Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.13099
Peer-review started: September 30, 2022
First decision: October 24, 2022
Revised: November 2, 2022
Accepted: November 22, 2022
Article in press: November 22, 2022
Published online: December 16, 2022
Processing time: 74 Days and 16.8 Hours
Acupuncture is relatively popular worldwide, but an unregulated operation can easily lead to infections. The purpose of this report was to analyze a clinical case of surgery combined with the use of antibiotics for the treatment of thoracic vertebral infection by Escherichia coli (E. coli) after acupuncture.
A 63-year-old male was diagnosed with E. coli infection in the thoracic vertebra after acupuncture. His fever and pain did not improve after treatment with broad-spectrum antibiotics for 10 d. Thus, debridement of the infected area and biopsy were decided. The final pathology confirmed the diagnosis of vertebral infection by E. coli. The patient underwent anterior and posterior thoracic vertebral debridement and internal fixation surgery combined with the use of sensitive antibiotics. He had no fever or backache 3 mo postoperatively.
In this report, we first considered antibiotic treatment for the patient with septic spinal infection, but the effect was not obvious. Interventional surgery was combined with the use of sensitive antibiotics to relieve backache, and good clinical results were achieved. Furthermore, acupuncture practitioners should pay attention to hygienic measures.
Core Tip: Lack of aseptic awareness of acupuncture can easily cause patients to develop infections at the treatment area. Some even lead to serious medical errors. The patient in this case developed vertebral infection after acupuncture treatment on the back. After a cycle of antibiotic treatment without significant improvement, early surgical intervention in combination with the postoperative use of sensitive antibiotics may be considered.
- Citation: Mo YF, Mu ZS, Zhou K, Pan D, Zhan HT, Tang YH. Surgery combined with antibiotics for thoracic vertebral Escherichia coli infection after acupuncture: A case report. World J Clin Cases 2022; 10(35): 13099-13107
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/13099.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.13099
Spinal infections account for approximately 2%-7% of infections of the musculoskeletal system[1,2]. With the widespread use of antibiotics, spinal infection is difficult to diagnose early and has a long treatment cycle[3,4]. From the experience of this case, relevant medical history is an important hint for an early diagnosis. Detailed history-taking may reveal easily missed systemic symptoms such as fever or history of infection at other sites associated with the initial onset of the disease.
A 63-year-old male developed fever and backache after acupuncture 27 d prior.
The patient was diagnosed with a herniated lumbar disc 31 d prior to admission and underwent acupuncture, but his backache gradually worsened. On the 4th d after acupuncture, the patient developed a fever, but he did not pay attention to it and took antibiotics (which the patient could not describe). During the next 4 wk, his fever sporadically recurred and backache gradually worsened.
The patient had a history of pneumonia 7 years prior but denied having tuberculosis. He also denied having a history of diabetes; however, after our examination and blood glucose monitoring, he was diagnosed with diabetes. The patient denied having a history of other diseases.
The patient was born in Hangzhou and resided there for many years. He denied exposure to epidemic water and residence in an epidemic area. He had a history of smoking for 25 years (at present, 10 cigarettes/d). Furthermore, he denied a history of alcoholism, special dietary hobbies, and exposure to toxic and harmful substances, smuggling, endemic diseases, occupational diseases, and special chemical and radiation exposure. He had no familial history of hereditary disease or genetic predisposition to disease and had no immediate family members with infectious diseases.
The patient was conscious but tired, with pressure pain at the low back, no obvious pressure pain in the lower lumbar region, no radiating pain and numbness in both lower limbs, a negative Lasegue sign, normal muscle strength in the lower limbs, no elicitation of pathological signs, and normal walking gait.
