Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.13052
Peer-review started: August 30, 2022
First decision: October 12, 2022
Revised: October 12, 2022
Accepted: November 17, 2022
Article in press: November 17, 2022
Published online: December 16, 2022
Processing time: 105 Days and 20.9 Hours
We report two cases of acute femoral artery occlusion following the use of ProGlide in minimally invasive cardiac surgery and insertion of large-bore catheters through the common femoral artery. This will add to the existing body of literature by highlighting the possible complications associated with the use of ProGlide and reiterate that the use of the sono-guided ProGlide skill will reduce the incidence of these complications.
A 78-year-old man underwent minimally invasive cardiac surgery for severe aortic valve stenosis. After the operation, the puncture site of the common femoral artery was closed using ProGlide. The next morning, after regaining consciousness, he complained of pain, motor weakness (grade 2), and coldness in the right lower extremity. A 65-year-old man underwent minimally invasive cardiac surgery for a large secundum atrial septal defect (5 cm × 5 cm). After the operation, the puncture site of the common femoral artery was closed using ProGlide. After extubation, the patient complained of paresthesia of the right thigh. Both the patients underwent emergency surgery for acute occlusion of the common femoral artery.
If the sono-guided ProGlide skill is used, complications can be prevented, and ProGlide can be safely used.
Core Tip: Sono-guided ProGlide skill is advocated for use during cardiopulmonary bypass to avoid the complication of femoral artery occlusion and stenosis associated with its use by standard techniques.
- Citation: Lee J, Huh U, Song S, Lee CW. Acute limb ischemia after minimally invasive cardiac surgery using the ProGlide: A case series. World J Clin Cases 2022; 10(35): 13052-13057
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/13052.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.13052
The insertion of large-bore catheters through the common femoral artery was previously performed using the cutdown technique. The advantage of the cutdown technique is that the operator is able to directly visualize the artery, which makes it easier to perform the procedure and ensure adequate hemostasis. However, there are some complications associated with the procedure, including inguinal hematomas, femoral nerve injuries, lymphocele and wound infections, with a reported prevalence of 14%-22%[1]. Recently, as a suture-mediated closure device has been developed, large-bore access holes can be closed more quickly, and safely, and less invasively, using the Perclose ProGlide™ SMC System (Abbott, IL, USA), and access-related complications related to cutdown can be reduced[2-5]. Despite these advantages, complications that may occur when using the Perclose ProGlide include dissection, acute femoral artery stenosis or occlusion, bleeding, and device failure[6]. According to a multicenter, randomized, controlled trial of totally percutaneous access vs open femoral exposure for endovascular aortic aneurysm repair (the PEVAR trial), vascular complications occurred in 4 out of 50 cases in the Perclose ProGlide group (hemorrhage 1, thrombosis/occlusion 2, and vascular injury 1)[3]. Acute occlusion requires urgent surgical treatment because there is a risk of nerve damage or the necessity for amputation in severe cases.
We report two cases of acute limb ischemia after closure of large-bore access holes using Perclose ProGlide after minimally invasive cardiac surgery.
Case 1: A 78-year-old man presented to the outpatient clinic with dyspnea.
Case 2: A 65-year-old man presented with dyspnea.
Case 1: A 78-year-old man presented to the outpatient clinic with dyspnea.
Case 2: A 65-year-old man presented with dyspnea.
Case 1: Ten years earlier, he had undergone percutaneous coronary intervention for coronary artery occlusion and was treated for diabetes and prostate cancer.
Case 2: Not relevant.
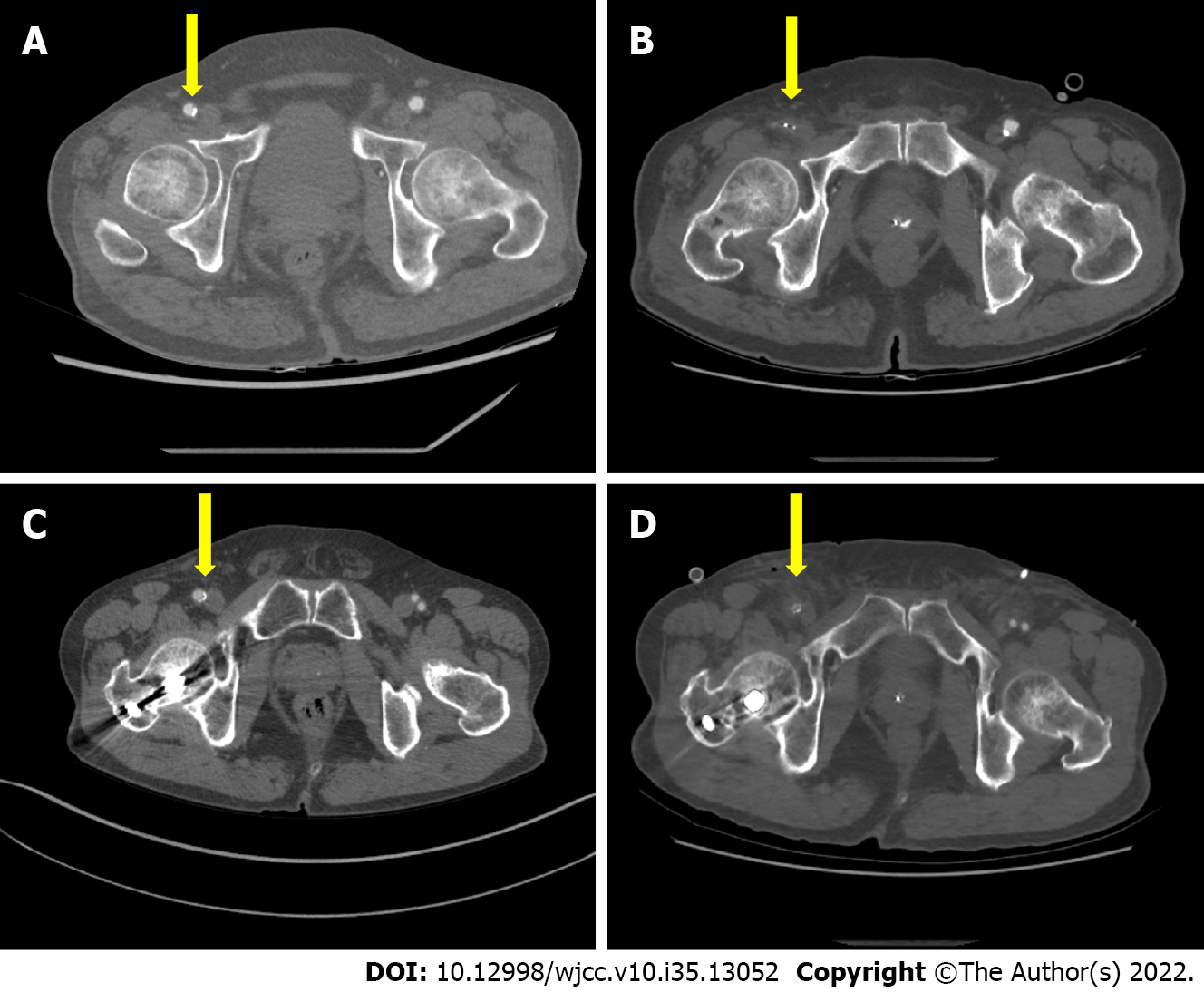
Case 1: We observed calcification, without stenosis, of the right common femoral artery (size, 8 mm × 8 mm) on preoperative computed tomography (CT) (Figure 1A).
Case 2: Preoperative CT showed calcification of the right common femoral artery (size 7.5 mm × 7.3 mm), but no stenosis was observed (Figure 1C).
The patient was diagnosed with severe aortic valve stenosis and surgery was planned.
A large secundum atrial septum defect (5 cm × 5 cm) was diagnosed on echocardiography, and minimally invasive cardiac surgery and patch closure of the atrial septum defect with bovine pericardium under right mini-thoracotomy were planned.
Cardiopulmonary bypass was performed, with cannulation using Bio-Medicus™ NextGen cannula 17 Fr (Medtronic, Dublin, Ireland), in the right femoral artery. The patient underwent aortic valve replacement with minimally invasive cardiac surgery, and the percutaneous puncture was closed using Perclose ProGlide™ SMC System (Abbott, IL, USA). He was shifted to the intensive care unit after surgery without any apparent complications.
The next morning, after regaining consciousness, the patient complained of pain, motor weakness (grade 2), and coldness in the right leg. Ultrasound showed that blood flow was very weak in the right leg, and blood flow could not be confirmed in the dorsalis pedis and posterior tibial arteries. Emergency surgery was performed because the arteries of right leg were not contrasted on CT angiography (Figure 1B).
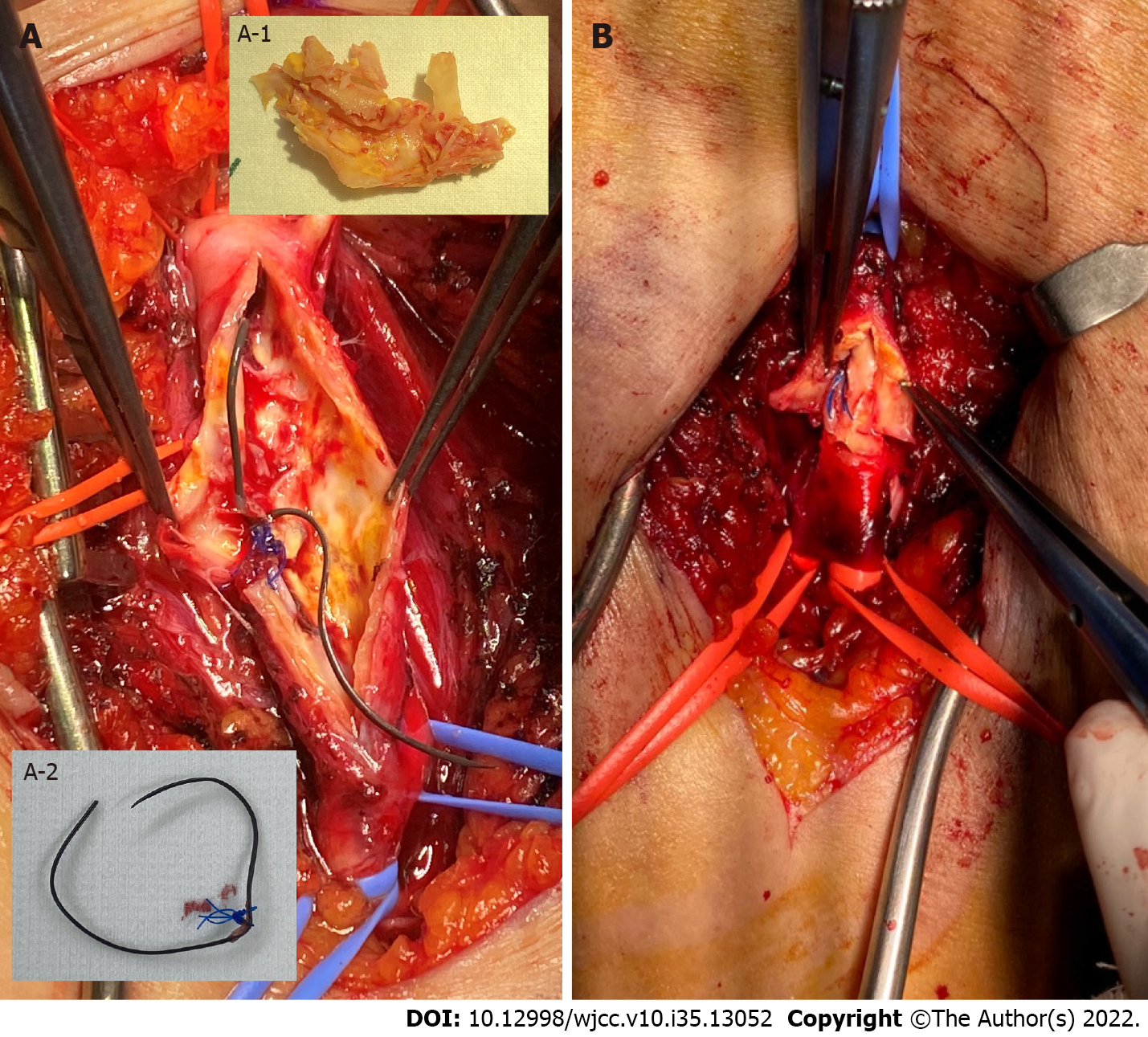
After exfoliating the right common femoral artery, we found a plastic ring hanging outside the vessel wall. After clamping it, arteriotomy was performed, and it was confirmed that a long plastic line hung in the suture tie was caught in the dorsal arterial wall. Contrary to the CT findings, the vessel wall was severely calcified, and the lumen was narrow (Figure 2A). Thrombectomy and endarterectomy with patch closure were performed using bovine pericardium.
Bio-Medicus™ NextGen cannulae 17 Fr (Medtronic, Dublin, Ireland) was used for the arterial line of the cardiopulmonary bypass, and percutaneous puncture was performed by the Seldinger technique under ultrasound guidance in the common femoral artery of the right side. After surgery, the percutaneous puncture was closed using the Perclose ProGlide™ SMC System (Abbott, IL, USA). He was moved to the intensive care unit without any apparent complications and was extubated 3 h after surgery.
After extubation, the patient complained of paresthesia in the right thigh, and CT showed that there was no arterial flow toward the distal part of the right common femoral artery (Figure 1D). Emergency surgery was performed immediately and the thread of the ProGlide™ SMC System (Abbott, IL, USA) was found tied to the dorsal arterial wall. Contrary to the CT findings, the vessel wall was severely calcified and the lumen was narrow (Figure 2B). After thrombectomy and endarterectomy, the arterial flow in the right leg was completely restored.
Postoperatively, the patient's arterial flow recovered completely. After postoperative day 10, the patient was transferred to a rehabilitation hospital for lower limb rehabilitation. After 3 mo, his condition improved to motor grade 4, and he was able to walk using a brace.
The patient recovered without any other sequelae after the surgery and was discharged on postoperative day 6.
The PEVAR trial reported that the Preclose technique using ProGlide in endovascular aortic aneurysm repair (EVAR) is safe and effective and can minimize access-related complications[2]. It was also better than standard open femoral exposure. Compared with standard open femoral exposure, Proglide and Prostar XL showed significantly faster hemostasis and better outcomes with respect to bleeding, groin pain, and overall quality of life[3]. Two types of closure devices are available for closing large-bore access holes: Prostar XL and Perclose ProGlide. In a multicenter prospective study comparing Proglide and Prostar XL for transcatheter aortic valve replacement (TAVR)[7] and a meta-analysis comparing Proglide and Prostar XL in TAVR and EVAR, ProGlide showed lesser bleeding complications than Prostar XL[1].
Several complications are associated with the use of ProGlide. Examples include acute stenosis or occlusion of the femoral artery, bleeding, and device failure. Mathisen et al[8] conducted PEVAR using Perclose ProGlide, and set the access sites to Group 1 with OD. It was classified as 12-16 Fr and group 2 with an OD 17-22 Fr, and the technical success was compared. In Group 1, out of 388 patients, 3 had thrombosis/occlusion, 2 had stenosis or dissection, 4 had bleeding or hematoma, and 10 had pseudoaneurysms. In Group 2, out of 449 patients, 4 had thrombosis/occlusion (with 1 case of stenosis or dissection), 2 had bleeding or hematoma, and 5 had pseudoaneurysms.
Since the functioning of the ProGlide in the blood vessel cannot be visualized, the underlying cause of complications caused by the ProGlide has not yet been clearly demonstrated. The occurrence of complications associated with ProGlide in other TAVI studies is 3.4% to 8%[9,10]. To overcome this issue, Honda et al[6] reported the advantages of a novel sono-guided ProGlide skill. They used sono-guided ProGlide skill to reduce the occurrence of complications associated with ProGlide by 1.6%, and there were not any cases of acute occlusion or stenosis. The general method of using ProGlide is to insert a 0.035-inch guide wire at the puncture site of the femoral artery and then to insert the ProGlide device. An examination is performed to determine significant blood return, and the ProGlide is withdrawn until the "foot" develops and the "foot" makes contact with the arterial wall. When the return of blood stops, the needle plunger is depressed. If ProGlide does not work properly, the "foot" can interfere with posterior wall movement, which can lead to acute occlusion of femoral artery and ProGlide failure. Honda et al[6] used echo to push the ProGlide into a blood vessel until blood flow returned, folded and rotated the "foot" slightly, and then retried the sequential procedure when abnormal movement was detected. After optimal ProGlide behavior was identified, the needle plunger was depressed and the suture knot was deployed outside the skin.
If the sono-guided ProGlide skill is used, complications such as acute occlusion or stenosis of femoral arteries can be prevented, and ProGlide can be safely used.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ozden F, Turkey; Ullah K, Pakistan S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Maniotis C, Andreou C, Karalis I, Koutouzi G, Agelaki M, Koutouzis M. A systematic review on the safety of Prostar XL vs ProGlide after TAVR and EVAR. Cardiovasc Revasc Med. 2017;18:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Lee WA, Brown MP, Nelson PR, Huber TS. Total percutaneous access for endovascular aortic aneurysm repair ("Preclose" technique). J Vasc Surg. 2007;45:1095-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Nelson PR, Kracjer Z, Kansal N, Rao V, Bianchi C, Hashemi H, Jones P, Bacharach JM. A multicenter, randomized, controlled trial of totally percutaneous access vs open femoral exposure for endovascular aortic aneurysm repair (the PEVAR trial). J Vasc Surg. 2014;59:1181-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 218] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 4. | Watelet J, Gallot JC, Thomas P, Douvrin F, Plissonnier D. Percutaneous repair of aortic aneurysms: a prospective study of suture-mediated closure devices. Eur J Vasc Endovasc Surg. 2006;32:261-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Starnes BW, Andersen CA, Ronsivalle JA, Stockmaster NR, Mullenix PS, Statler JD. Totally percutaneous aortic aneurysm repair: experience and prudence. J Vasc Surg. 2006;43:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Honda Y, Araki M, Yamawaki M, Tokuda T, Tsutumi M, Mori S, Sakamoto Y, Kobayashi N, Hirano K, Ito Y. The novel echo-guided ProGlide technique during percutaneous transfemoral transcatheter aortic valve implantation. J Interv Cardiol. 2018;31:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Berti S, Bedogni F, Giordano A, Petronio AS, Iadanza A, Bartorelli AL, Reimers B, Spaccarotella C, Trani C, Attisano T, Marella Cenname A, Sardella G, Bonmassari R, Medda M, Tomai F, Tarantini G, Navarese EP; Italian Society of Interventional Cardiology‐GISE†. Efficacy and Safety of ProGlide Versus Prostar XL Vascular Closure Devices in Transcatheter Aortic Valve Replacement: The RISPEVA Registry. J Am Heart Assoc. 2020;9:e018042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Mathisen SR, Nilsson KF, Larzon T. A Single Center Study of ProGlide Used for Closure of Large-Bore Puncture Holes After EVAR for AAA. Vasc Endovascular Surg. 2021;55:798-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Barbash IM, Barbanti M, Webb J, Molina-Martin De Nicolas J, Abramowitz Y, Latib A, Nguyen C, Deuschl F, Segev A, Sideris K, Buccheri S, Simonato M, Rosa FD, Tamburino C, Jilaihawi H, Miyazaki T, Himbert D, Schofer N, Guetta V, Bleiziffer S, Tchetche D, Immè S, Makkar RR, Vahanian A, Treede H, Lange R, Colombo A, Dvir D. Comparison of vascular closure devices for access site closure after transfemoral aortic valve implantation. Eur Heart J. 2015;36:3370-3379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 110] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 10. | Nara Y, Watanabe Y, Kozuma K, Kataoka A, Nakashima M, Hioki H, Kawashima H, Nagura F, Shirai S, Tada N, Araki M, Naganuma T, Yamanaka F, Yamamoto M, Hayashida K. Incidence, Predictors, and Mid-Term Outcomes of Percutaneous Closure Failure After Transfemoral Aortic Valve Implantation Using an Expandable Sheath (from the Optimized Transcatheter Valvular Intervention [OCEAN-TAVI] Registry). Am J Cardiol. 2017;119:611-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |