, diarrhea, and sore throat[9] (Table 4).
| Our study (n = 15) | Park et al[22] (n = 108) | Hu et al[23] (n = 156) | |
| Age | 29.87 ± 5.097 | 34.5 (26.5-46.0) | 43.0 (33.0-56.8) |
| Comorbidity | |||
| Hypertension | 12 (11.1) | 31 (19.9) | |
| Hyperlipidaemia | 4 (3.7) | ||
| Diabetes | 7 (6.5) | 9 (5.8) | |
| Psychiatric illness | 1(0.9) | ||
| Cancer | 1 (0.9) | ||
| Obesity (BMI > 30) | 1 (6.67) | 12 (11.1) | |
| Cardiovascular disease | 5 (3.2) | ||
| Respiratory disease | 1 (6.67) | ||
| Symptoms | |||
| Fever | 10 (66.67) | 73 (73.7) | 54 (34.6) |
| Cough | 7 (46.67) | 49 (49.5) | 76 (48.7) |
| Rhinorrhoea | 9 (60) | 4 (4.0) | |
| Headache | 5 (33.34) | 34 (34.3) | |
| Sore throat | 2 (13.34) | 43 (43.4) | 40 (25.6) |
| Anosmia | 8 (53.34) | 7 (7.1) | |
| Ageusia/dysgeusia | 4 (26.67) | 2 (2.0) | |
| Diarrhoea | 3 (20) | 3 (3.0) | 14 (9.0) |
| Fatigue | 4 (26.67) | 30 (19.2) | |
| Myalgia | 4 (26.67) | ||
| Dyspnoea | 1 (6.67) | 1 (1.0) | 1 (0.6) |
| Nausea | 1 (6.67) |
Although subjects with two-dose vaccination can still be infected with SARS-CoV-2, the results from a current trial suggest that there is a 90% reduction in symptomatic COVID-19 with vaccine. However, it remains unknown whether this efficacy is mediated by decreasing SARS-CoV-2 infection susceptibility (VESUSC) or the development of symptoms after infection (VESYMP)[25]. In our case series, symptoms that developed in COVID-19 patients were mild to moderate according to the Indonesian COVID-19 Guideline. In addition, vaccination decreased the symptom duration of COVID-19 patients (7.73 ± 5.444 d), increased the recovery time from the first positive swab to negative swab (17.93 ± 6.364 d), and prevented the subjects from needing hospitalization. A recent study revealed that VE in terms of protection against deaths was 72%, with a lower reduction of mortality for B.1.1.7 vs non-B.1.1.7 variants (70% vs 78%, respectively)[26]. A study from a hospital in New Delhi, India showed that among those fully vaccinated, there was 12.5% (23/184) mortality compared to 31.45% (309/984) among the unvaccinated (OR = 0.3, 95%CI: 0.2-0.5; P < 0.0001)[27].
The most common drugs used in our case series were vitamin C (14 subjects, 93.34%) and vitamin D (12 subjects, 80%). Low levels of micronutrients have been associated with adverse clinical outcomes during SARS-CoV-2 infection. As a result, daily vitamin intake may be beneficial in maximizing the immune response to viral infection. Recent studies have shown that vitamin D improves the physical barrier against viruses and stimulates the production of antimicrobial peptides. It may also prevent cytokine storm by lowering the production of inflammatory cytokines. Vitamin C is considered an antiviral agent as it increases immunity. It also increases antiviral cytokines and free radical formation, lowering viral yield and attenuating excessive inflammatory responses and hyperactivation of immune cells[28]. However, the effectiveness of vitamin C and vitamin D against the B.1.617.2 (delta) variant remain unknown. In this study, 1 subject had consumed Andrographis paniculata as phytopharmaca. According to current studies, Andrographis paniculatecan act as a potential inhibitor of the main protease of SARS-CoV-2, but further studies should be considered[29].
This study had some limitations. First, due to the mandatory WGS results, there were limitations in the subjects included. Thus, the case series might not be representative of the general population and extrapolation to other settings should be done with caution. Second, the data were collected using a questionnaire filled out by the patients themselves, which may have led to bias. Finally, due to regulations, the RT-PCR test was not performed daily. Duration of conversion was considered the time from the first positive swab until the first negative result. It is possible that a patient had a negative result before RT-PCR was conducted (Table 5).
| Ref. | Reasons(s) for gap | Population | Results | Free text of gap |
| Park et al[22] | D | Delta variant | A total of 141 patients [Delta group, n = 108 (77%); non-Delta group, n = 33 (23%)]; Delta group: Median age 34.5 (26.5-46.0); Hypertension 12 (11.1); Hyperlidemia 2 (6.1); Diabetes 5 (15.2); Psychiatric Illness 1(3.0); Asthma/Rhinitis 1 (3.0); Cancer 1 (3.0); Obesity BMI > 30.4 (12.1) | Results may not be applicable for reference as full vaccinated criteria not included and our subject only had chronic respiratory disease 1 (6.67) and obesity 1 (6.67) |
| Hu et al[23] | D | Delta variant fully vaccinated | A total of 677 patients (Wild type = 341; Delta unvaccinated = 120; Delta Partially vaccinated = 60; Delta fully vaccinated = 156); Delta fully vaccinated: Median age 43.0 (33.0-56.8); Hypertension 31 (19.9); Diabetes 9 (5.8); Cardiovascular disease 5 (3.2) | Results may not be applicable for reference as median age in our subject 29.87 ± 5.097 with comorbidity chronic respiratory disease 1 (6.67) and obesity 1 (6.67) |
This case series highlights that the currently available treatment for the B.1.617.2 (delta) variant of SARS-CoV-2 infection is still unknown. Further studies and research should be conducted. Although this case shows that after two doses of vaccine, subjects are still susceptible to the B.1.617.2 (delta) variant, currently available vaccines remain the most effective protection. They reduce the clinical manifestations of COVID-19, decrease the recovery time from first positive swab to negative swab, and lower the probability of hospitalization and mortality rate compared to unvaccinated individuals. We should also support efforts to maximize vaccine uptake with two doses among vulnerable populations to protect them against the B.1.617.2 (delta) variant.
The delta variant of coronavirus disease 2019 (COVID-19) has quickly spread around the globe and infected not only unvaccinated population but fully vaccinated citizens. The demographic statistics and clinical presentation of the first cluster of delta variant infection in this population remained unknown and neglected.
The authors aimed to provide an insight into the demographic statistics and clinical presentation of the first cluster of delta variant infection after a second dose of vaccine. This could help others with lack of laboratory facility to diagnose delta variant infection.
The objective of this case series was to describe the demographic statistics and clinical presentation of the first cluster of delta variant infection after a second dose of vaccine.
This is a retrospective, single-center case series of the general consecutive population that worked or studied in Our University with confirmed Delta Variant Infection after a second dose of vaccine from 24 June and 25 June 2021. We decided to collect data based on a combination of author recall, reverse transcription-polymerase chain reaction (RT-PCR), and whole genome sequencing results. Epidemiological, demographic, clinical, and laboratory data were analyzed.
Among 15 subjects recruited, Fourteen subjects were vaccinated with CoronaVac (Sinovac) and one subject with ChAdOx1 nCoV-19 (Oxford-AstraZeneca). All of the subjects remained in home isolation, with fever being the most common symptom at the onset of illness (n = 10, 66.67%). The mean duration of symptoms was 7.73 d (± 5.444). The mean time that elapsed from the first positive swab to a negative RT-PCR test for SARS-CoV-2 was 17.93 d (± 6.3464). The median time that elapsed from the second dose of vaccine to the first positive swab was 87 d (interquartile range: 86-128).
After two doses of vaccine, subjects are still susceptible to the delta variant infection. Currently available vaccines remain the most effective protection.
The case series might not be representative of the general population. It is necessary to collect more subjects infected with delta variant after second dose of vaccination to improve the quality of this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Indonesian Society of Gastroenterology.
Specialty type: Infectious diseases
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dey J, India; Ramesh PV, India S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Gómez CE, Perdiguero B, Esteban M. Emerging SARS-CoV-2 Variants and Impact in Global Vaccination Programs against SARS-CoV-2/COVID-19. Vaccines (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 184] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 2. | Fontanet A, Autran B, Lina B, Kieny MP, Karim SSA, Sridhar D. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021;397:952-954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 440] [Cited by in RCA: 368] [Article Influence: 92.0] [Reference Citation Analysis (0)] |
| 3. | Sanjuán R, Domingo-Calap P. Mechanisms of viral mutation. Cell Mol Life Sci. 2016;73:4433-4448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 621] [Cited by in RCA: 535] [Article Influence: 59.4] [Reference Citation Analysis (68)] |
| 4. | Mlcochova P, Kemp SA, Dhar MS, Papa G, Meng B, Ferreira IATM, Datir R, Collier DA, Albecka A, Singh S, Pandey R, Brown J, Zhou J, Goonawardane N, Mishra S, Whittaker C, Mellan T, Marwal R, Datta M, Sengupta S, Ponnusamy K, Radhakrishnan VS, Abdullahi A, Charles O, Chattopadhyay P, Devi P, Caputo D, Peacock T, Wattal C, Goel N, Satwik A, Vaishya R, Agarwal M; Indian SARS-CoV-2 Genomics Consortium (INSACOG); Genotype to Phenotype Japan (G2P-Japan) Consortium; CITIID-NIHR BioResource COVID-19 Collaboration, Mavousian A, Lee JH, Bassi J, Silacci-Fegni C, Saliba C, Pinto D, Irie T, Yoshida I, Hamilton WL, Sato K, Bhatt S, Flaxman S, James LC, Corti D, Piccoli L, Barclay WS, Rakshit P, Agrawal A, Gupta RK. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature. 2021;599:114-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 952] [Cited by in RCA: 928] [Article Influence: 232.0] [Reference Citation Analysis (0)] |
| 5. | Bian L, Gao F, Zhang J, He Q, Mao Q, Xu M, Liang Z. Effects of SARS-CoV-2 variants on vaccine efficacy and response strategies. Expert Rev Vaccines. 2021;20:365-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 117] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 6. | Dyer O. Covid-19: Indonesia becomes Asia's new pandemic epicentre as delta variant spreads. BMJ. 2021;374:n1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Farinholt T, Doddapaneni H, Qin X, Menon V, Meng Q, Metcalf G, Chao H, Gingras MC, Avadhanula V, Farinholt P, Agrawal C, Muzny DM, Piedra PA, Gibbs RA, Petrosino J. Transmission event of SARS-CoV-2 delta variant reveals multiple vaccine breakthrough infections. BMC Med. 2021;19:255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 126] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 8. | Lim JU, Lee JH, Kim JS, Hwang YI, Kim TH, Lim SY, Yoo KH, Jung KS, Kim YK, Rhee CK. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:2465-2475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 329] [Cited by in RCA: 262] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 9. | Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, Li Q, Jiang C, Zhou Y, Liu S, Ye C, Zhang P, Xing Y, Guo H, Tang W. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020;81:e16-e25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1186] [Cited by in RCA: 1464] [Article Influence: 292.8] [Reference Citation Analysis (0)] |
| 10. | Hu K, Lin L, Liang Y, Shao X, Hu Z, Luo H, Lei M. COVID-19: risk factors for severe cases of the Delta variant. Aging (Albany NY). 2021;13:23459-23470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Romero Starke K, Petereit-Haack G, Schubert M, Kämpf D, Schliebner A, Hegewald J, Seidler A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 12. | Sattar N, McInnes IB, McMurray JJV. Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms. Circulation. 2020;142:4-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 486] [Article Influence: 97.2] [Reference Citation Analysis (0)] |
| 13. | Li XN, Huang Y, Wang W, Jing QL, Zhang CH, Qin PZ, Guan WJ, Gan L, Li YL, Liu WH, Dong H, Miao YT, Fan SJ, Zhang ZB, Zhang DM, Zhong NS. Effectiveness of inactivated SARS-CoV-2 vaccines against the Delta variant infection in Guangzhou: a test-negative case-control real-world study. Emerg Microbes Infect. 2021;10:1751-1759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 177] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 14. | Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, Stowe J, Tessier E, Groves N, Dabrera G, Myers R, Campbell CNJ, Amirthalingam G, Edmunds M, Zambon M, Brown KE, Hopkins S, Chand M, Ramsay M. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med. 2021;385:585-594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2223] [Cited by in RCA: 1888] [Article Influence: 472.0] [Reference Citation Analysis (0)] |
| 15. | Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, Planchais C, Porrot F, Robillard N, Puech J, Prot M, Gallais F, Gantner P, Velay A, Le Guen J, Kassis-Chikhani N, Edriss D, Belec L, Seve A, Courtellemont L, Péré H, Hocqueloux L, Fafi-Kremer S, Prazuck T, Mouquet H, Bruel T, Simon-Lorière E, Rey FA, Schwartz O. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021;596:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1091] [Cited by in RCA: 1490] [Article Influence: 372.5] [Reference Citation Analysis (0)] |
| 16. | Bian L, Gao Q, Gao F, Wang Q, He Q, Wu X, Mao Q, Xu M, Liang Z. Impact of the Delta variant on vaccine efficacy and response strategies. Expert Rev Vaccines. 2021;20:1201-1209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 152] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 17. | Kuzmina A, Wattad S, Khalaila Y, Ottolenghi A, Rosental B, Engel S, Rosenberg E, Taube R. SARS CoV-2 Delta variant exhibits enhanced infectivity and a minor decrease in neutralization sensitivity to convalescent or post-vaccination sera. iScience. 2021;24:103467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Saito A, Irie T, Suzuki R, Maemura T, Nasser H, Uriu K, Kosugi Y, Shirakawa K, Sadamasu K, Kimura I, Ito J, Wu J, Iwatsuki-Horimoto K, Ito M, Yamayoshi S, Loeber S, Tsuda M, Wang L, Ozono S, Butlertanaka EP, Tanaka YL, Shimizu R, Shimizu K, Yoshimatsu K, Kawabata R, Sakaguchi T, Tokunaga K, Yoshida I, Asakura H, Nagashima M, Kazuma Y, Nomura R, Horisawa Y, Yoshimura K, Takaori-Kondo A, Imai M; Genotype to Phenotype Japan (G2P-Japan) Consortium, Tanaka S, Nakagawa S, Ikeda T, Fukuhara T, Kawaoka Y, Sato K. Enhanced fusogenicity and pathogenicity of SARS-CoV-2 Delta P681R mutation. Nature. 2022;602:300-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 420] [Article Influence: 140.0] [Reference Citation Analysis (0)] |
| 19. | Altawalah H. Antibody Responses to Natural SARS-CoV-2 Infection or after COVID-19 Vaccination. Vaccines (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 20. | Ebinger JE, Fert-Bober J, Printsev I, Wu M, Sun N, Figueiredo JC, Eyk JEV, Braun JG, Cheng S, Sobhani K. Prior COVID-19 Infection and Antibody Response to Single Versus Double Dose mRNA SARS-CoV-2 Vaccination. medRxiv. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | Das S, Sarkar S, Das A, Das S, Chakraborty P, Sarkar J. A comprehensive review of various categories of face masks resistant to Covid-19. Clin Epidemiol Glob Health. 2021;12:100835. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Park S, Lim SY, Kim JY, Park H, Lim JS, Bae S, Kim J, Jung J, Kim MJ, Chong YP, Choi SH, Lee SO, Kim YS, Park MS, Kim SH. Clinical and virological characteristics of SARS-CoV-2 B.1.617.2 (Delta) variant: a prospective cohort study. Clin Infect Dis. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 23. | Hu Z, Huang X, Zhang J, Fu S, Ding D, Tao Z. Differences in Clinical Characteristics Between Delta Variant and Wild-Type SARS-CoV-2 Infected Patients. Front Med (Lausanne). 2021;8:792135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 24. | Shiehzadegan S, Alaghemand N, Fox M, Venketaraman V. Analysis of the Delta Variant B.1.617.2 COVID-19. Clin Pract. 2021;11:778-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 186] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 25. | Swan DA, Bracis C, Janes H, Moore M, Matrajt L, Reeves DB, Burns E, Donnell DJ, Cohen M, Schiffer JT, Dimitrov DT. COVID-19 vaccines that reduce symptoms but do not block infection need higher coverage and faster rollout to achieve population impact. Sci Rep. 2020;11:15531. [DOI] [Full Text] |
| 26. | Jabłońska K, Aballéa S, Toumi M. The real-life impact of vaccination on COVID-19 mortality in Europe and Israel. Public Health. 2021;198:230-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | Muthukrishnan J, Vardhan V, Mangalesh S, Koley M, Shankar S, Yadav AK, Khera A. Vaccination status and COVID-19 related mortality: A hospital based cross sectional study. Med J Armed Forces India. 2021;77:S278-S282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 28. | Bae M, Kim H. Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19. Molecules. 2020;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 150] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 29. | Enmozhi SK, Raja K, Sebastine I, Joseph J. Andrographolide as a potential inhibitor of SARS-CoV-2 main protease: an in silico approach. J Biomol Struct Dyn. 2021;39:3092-3098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 229] [Article Influence: 45.8] [Reference Citation Analysis (0)] |