A blood test was conducted after admission (Table 1). The other tests and results were as follows: T-cell test for tuberculosis infection, negative; tuberculosis smear, no antacid bacilli detected; blood routine aerobic culture for 5 d, no bacterial growth observed; hepatitis B surface antigen, hepatitis B e antigen, and hepatitis B core antibody tests, positive; and urine and stool tests, normal.
| Blood project | Measured value |
| White blood cells (× 109/L) | 9.94 |
| Red blood cells (× 1012/L) | 4.40 |
| Blood platelets (× 109/L) | 235.00 |
| Hemoglobin (g/L) | 131.00 |
| Percentage of neutrophils (%) | 75.60 |
| Neutrophil absolute value (× 109/L) | 7.50 |
| C-reactive protein (mg/L) | 19.18 |
| Blood sedimentation (mm/h) | 45.00 |
| Glycated hemoglobin (%) | 6.70 |
| Alpha-fetoprotein (ng/mL) | 2.28 |
| Carcinoembryonic antigen (ng/mL) | 3.58 |
| CA199 (U/mL) | 13.68 |
| Ferrous protein (ng/mL) | 290.20 |
| Prostate specific antigen ratio (i) | 0.10 |
| Total prostate-specific antigen (ng/mL) | 17.20 |
| Free prostate-specific antigen (ng/mL) | 1.678 |
| Antinuclear antibody (AU/mL) | < 4.00 |
| Anti-cardiolipin antibody (AU/mL) | 26.90 |
| Anti-cyclic citrullinated peptide antibody (U/mL) | < 0.50 |
Multiple preoperative and postoperative blood infection indices, including percentage of neutrophils, erythrocyte sedimentation rate, and C-reactive protein level, were conducted (Figure 1).
Preoperative images: Computed tomography revealed destruction of the 9/10 thoracic vertebrae (Figure 2A-D). Normal thoracic vertebral magnetic resonance imaging revealed large patchy T1 image hypointensity, T2 image isointensity, and fat suppression image hyperintensity in the 9/10 thoracic vertebrae (Figure 2E-H). Infectious disease of the 9/10 thoracic vertebrae was considered.
Thoracic vertebral contrast-enhanced magnetic resonance imaging revealed thoracic vertebrae physiological curvature, fair sequence, and smoothly arranged vertebrae. The 9/10 thoracic vertebrae had large patchy T1 image hypointensity, T2 image isointensity, and fat suppression image hyperintensity. With stenosis of the intervertebral space and thickening of the surrounding soft tissue, no obvious abnormal signal was detected in the tube, and there was a high possibility of tuberculosis considering the infectious lesions of the 9/10 thoracic vertebrae (Figure 2I-L).
The final diagnosis in this case was septic thoracic vertebral infection with Escherichia coli (E. coli).
After admission, the patient was given levofloxacin and cefoperazone sulbactam for 10 d as anti-infectives. The patient experienced recurrent episodes of backache and fever reaching 38 °C in the evening. Considering his physical condition and his family’s request, we excluded any contraindications to surgery and performed surgery after perfecting the preoperative examination.
The patient was operated under general anesthesia in the prone position, and his back was disinfected with 5% povidone-iodine solution; towels and skincare film were applied. A 12 cm incision was made through the skin and subcutaneous tissue, the T8 ribs were cut, the pleura was shown, and the thoracic cavity was examined to reach the lateral side of the injured vertebrae. The anterior edge of the psoas major muscle was separated longitudinally and pulled open with a Hoffman hook. The 9/10 intervertebral disc with purulent fluid overflow was examined, the segmental artery was ligatured, and about 20 mL of purulent fluid and bone destruction of the 9/10 vertebrae were observed.
The 9/10 intervertebral disc was gradually resected, and a large amount of inflammatory tissue was observed. The 9/10 intervertebral space and part of the T9 vertebral osteomyelitis lesion were excised, and the lesion was completely removed (intraoperative pathology sent for rapid sectioning showed chronic purulent osteomyelitis infection). A considerable amount of saline and hydrogen peroxide was flushed, and the 9/10 intervertebral disc was excised. The cartilaginous end plate was treated with a scraper, the T9 vertebral lesion was partially excised, and iliac bone graft was performed for the intervertebral fusion of T9/10. The bone graft was well positioned after monitoring with a C-arm X-ray machine. Then, hemostasis, irrigation, drainage, local immersion with vancomycin, and placement of a closed thoracic drainage device were performed followed by layer-by-layer suturing. Next, The patient was positioned in the prone position. Routine disinfection and towel laying was performed. A 10-cm incision was made between the T8-10 spinous process. The skin, subcutaneous tissue, and thoracic dorsal fascia were incised, and the muscles were retracted on both sides through the multifidus paravertebral muscle gap to reveal the corresponding segmental plate and articular eminence. Hemostasis was achieved via electrocoagulation. Positioned above the intersection of the line of the outer edge of the superior articular eminence and the transverse eminence parallelogram, T9/10 was opened, reamed, and tapped. Four universal domestic pedicle screws (6.5 mm × 40.0 mm) were placed. The connecting rod and nut were installed under the guidance of a C-arm X-ray machine. Intraoperative bleeding was about 600 mL, and 2 U of allogeneic red blood cells were transfused.
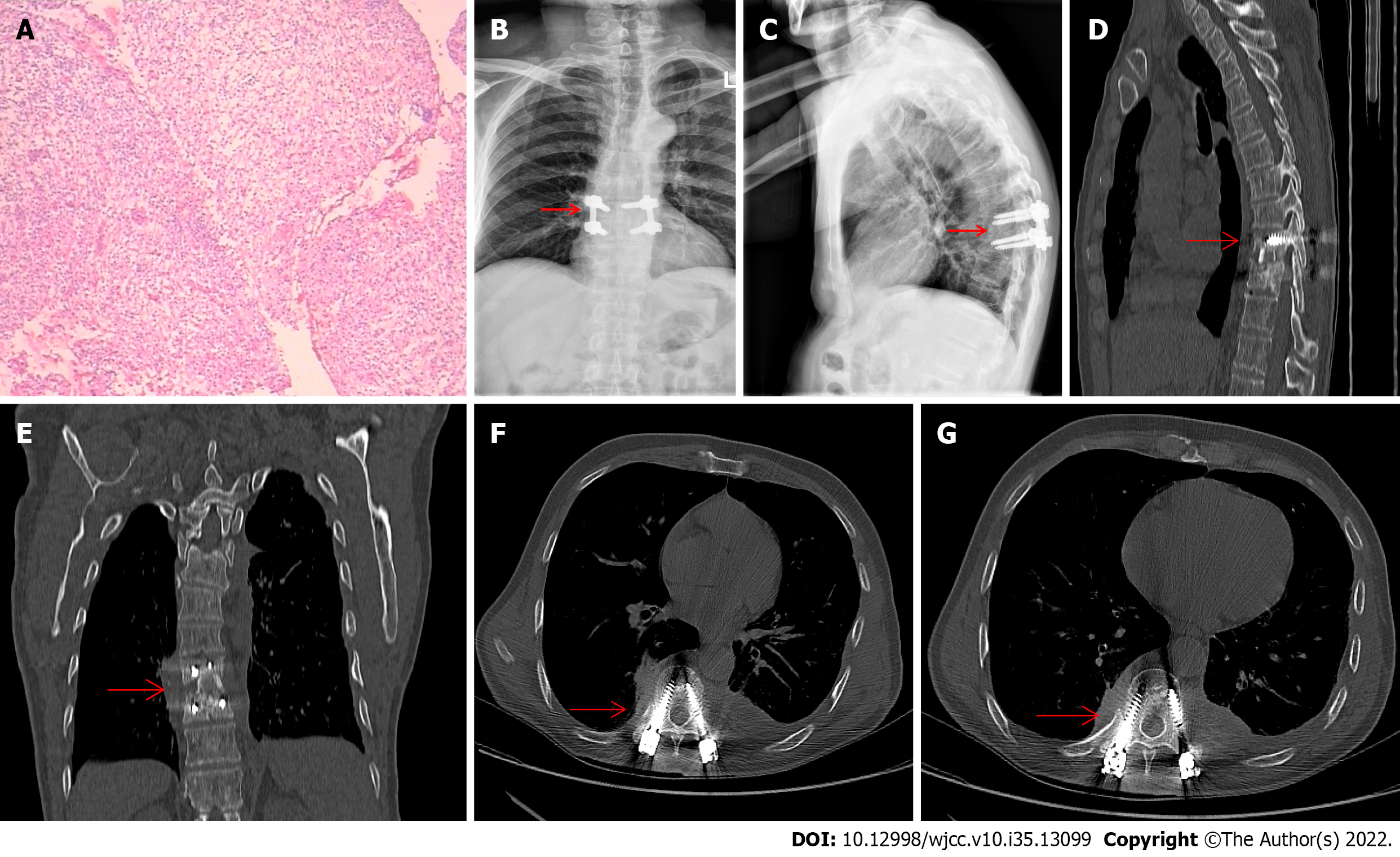
When the results of postoperative specimen culture were not available, the patient was given cefoperazone sulbactam and linezolid as anti-infectives. The specimen culture results indicated that the infecting bacterium was E. coli (Figure 3A), and meropenem combined with levofloxacin was given as anti-infective.
The patient had no fever or backache 3 mo postoperatively. At the 3-mo follow-up, postoperative signs were detected by X-ray in the 9/10 thoracic vertebrae (Figure 3B and C). Postoperative signs were detected by computed tomography in the 9/10 thoracic vertebrae (Figure 3D-G).
In some developed countries, the prevalence of spinal infections is 1/20000 to 1/100000, with a mortality rate of 2%-20%[5,6]. Spinal infections mostly occur in patients under 20-years-old and patients between 50-70-years-old. Males are more susceptible to spinal infections than females with a sex ratio of approximately 2:1-5:1[1,2]. Diagnosing spinal infection has been clinically challenging due to its relatively low incidence, lack of specificity of symptoms, and insidious course in some patients.
Acupuncture treatment can become a source of infection if asepsis is not standardized. By searching the relevant literature in databases such as China National Knowledge Infrastructure, PubMed, and Embase, we summarized the literature related to vertebra and its surrounding infections caused by acupuncture reported from 2000 to 2022[7-15] (Table 2). Based on the relevant cases, it is clear that vertebral infections caused by acupuncture are rare, with the most common site being the lumbar region, often due to the application of long needles; the most common bacterium was Staphylococcus aureus, and the most common treatment modality was antibiotic therapy combined with or without surgical debridement. Residual complications remain after treatment in more than half of the cases.
| Ref. | Country | Causes of infection | Site of infection | Bacterial species | Treatment method | Duration of treatment | Prognosis |
| Xiao et al[7], 2022 | China | Acupuncture for the waist | Lumbar spine and lungs | Burkholderia pseudomallei | Abscess debridement and antibiotics | - | The bacteria was found again in a urine test 5 mo after discharge from the hospital |
| Alexandre et al[8], 2018 | Portugal | Acupuncture for the waist | The left facet joint between L4 and L5 vertebrae and epidural abscess from T12 to S1 vertebral level | Methicillin-resistant Staphylococcus aureus | Percutaneous drainage of the abscesses and antibiotics | 8 wk | Full recovery, no recurrence |
| Yao et al[9], 2016 | China | Acupuncture for neck and shoulder | An epidural abscess at C4 to T2 | Methicillin-resistant Staphylococcus aureus | Antibiotics | 6 wk | Infection was controlled, but the patient had decreased muscle strength in the lower extremities |
| Robinson et al[10], 2015 | Australia | Acupuncture for cervical spondylosis | Atlantoaxial septic arthritis | Methicillin-sensitive Staphylococcus aureus | Antibiotics | 6 wk | Effective control of infection and chronic neck pain |
| He et al[11], 2015 | China | Acupuncture for the waist | Lumbar spine and intervertebral disc | Group C Streptococcus | Percutaneous lumbar discectomy, external drainage, irrigation using antibiotics, and postoperative antibiotic therapy | - | Infection control and pain relief |
| Chiang et al[12], 2014 | Singapore | Acupuncture for the waist | T12 and urinary system | Methicillin-sensitive Staphylococcus aureus | Antibiotics | 6 wk | - |
| Lee et al[13], 2012 | Korea | Acupuncture at the back of the neck | Epidural abscess at C1-3 level | - | Antibiotics | - | Abscess subsides |
| Bang et al[14], 2006 | Korea | Acupuncture for the waist | Abscesses of bilateral psoas muscles and spondylitis with epidural abscess | Escherichia coli | Antibiotics | - | Infection controlled, but no recovery of neurological symptoms |
| Daivajna et al[15], 2004 | United Kingdom | Acupuncture for the lumbosacral | The right L5/S1 facet joint | Staphylococcus aureus | Antibiotic treatment and surgical debridement | - | Symptoms disappeared, and infection was controlled |
Spinal infection causes pain, fever, movement limitation, and neurological impairment, which seriously affect the patient quality of life. Therefore, if patients have these symptoms, combined with susceptibility factors, such as diabetes mellitus and hepatitis C, or are immunocompromised, the possibility of septic spinal infection should be considered[16,17].
For patients in the acute stage, symptoms such as severe backache and accompanying fever can help make an early diagnosis. However, with the widespread use of antibiotics, many patients come to the clinic during the subacute or chronic stage without specific manifestations; this causes delay of diagnosis for 2-6 mo, with an early misdiagnosis rate of up to 80%[3,4]. Fever and elevated inflammatory indicators may support the diagnosis, but such indicators are not always elevated at the time of presentation, especially in older patients with a less-pronounced inflammatory response. Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) suggest that the doctor should be aware of various relevant tests at an early stage[18,19]. In particular, it should be noted that among the inflammatory indicators, CRP has a higher differential diagnostic significance than ESR[20,21].
The main principle in the treatment of septic spinal infection is early diagnosis and treatment. However, literature on the best way to treat septic spinal infection is lacking. Nonsurgical treatment requires a longer period of bed rest, and the special blood flow of the intervertebral disc makes it difficult for antibiotics to completely remove the lesion, which may lead to bone destruction of the vertebrae and affect spinal stability[22]. For these reasons, it has been suggested that septic spinal infection should be diagnosed early, cleared thoroughly, and combined with the use of antibiotics to maintain spinal stability and reduce complications[23].
In this case, the patient’s infection site was relatively limited; thus, we considered a direct extension of the infection from the long acupuncture needles. The patient was initially treated with antibiotics alone. After treatment, the body temperature could not be controlled, and the backache worsened. Thus, surgery was performed, and the postoperative clinical outcome was satisfactory. Therefore, we believe that septic spinal infection should be actively treated surgically in cases where early nonoperative treatment is ineffective, which is conducive to complete clearance of the lesion, restoration of spinal stability, and reduction of hospitalization time.
Some scholars have reported that the benefit of debridement and internal fixation to stabilize the spine in patients with septic spinal infection outweighs the risk of recurrent infection and reoperation[24]. The application of internal fixation helps stabilize the spine, relieve pain, restore or maintain normal physiological curvature of the spine, and allow patients to walk early. For the use of sensitive antibiotics, we cannot rely too much on bacterial culture results due to the chance of single sampling. Based on experience and pathological results, we combined other antibiotics with sensitive antibiotics in the postoperative period. In this case, we found that antibiotics + debridement + internal fixation had a higher healing rate. Surgical debridement reduces the host of pathogenic microorganisms and breaks the barrier of the bacterial biofilm, which facilitates the penetration of antibiotics into the infected lesion to control the infection.
In this study, we first considered antibiotic treatment for the patient with septic spinal infection. When the effect was not obvious, interventional surgery combined with the use of sensitive antibiotics was performed to relieve the patient’s backache. Whether the surgery should be performed also requires consideration of the patient’s physical condition and expectations. Furthermore, acupuncture practitioners should pay attention to hygienic measures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bharara T, India; Nakaji K, Japan; Rosboch GL, Italy S-Editor: Chen YL L-Editor: Filipodia A P-Editor: Chen YL
| 1. | Ha JH, Kim SH, Park SM, Lee CK, Chang BS, Kim H. Geriatric risk in the surgical management of infectious spondylitis. Geriatr Gerontol Int. 2017;17:984-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 2. | Aljawadi A, Jahangir N, Jeelani A, Ferguson Z, Niazi N, Arnall F, Pillai A. Management of Pyogenic Spinal Infection, review of literature. J Orthop. 2019;16:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Tsantes AG, Papadopoulos DV, Vrioni G, Sioutis S, Sapkas G, Benzakour A, Benzakour T, Angelini A, Ruggieri P, Mavrogenis AF; World Association Against Infection In Orthopedics And Trauma W A I O T Study Group On Bone And Joint Infection Definitions. Spinal Infections: An Update. Microorganisms. 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 4. | Gregori F, Grasso G, Iaiani G, Marotta N, Torregrossa F, Landi A. Treatment algorithm for spontaneous spinal infections: A review of the literature. J Craniovertebr Junction Spine. 2019;10:3-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Schoenfeld AJ, Wahlquist TC. Mortality, complication risk, and total charges after the treatment of epidural abscess. Spine J. 2015;15:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Aagaard T, Roed C, Dahl B, Obel N. Long-term prognosis and causes of death after spondylodiscitis: A Danish nationwide cohort study. Infect Dis (Lond). 2016;48:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Xiao L, Zhou T, Chen J, Hu Y, Zheng Y. Paravertebral abscess and bloodstream infection caused by Burkholderia pseudomallei after acupuncture: a case report. BMC Complement Med Ther. 2022;22:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Alexandre AR, Raimundo P. Epidural, paravertebral and bilateral psoas abscess after lumbar acupuncture. BMJ Case Rep. 2018;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Yao Y, Hong W, Chen H, Guan Q, Yu H, Chang X, Yu Y, Xu S, Fan W. Cervical spinal epidural abscess following acupuncture and wet-cupping therapy: A case report. Complement Ther Med. 2016;24:108-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Robinson A, Lind CR, Smith RJ, Kodali V. Atlanto-axial infection after acupuncture. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | He C, Wang T, Gu Y, Tian Q, Zhou B, Wu C. Unusual case of pyogenic spondylodiscitis, vertebral osteomyelitis and bilateral psoas abscesses after acupuncture: diagnosis and treatment with interventional management. Acupunct Med. 2015;33:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Chiang GS, Tong K. Acupuncture causing methicillin-sensitive Staphylococcus aureus spondylodiscitis resulting in bacteremia and bacteriuria. J Am Geriatr Soc. 2014;62:2221-2222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Lee JH, Cho JH, Jo DJ. Cervical epidural abscess after cupping and acupuncture. Complement Ther Med. 2012;20:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Bang MS, Lim SH. Paraplegia caused by spinal infection after acupuncture. Spinal Cord. 2006;44:258-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Daivajna S, Jones A, O'Malley M, Mehdian H. Unilateral septic arthritis of a lumbar facet joint secondary to acupuncture treatment--a case report. Acupunct Med. 2004;22:152-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Lee YD, Jeon YH, Kim YH, Ha KY, Hur JW, Ryu KS, Kim JS, Kim YJ. Clinical Characteristics and Outcomes of Patients with Culture-Negative Pyogenic Spondylitis according to Empiric Glycopeptide Use. Infect Chemother. 2019;51:274-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Zimmerli W. Clinical practice. Vertebral osteomyelitis. N Engl J Med. 2010;362:1022-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 413] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 18. | Lee KY. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J. 2014;8:216-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Kim CJ, Kim EJ, Song KH, Choe PG, Park WB, Bang JH, Kim ES, Park SW, Kim HB, Oh MD, Kim NJ. Comparison of characteristics of culture-negative pyogenic spondylitis and tuberculous spondylitis: a retrospective study. BMC Infect Dis. 2016;16:560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Digby JM, Kersley JB. Pyogenic non-tuberculous spinal infection: an analysis of thirty cases. J Bone Joint Surg Br. 1979;61:47-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 127] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Schulitz KP, Assheuer J. Discitis after procedures on the intervertebral disc. Spine (Phila Pa 1976). 1994;19:1172-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Michiels I, Jäger M. [Spondylodiscitis : Current strategies for diagnosis and treatment]. Orthopade. 2017;46:785-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Parchi PD, Evangelisti G, Andreani L, Girardi F, Darren L, Sama A, Lisanti M. Postoperative Spine Infections. Orthop Rev (Pavia). 2015;7:5900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Dennis Hey HW, Nathaniel Ng LW, Tan CS, Fisher D, Vasudevan A, Liu KG, Thambiah JS, Kumar N, Lau LL, Wong HK, Tambyah PA. Spinal Implants Can Be Inserted in Patients With Deep Spine Infection: Results From a Large Cohort Study. Spine (Phila Pa 1976). 2017;42:E490-E495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |