Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.13115
Peer-review started: October 7, 2022
First decision: October 27, 2022
Revised: November 10, 2022
Accepted: November 24, 2022
Article in press: November 24, 2022
Published online: December 16, 2022
Processing time: 67 Days and 15.3 Hours
We describe a case of relentless placoid chorioretinitis (RPC) that progressed despite administration of peribulbar and systemic corticosteroids, and was resolved by systemic combined with intravitreal methotrexate.
A 16-year-old male reported painless blurred vision and a temporal scotoma in his right eye for one week. Due to widespread distribution and continuous enlargement, multimodal imaging of the lesions led to the diagnosis of RPC. Lesions in the right eye extended despite peribulbar injection of triamcinolone acetonide, but the progression was immediately terminated by a single dose of intravitreal methotrexate. A new fresh lesion occurred in the contralateral eye despite systemic prednisolone but was resolved by oral methotrexate.
Systemic immunosuppressants should be given upon RPC diagnosis. Intravitreal methotrexate immediately halted progression and may be considered for sight-threatening cases as part of the initial therapy.
Core Tip: Relentless placoid chorioretinitis is a bilateral disease in nature and refractory to corticosteroid monotherapy, which warrants the importance of systemic immunosuppressants given upon diagnosis. Intravitreal methotrexate should also be considered as part of the initial therapy for macula-threatening cases in order to halt progression immediately and preserve visual function.
- Citation: Luo L, Chen WB, Zhao MW, Miao H. Systemic combined with intravitreal methotrexate for relentless placoid chorioretinitis: A case report. World J Clin Cases 2022; 10(35): 13115-13121
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/13115.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.13115
Relentless placoid chorioretinitis (RPC), also referred to as ampiginous choroiditis[1], is a relatively new and rare entity that was proposed by Jones et al[2] in 2000. The average age of patients was 34 years and a male preponderance was found in a case series by Jyotirmay et al[3]. RPC exhibits multiple inflammatory, deep white-creamy lesions resembling those seen in acute posterior multifocal placoid pigment epitheliopathy (APMPPE) and serpiginous choroiditis (SC). However, unlike APMPPE and SC, prolonged periods of widespread and multifocal retinal activity results in the unique appearance of numerous lesions (> 50), lesions extending anterior and posterior to the equator, and healed lesions that involve the superficial choroid[2].
Due to the rarity of this process, the optimum treatment is unknown. Most reported cases of RPC were refractory to corticosteroid monotherapy, and corticosteroid combined with systemic immunosuppressants, such as cyclosporine[4], mycophenolate mofetil[3,5], azathioprine or cyclophosphamide[3] were considered to be effective in ceasing disease progression and preventing further recurrence. However, progression during the first one to two weeks despite initiation of medication in serpiginous-like choroiditis (SLC) (with a similar clinical picture to RPC) has also been reported (so called “paradoxical worsening”)[6], which could be extremely challenging especially when the macula was about to or had already been involved at diagnosis.
Here we report a case of RPC which progressed despite administration of local and systemic corticosteroids and improved after oral combined with intravitreal methotrexate (MTX), and emphasize the importance of intravitreal MTX injection as initial therapy for sight-threatening cases.
A 16-year-old male was hospitalized complaining of progressive painless blurred vision and a temporal scotoma in his right eye for one week.
Visual acuity in his right eye had gradually decreased during the last week without soreness or redness.
The patient denied any previous ophthalmic diseases, febrile or flu-like episodes.
The family history was unremarkable.
On initial examination, his visual acuity was 20/20 and intraocular pressure was normal in both eyes. Anterior segment examination was unremarkable. Fundoscopic examination of the right eye revealed 1+ vitreous cells, along with well-circumscribed fresh creamy-white serpiginous-like lesions around the optic disc and multiple pigmented scars in the nasal and inferior mid-peripheral retina.
Uveitis workup including complete blood count, blood biochemistry, urinalysis, erythrocyte sedimentation rate, C-reactive protein, chest computed tomography and brain magnetic resonance imaging were all normal. Serologic tests for syphilis, toxoplasma, human immunodeficiency virus and T cell spot test were all negative.
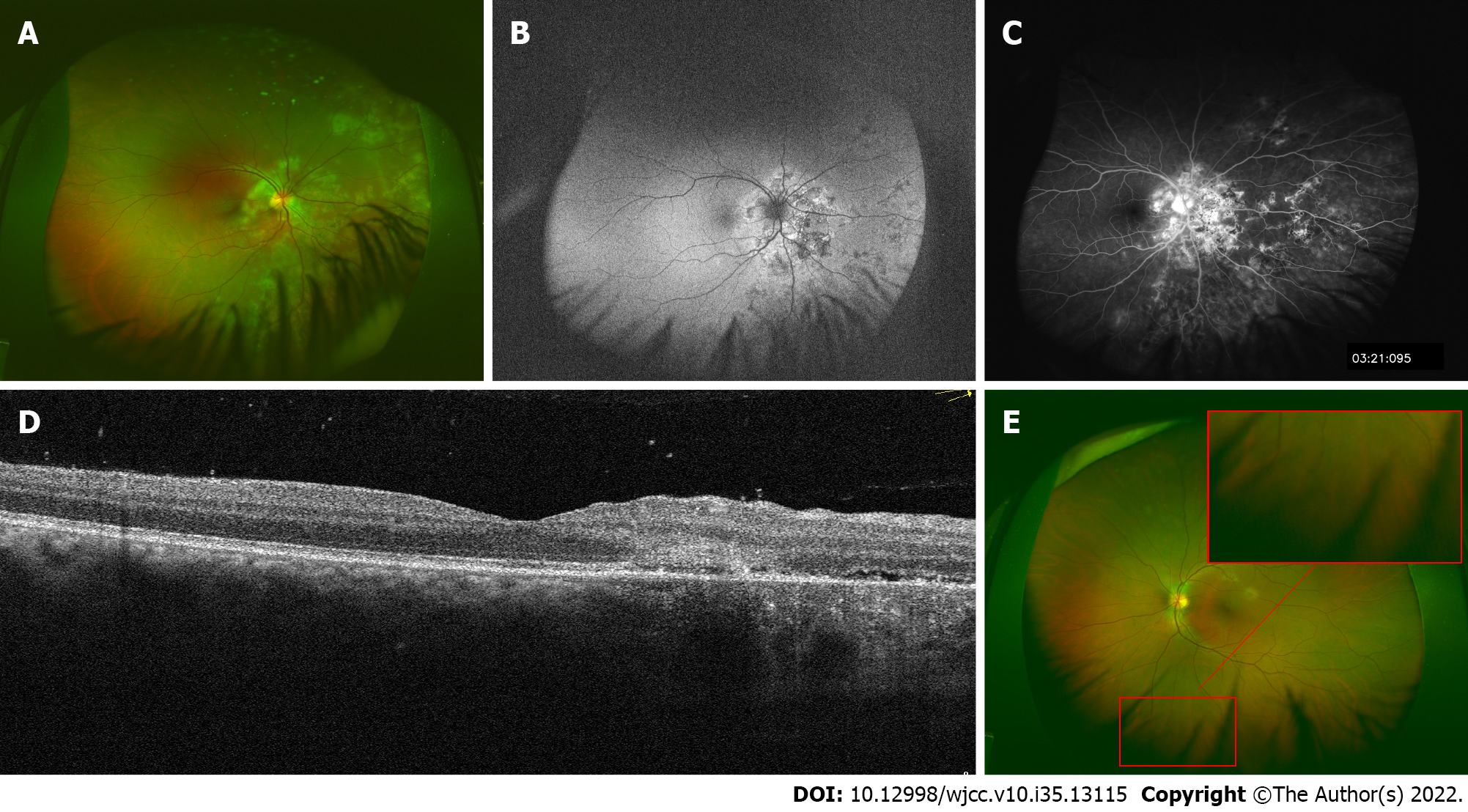
Fundus imaging showed well-circumscribed fresh creamy-white serpiginous-like lesions around the optic disc and multiple pigmented scars in the nasal and inferior mid-peripheral retina (Figure 1A). The lesions around the optic disc were hyperfluorescent on autofluorescence (AF) and in the late phase of fundus fluorescein angiography (Figure 1B and C). Optical coherence tomography (OCT) revealed normal fovea but disorganization of the outer retina in the nasal macular area (Figure 1D). The fundus of the left eye was unremarkable (Figure 1E).
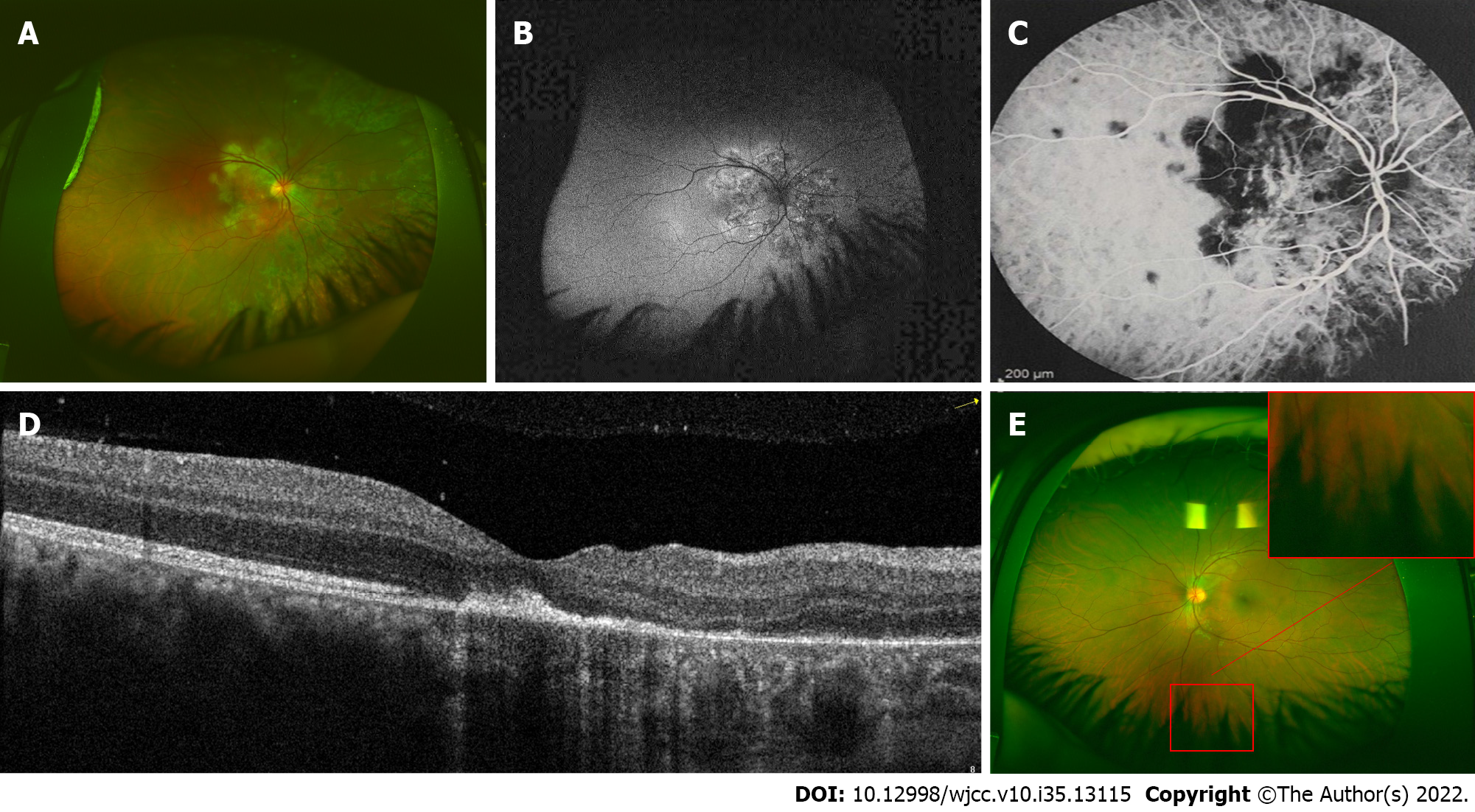
Peribulbar injection of triamcinolone acetonide (TA) 20 mg was prescribed initially as diagnostic treatment. Two weeks later, however, vision in his right eye declined to 20/50. Fundus examination revealed lesion extension which was hyperfluorescent on AF and hypofluorescent on indocyanine green angiography (Figure 2A-C). OCT showed fovea involvement, as well as atrophy of the outer retinal layers and subretinal fibrosis (Figure 2D). The left eye remained unremarkable (Figure 2E). The patient was then referred to us for further diagnosis and treatment. The widespread, multifocal and serpiginous-like pattern, together with the multimodal imaging features and poor response to treatment led us to the diagnosis of RPC.
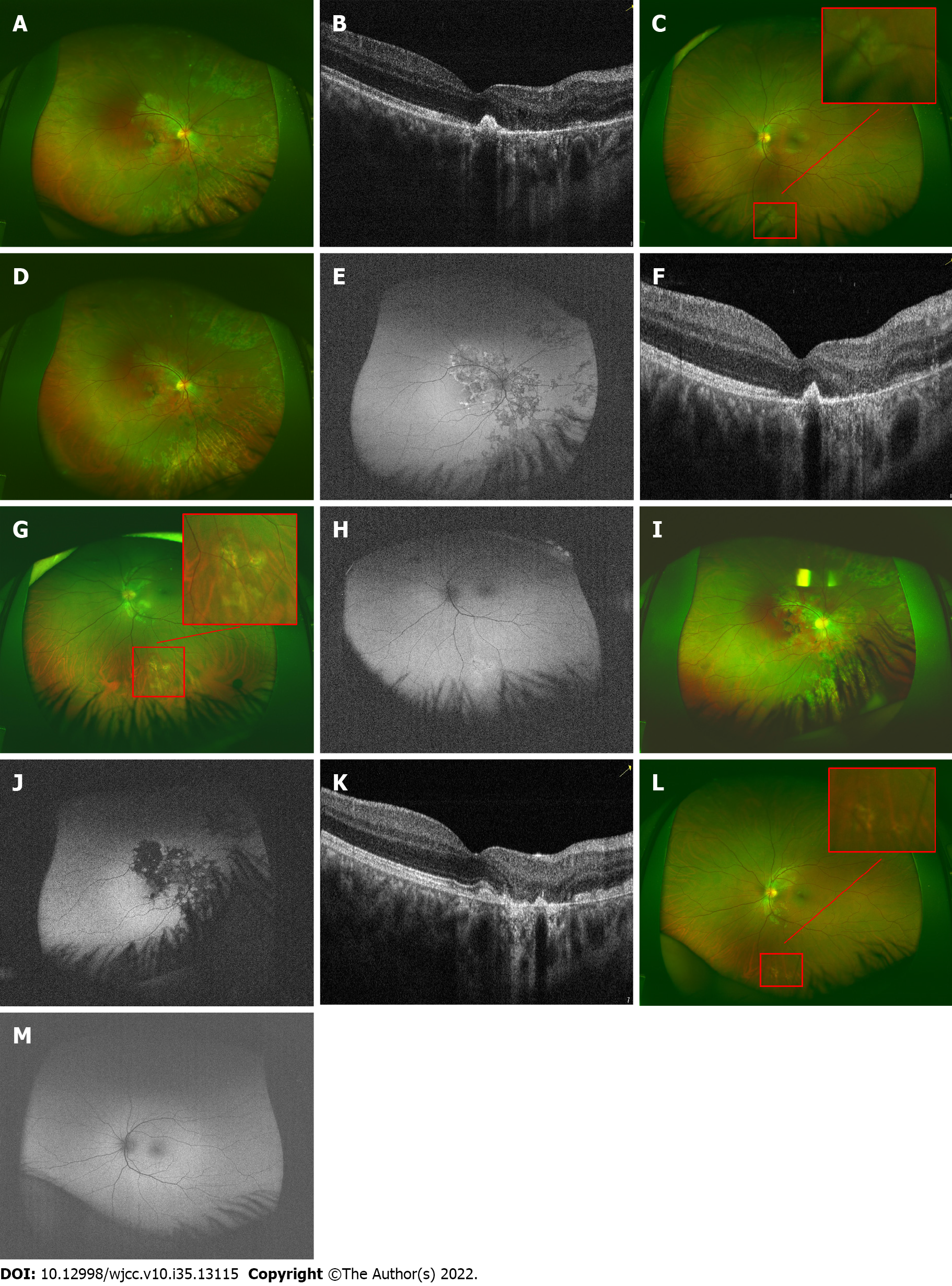
Oral MTX (20 mg/wk) and prednisolone (0.6 mg/kg/d) were administered immediately. Considering the rapid progression and central involvement, intravitreal MTX 0.4 mg was also given in order to preserve vision. Two weeks later, the fresh lesions in the right eye started to become transparent and pigmented (Figure 3A). No progression in the right eye was seen on OCT (Figure 3B), but a new creamy-white lesion appeared at six-o’clock in the equator of the left eye (Figure 3C). Considering the relatively short period of oral MTX after initiation, no further adjustment of treatment was adopted. Another two weeks later, the lesions in the right eye were almost transparent and hypofluorescent on AF (Figure 3D and E). OCT showed no further progression with the ellipsoid zone at the central fovea partially recovered (Figure 3F), and his visual acuity also improved to 30/50. In the left eye, the newly developed lesion also started to become transparent, but was hyperfluorescent on AF (Figure 3G and H). Prednisolone was then tapered off gradually, leaving oral MTX as maintenance therapy.
The patient was then followed for 21 mo, and his vision improved to 20/20 and remained stable. At the last visit, MTX had been discontinued, and no new lesions or enlargement of the scars were noted in both eyes (Figure 3I-M).
Here, we report an otherwise healthy 16-year-old male who presented with unilateral posterior uveitis. According to diagnostic criteria proposed by Jyotirmay et al[3], widespread lesions reminiscent of APMPPE in the mid-periphery, a continuously enlarging lesion at the posterior pole despite local corticosteroid therapy and outer retinal atrophy led to the diagnosis of RPC.
In this case, a new lesion developed in the contralateral eye two weeks after systemic prednisolone and MTX initiation, which suggested the nature of bilateral involvement of the disease. Jyotirmay et al[3] reported 16 RPC patients and bilateral involvement was 63% at baseline. The proportion further increased to 81% with a median follow-up time of 3 years. Although the etiology of RPC is still unknown, the involvement of a degenerative, autoimmune and/or infectious process has been considered, with some speculating that it is an ocular manifestation of a larger systemic autoimmune condition[7]. This warrants the importance of systemic administration even in patients who present with unilateral disease.
Another interesting phenomenon was that the new lesion developed in the contralateral eye two weeks after initiation of systemic treatment and healed two weeks later without any modification of systemic therapy, which indicated that it is necessary to administer immunosuppressants in addition to steroids at baseline in order to effectively control progression. As it usually takes weeks for immunosuppressants to show a clinical effect, progression despite peribulbar TA and the occurrence of a new active lesion despite systemic prednisolone in the contralateral side suggest that RPC is recalcitrant to steroid monotherapy, which is in accordance with previous studies where progression of RPC could only be stopped when cyclosporine[4], mycophenolate mofetil[3,5], azathioprine and cyclophosphamide[3] etc. were administered. For sight-threatening cases when the macula was about to be or had already been involved at baseline, progression despite systemic treatment could totally destroy the macula resulting in blindness. More aggressive therapy is needed for such situations.
Although repeated intravitreal TA was shown to be an alternative in the treatment of RPC by avoiding significant systemic side effects caused by long-term systemic therapy[8], considering the bilateral nature of the disease, it has no preventive effect on the contralateral eye and local adverse effects, such as cataract and intraocular hypertension etc., limiting its application in young patients. Intravitreal injection of MTX was previously used as a standard method for intraocular lymphoma and had been proved to be safe and effective. For some patients, the aqueous level of interleukin 10, which represents intraocular tumor load, could be lowered below detection limits after two injections given twice a week[9], which suggests its feature of rapid-onset. Intravitreal MTX has also been reported to have an excellent effect in managing presumed and refractory tuberculous SLC[10], which has a similar clinical picture to RPC. In this case, macula involvement at baseline prompted us to administer intravitreal MTX as part of the initial therapy in addition to systemic administration, and the lesions healed quickly without any further deterioration. As the vitreous half-life of MTX after a single injection was estimated to be about 10.4 h[9], weekly injection was recommended for patients with intraocular lymphoma. In order to avoid unnecessary invasive treatment, we chose to follow our patient closely and repeat intravitreal injection if necessary until systemic MTX took effect. Luckily, no new lesions were found in his right eye during follow-up, which is in agreement with previous reports that one to two injections of MTX were adequate to control SLC progression without adverse reactions[10].
Relentless placoid chorioretinitis is a bilateral disease in nature and refractory to corticosteroid monotherapy, indicating the importance of systemic immunosuppressants given at diagnosis. Intravitreal methotrexate should also be considered as part of the initial therapy for macula-threatening cases in order to terminate progression immediately and preserve visual function.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Biochemical research methods
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Şahin EA, Turkey; Ullah K, Pakistan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Nussenblatt R, Whitcup S and Palestine A. Uveitis: Fundamentals and Clinical Practice, Mosby. Year Book, St. Louis, MO 1996. [DOI] [Full Text] |
| 2. | Jones BE, Jampol LM, Yannuzzi LA, Tittl M, Johnson MW, Han DP, Davis JL, Williams DF. Relentless placoid chorioretinitis: A new entity or an unusual variant of serpiginous chorioretinitis? Arch Ophthalmol. 2000;118:931-938. [PubMed] |
| 3. | Jyotirmay B, Jafferji SS, Sudharshan S, Kalpana B. Clinical profile, treatment, and visual outcome of ampiginous choroiditis. Ocul Immunol Inflamm. 2010;18:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Uraki T, Namba K, Mizuuchi K, Iwata D, Ohno S, Kitaichi N, Ishida S. Cyclosporine and prednisolone combination therapy as a potential therapeutic strategy for relentless placoid chorioretinitis. Am J Ophthalmol Case Rep. 2019;14:87-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Yeh S, Lew JC, Wong WT, Nussenblatt RB. Relentless placoid chorioretinitis associated with central nervous system lesions treated with mycophenolate mofetil. Arch Ophthalmol. 2009;127:341-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Mishra SB, Saoji K, Pathengay A. Dual lesion margins on fundus autofluorescence associated with paradoxical worsening following treatment for tubercular serpiginous-like choroiditis. Indian J Ophthalmol. 2020;68:536-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Lambrecht P, Claeys M, De Schryver I. A Case of Ampiginous Choroiditis. Case Rep Ophthalmol. 2015;6:453-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Roth DB, Ballintine S, Mantopoulos D, Prenner J, Fine HF. Relentless placoid chorioretinitis: successful long-term treatment with intravitreal triamcinolone. Retin Cases Brief Rep. 2019;13:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Nakauchi Y, Takase H, Sugita S, Mochizuki M, Shibata S, Ishiwata Y, Shibuya Y, Yasuhara M, Miura O, Arai A. Concurrent administration of intravenous systemic and intravitreal methotrexate for intraocular lymphoma with central nervous system involvement. Int J Hematol. 2010;92:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Julian K, Langner-Wegscheider BJ, Haas A, De Smet MD. Intravitreal methotrexate in the management of presumed tuberculous serpiginous-like choroiditis. Retina. 2013;33:1943-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |