Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.12880
Peer-review started: August 11, 2022
First decision: September 25, 2022
Revised: October 7, 2022
Accepted: November 17, 2022
Article in press: November 17, 2022
Published online: December 16, 2022
Processing time: 125 Days and 0.4 Hours
Improving the sagittal lumbar-pelvic parameters after fusion surgery is important for improving clinical outcomes. The impact of midline lumbar fusion (MIDLF) on sagittal lumbar-pelvic alignment for the management of degenerative lumbar diseases is still unknown.
To analyze the effects of short-segment MIDLF and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) on sagittal lumbar-pelvic parameters.
We retrospectively analyzed 63 patients with degenerative lumbar diseases who underwent single-segment MIDLF or MIS-TLIF. The imaging data of patients were collected before surgery and at the final follow-up. The radiological sagittal parameters included the lumbar lordosis (LL), lower LL, L4 slope (L4S), L5 slope (L5S), L5 incidence (L5I), L1 axis and S1 distance (LASD), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and PI-LL mismatch (PI-LL). Additionally, the clinical outcomes, including lower back and leg pain visual analog scale (VAS) and Oswestry disability index (ODI) scores, were also analyzed.
In both groups, LL and Lower LL significantly increased, while L5I and LASD significantly decreased at the final follow-up compared to that recorded prior to operation (P < 0.05). In the MIDLF group, L4S significantly decreased compared to that recorded prior to operation (P < 0.05), while the mean SS significantly increased and the PT significantly decreased compared to that recorded prior to operation (P < 0.05). In the MIS-TLIF group, SS slightly increased and the mean PT value decreased compared to that recorded prior to operation, but without a statistically significant difference (P > 0.05). However, the PI-LL in both groups was significantly reduced compared to that recorded prior to operation (P < 0.05). There was no significant difference in the sagittal lumbar-pelvic parameters between the two groups prior to operation and at the final follow-up (P > 0.05). In addition, the change in sagittal lumbar-pelvic parameters did not differ significantly, except for ΔLASD within the two groups (P > 0.05). The mean lower back and leg pain VAS and ODI scores in both groups were significantly improved three months after surgery and at the final follow-up. Though the mean ODI score in the MIDLF group three months after surgery was slightly higher than that in the MIS-TLIF group, there was no significant difference between the two groups at the final follow-up.
Short-segment MIDLF and MIS-TLIF can equally improve sagittal lumbar parameters such as LL, Lower LL, L5I, and LASD in the treatment of lumbar degenerative diseases. However, MIDLF had a larger impact on pelvic parameters than MIS-TLIF.
Core Tip: It is important for clinical outcomes to improve the sagittal lumbar-pelvic parameters after fusion surgery. However, whether midline lumbar fusion (MIDLF) and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) differ in the impact of the sagittal lumbar-pelvic alignment for degenerative lumbar diseases is still unknown. The current study compared the imaging data and clinical efficacy of MIDLF with those of MIS-TLIF to evaluate the impact of the two procedures on the sagittal lumbar-pelvic parameters in the treatment of lumbar degenerative diseases.
- Citation: Wang YT, Li BX, Wang SJ, Li CD, Sun HL. Radiological and clinical outcomes of midline lumbar fusion on sagittal lumbar-pelvic parameters for degenerative lumbar diseases. World J Clin Cases 2022; 10(35): 12880-12889
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/12880.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.12880
Posterior lumbar fusion surgery is an effective method for the treatment of lumbar degenerative diseases such as lumbar spinal stenosis, lumbar disc herniation, and degenerative lumbar spondy
Midline lumbar interbody fusion (MIDLF) is also considered a limited invasive procedure with a modest muscle dissection[6]. The technique of cortical bone trajectory (CBT) screw placements not only contributes to enhancing screws’ holding power by increasing cortical bone contact but also reduces the paraspinal soft tissue dissection following a medial to lateral screw-insertion direction, which facilitates the early recovery of patients postoperatively[6-8]. However, the length and diameter of CBT screws used in MIDLF tend to be smaller than those of traditional pedicle screws, so the supporting strength of CBT screws on the anterior column of lumbar vertebrae might be not as good as that of the traditional pedicle screws, which can achieve three-column lumbar fixation[9]. In addition, little research has focused on the improvement of sagittal lumbar-pelvic parameters with MIDLF.
Studies have confirmed that it is important for clinical outcomes to improve the sagittal lumbar-pelvic parameters after fusion surgery. However, whether MIDLF and MIS-TLIF differ in terms of the impact of sagittal lumbar-pelvic alignment for management of degenerative lumbar diseases is still unknown. The current study compared the imaging data and clinical efficacy of MIDLF with those of MIS-TLIF to evaluate the impact of both procedures on the sagittal lumbar-pelvic parameters in the treatment of lumbar degenerative diseases.
Patients seen at Peking University First Hospital (China, Beijing) from January 2019 to March 2021 who met the study inclusion and exclusion criteria were enrolled. This study was approved by the Human Subjects Institutional Review Board of Peking University First Hospital. Patients who underwent single-segment MILDF and MIS-TLIF for lower back pain, unilateral or bilateral lower-limb radiating pain, numbness, or intermittent claudication after strict conservative treatments for at least three months with complete preoperative and postoperative lateral lumbar X-ray images and at least one year of follow-up data after surgery were included. We excluded individuals with spinal tumors, tuberculosis, infection, scoliosis, or fractures; a history of spinal surgery; postoperative complications such as surgical site infection, cage displacement, or fixation failure; or without radiological images available from the study.
In our center, both MIDLF and MIS-TLIF could be employed for the treatment of degenerative lumbar diseases, such as lumbar disc herniation, lumbar spinal stenosis, and lumbar spondylolisthesis. MIDLF was more likely to be performed in patients with osteoporosis or osteopenia, as the CBT technique could enhance the screw stability. Furthermore, MIDLF tends to be used for central decompression of the lumbar canal due to central lumbar disc herniation, lumbar spinal stenosis, or lumbar spondylolisthesis, while MIS-TLIF is preferred for treating unilateral nerve root compression or nerve root canal stenosis caused by intervertebral disc herniation.
In the MIDLF group, after anesthesia and preoperative preparation, a median lumbar incision was made and the bilateral paraspinal muscle was dissected to expose the lamina and the lateral margin of the facet joint. CBT screw paths were set, following a mediolateral and caudocephalad direction to ensure the screws made adequate contact with the cortical bone. Then, thorough spinal canal and nerve root decompression was performed by facetectomy and resection of the partial vertebral lamina and thickening of the ligamentum flavum of the lesion segment. Next, the intervertebral disc on the lesion side was completely removed, and the cartilage endplate was scraped to the subchondral bone. After the intervertebral space was cleaned up and expanded, autologous bone grains were implanted into the anterior intervertebral space. Then, an appropriate cage with autologous bone was placed into the interbody space. CBT screws were inserted following the prepared paths, and the rods and nuts were connected. After creating a bone graft bed, a posterolateral bone graft was performed using local autologous bone grains mixed with allograft bone. Finally, a drainage tube was placed, and the wound was closed layer by layer.
In the MIS-TLIF group, after anesthesia and preoperative preparation, an incision was made from the middle line between the caudal and the cranial pedicle at the affected level. The subcutaneous tissue was dissected and moved to one side. Next, the working channel was placed through the space of the multifidi muscle to expose the unilateral facet joint after inserting an expansion sleeve progressively. A thorough decompression of the spinal canal and nerve root was performed by facetectomy and resection of partial vertebral lamina and ligamentum flavum. After performing a discectomy and scraping the cartilage endplate, an appropriate cage filled with autologous bone was placed. Then, the pedicle screws were percutaneously implanted under the guidance of fluoroscopy. After applying appropriate intervertebral pressure, the rods and nuts were installed. Finally, the drainage tube was placed and the wound was closed.
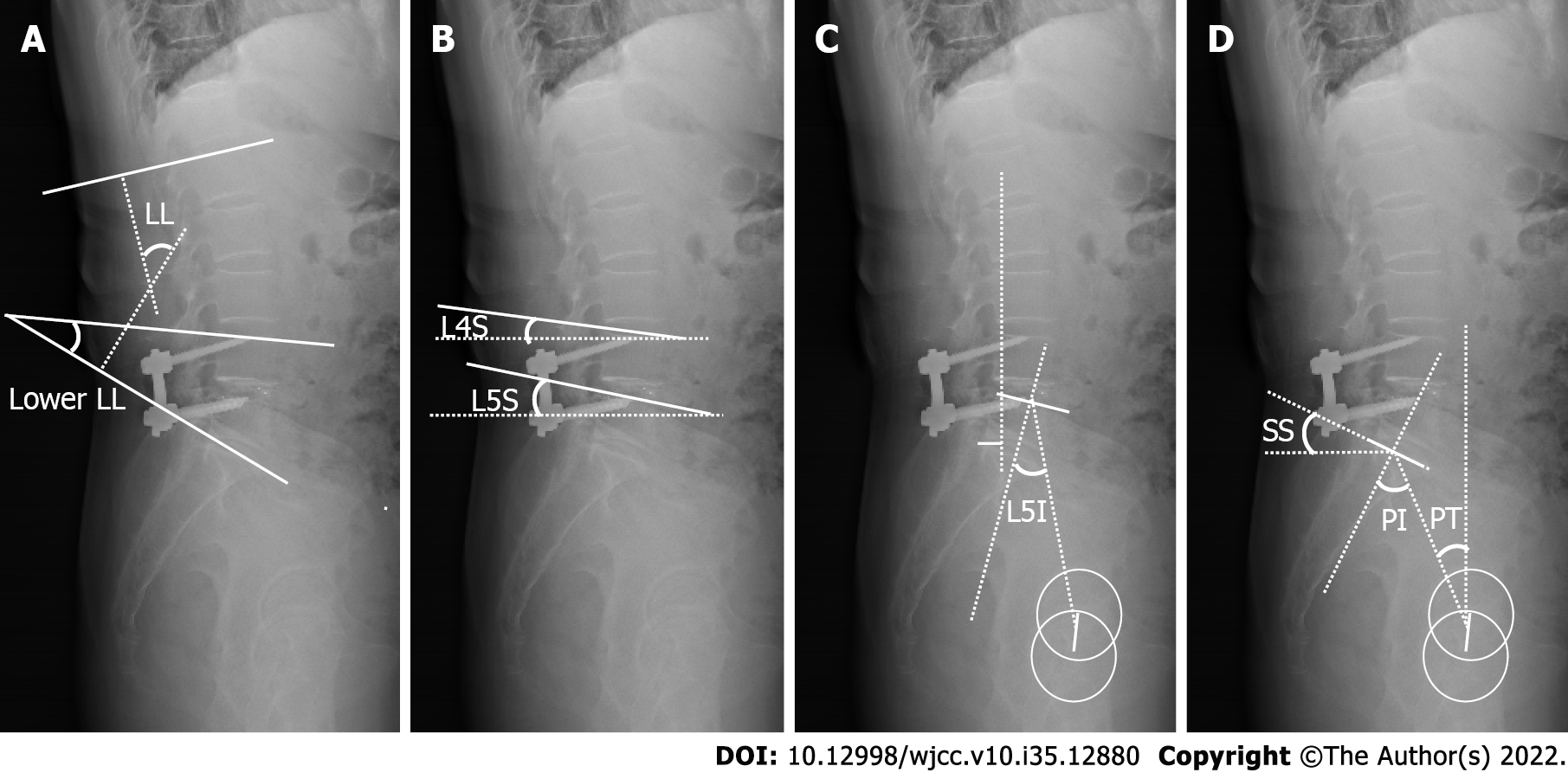
Full-length X-ray radiographs of the spine were taken for all patients in a relaxed standing position. The following preoperative and final follow-up sagittal lumbar-pelvic parameters were measured by two independent spinal surgeons using PACS software: lumbar lordosis (LL), lower LL, L4 slope (L4S), L5 slope (L5S), L5 incidence (L5I), L1 axis and S1 distance (LASD), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and PI-LL mismatch (PI-LL) (Figure 1). The mean value of three measurements from each surgeon was used. The change in each parameter (ΔLL, ΔLower LL, ΔL4S, ΔL5S, ΔL5I, ΔLASD, ΔPI, ΔPT, and ΔSS) was also calculated by subtracting the preoperative value from the value recorded at the final follow-up.
The clinical outcomes were evaluated preoperatively, at three months after surgery, and at the final follow-up. The degree of pain in the lower back and lower limbs was evaluated using a visual analog scale (VAS), while lumbar function was evaluated with the Oswestry disability index (ODI). The VAS and ODI scores were compared between the two groups prior to operation and at each follow-up visit.
SPSS 23.0 (IBM Corp., Armonk, NY, United States) was used for analysis. According to the normality of the data, the quantitative variables were presented as mean ± standard deviation or median (min, max) values, and qualitative variables were shown using numbers. A paired t-test or paired Wilcoxon test was used for intragroup comparison of continuous variables, and two independent-samples t-tests were used for the intergroup comparison. The chi-squared test or Fisher’s exact test was used for the analysis of categorical variables. A two-tailed P value of < 0.05 was chosen to indicate a statistically significant difference.
In the MIDLF group, there were 14 men and 20 women, with an age of 62.94 ± 13.03 years old. Twenty cases were diagnosed with lumbar spinal stenosis, 11 cases were diagnosed with lumbar disc herniation, and three cases were diagnosed with lumbar spondylolisthesis. In the MIS-TLIF group, there were 16 men and 13 women, with an age of 58.76 ± 8.65 years old. Eight cases were diagnosed with lumbar spinal stenosis, 19 cases were diagnosed with lumbar disc herniation, and two cases were diagnosed with lumbar spondylolisthesis. There was no significant difference in general information, such as age, gender, body mass index, or follow-up time, between the two groups (Table 1, P > 0.05).
| MIDLF (n = 34) | MIS-TLIF (n = 29) | P value | |
| Age (yr) | 62.94 ± 13.03 | 58.76 ± 8.65 | 0.146 |
| Gender (male/female) | 14/20 | 16/13 | 0.268 |
| BMI (kg/cm2) | 25.82 ± 3.81 | 26.06 ± 3.68 | 0.802 |
| Main diagnosis | |||
| Lumbar spinal stenosis | 20 | 8 | |
| Lumbar disc herniation | 11 | 19 | |
| Lumbar spondylolisthesis | 3 | 2 | |
| Operation segment | |||
| L3-4 | 2 | 0 | |
| L4-5 | 25 | 20 | |
| L5-S1 | 7 | 9 | |
| Operation duration (min) | 227.88 ± 35.53 | 240.24 ± 38.47 | 0.190 |
| Estimated blood loss (mL) | 400 (200-600) | 300 (150-500) | 0.013a |
| Hospital stay time (d) | 7 (4-11) | 6 (3-11) | 0.085 |
| Follow-up time (mo) | 15.65 ± 2.65 | 15.31 ± 1.85 | 0.568 |
The average operative duration in the MIDLF group was similar to that in the MIS-TLIF group (P = 0.190); however, the average volume of blood estimated to have been lost during surgery in the MIS-TLIF group was significantly less than that in the MIDLF group (P = 0.013). The patients in the MIDLF group required a similar length of hospital stay after surgery as those in the MIS-TLIF group (P = 0.085) (Table 1).
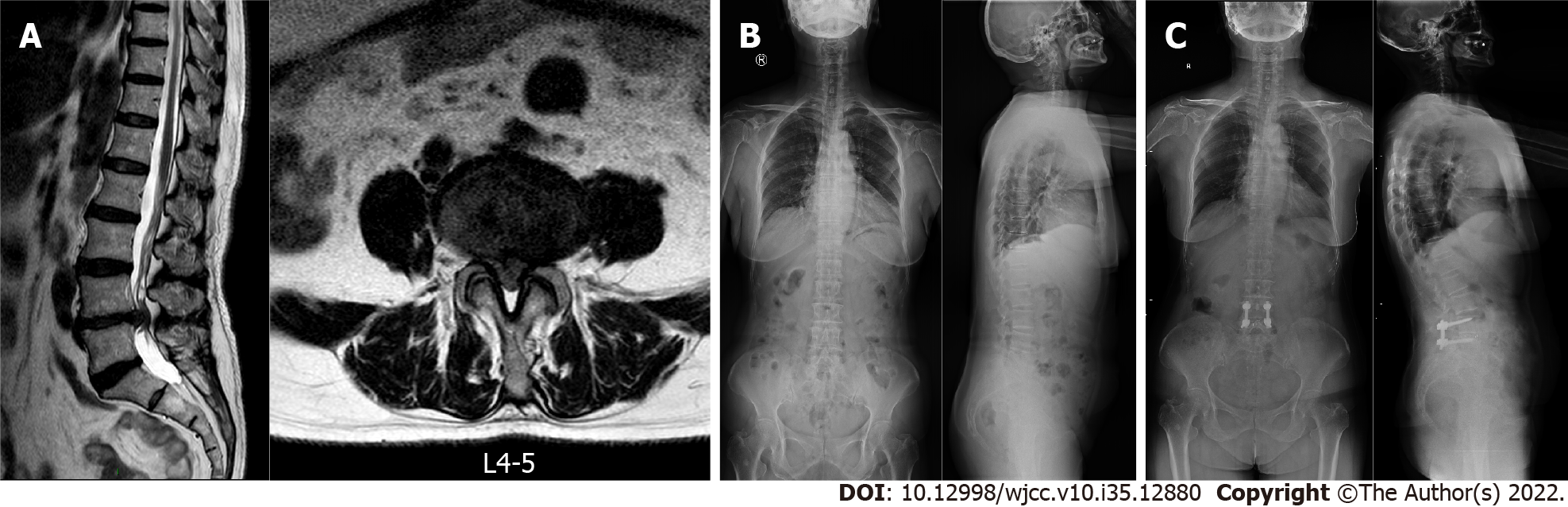
In the MIDLF group, LL and Lower LL significantly increased at the final follow-up; L4S, LASD, and L5I significantly decreased compared to that recorded prior to operation (P < 0.05); and L5S decreased at the final follow-up, but the difference was not statistically significant (P > 0.05). As for sagittal pelvic parameters, PI was similar to that recorded prior to operation, while SS significantly increased (P = 0.008) and PT significantly decreased (P = 0.014) compared to those recorded prior to operation. In the MIS-TLIF group, LL and Lower LL significantly increased (P < 0.05) and LASD and L5I significantly decreased (P < 0.05) at the final follow-up compared to those recorded prior to operation, while L4S and L5S were similar at the final follow-up to the pre-operation values (P > 0.05). For the sagittal pelvic parameters, SS increased and PT decreased compared to those values recorded prior to operation, but there was no statistically significant difference in either (P > 0.05). Meanwhile, the PI-LL in both groups significantly decreased compared to that seen prior to operation (P < 0.05). When it came to the inter-group comparison performed at each time point, there was no significant difference in the postoperative sagittal lumbar-pelvic parameters between the two groups (P > 0.05). The ΔLASD value in the MIS-TLIF group was significantly larger than that in the MIDLF group, while no significant differences were found in ΔLL, ΔLower LL, ΔL4S, ΔL5S, ΔL5I, ΔPI, ΔPT, ΔSS, or ΔPI-LL between the two groups. A typical case of MIDLF is shown in Figure 2, and the sagittal lumbar-pelvic parameters in both groups are shown in Table 2.
| MIDLF (n = 34) | MIS-TLIF (n = 29) | P value | |
| LL | |||
| Preoperative | 35.74 ± 14.77 | 35.17 ± 13.50 | 0.875 |
| Final follow-up | 41.45 ± 12.83 | 41.21 ± 12.11 | 0.940 |
| ΔLL | 5.48 (-14.13, 33.86) | 5.34 (-14.35, 33.85) | 0.772 |
| P value (pre-final) | 0.005a | 0.002a | |
| Lower LL | |||
| Preoperative | 23.21 ± 9.65 | 22.21 ± 9.90 | 0.688 |
| Final follow-up | 27.57 ± 8.00 | 26.49 ± 8.74 | 0.609 |
| ΔLower LL | 4.24 (-11.43, 24.02) | 4.27 ± 7.19 | 0.472 |
| P value (pre-final) | 0.001a | 0.003a | |
| L4S | |||
| Preoperative | 3.79 ± 8.03 | 4.81 ± 7.70 | 0.611 |
| Final follow-up | 2.65 ± 8.69 | 4.14 ± 8.35 | 0.492 |
| ΔL4S | -1.06 (-13.06, 12.83) | -0.63 (-12.74, 13.22) | 0.180 |
| P value (pre-final) | 0.029a | 0.157 | |
| L5S | |||
| Preoperative | 11.42 ± 7.63 | 12.74 ± 7.53 | 0.494 |
| Final follow-up | 11.16 ± 9.04 | 14.44 ± 14.78 | 0.284 |
| ΔL5S | -0.27 (-10.97, 25.62) | 2.58 (-16.20, 41.31) | 0.562 |
| P value (pre-final) | 0.204 | 0.673 | |
| L5I | |||
| Preoperative | 21.99 (8.01-55.98) | 23.26 (12.15-56.93) | 0.270 |
| Final follow-up | 19.67 (9.21-44.23) | 22.62 ± 9.91 | 0.440 |
| ΔL5I | -2.08 (15.33-22.47) | -2.65 (-15.77, 21.61) | 0.184 |
| P value (pre-final) | 0.02a | 0.001a | |
| LASD | |||
| Preoperative | 9.04 ± 23.11 | 14.24 ± 22.70 | 0.374 |
| Final follow-up | 2.80 ± 20.12 | 4.26 ± 20.85 | 0.779 |
| ΔLASD | -6.23 (-47.71, 32.43) | -7.91 (-49.24, 30.84) | 0.038a |
| P value (pre-final) | 0.002a | 0.000a | |
| PI | |||
| Preoperative | 46.73 ± 10.43 | 49.15 ± 10.81 | 0.369 |
| Final follow-up | 46.49 ± 11.38 | 50.21 ± 13.26 | 0.189 |
| ΔPI | -0.94 (-7.93, 38.08) | 0.49 (-8.15, 38.13) | 0.319 |
| P value (pre-final) | 0.062 | 0.754 | |
| PT | |||
| Preoperative | 18.92 (7.45, 40.71) | 21.14 ± 7.95 | 0.241 |
| Final follow-up | 18.54 ± 7.73 | 21.14 ± 8.04 | 0.846 |
| ΔPT | -1.56 (18.10-15.89) | -1.03 ± 6.22 | 0.673 |
| P value (pre-final) | 0.014a | 0.379 | |
| SS | |||
| Preoperative | 26.32 ± 8.52 | 26.98 ± 8.16 | 0.754 |
| Final follow-up | 28.92 ± 9.92 | 29.39 ± 9.02 | 0.196 |
| ΔSS | 2.60 (-13.78, 30.10) | 2.65 (-11.60, 30.63) | 0.847 |
| P value (pre-final) | 0.008a | 0.098 | |
| PI-LL | |||
| Preoperative | 10.99 ± 13.60 | 13.98 ± 13.46 | 0.385 |
| Final follow-up | 4.33 ± 11.87 | 8.99 ± 11.24 | 0.117 |
| ΔPI-LL | -6.65 ± 10.19 | -4.53 (-28.71, 29.39) | 0.453 |
| P value (pre-final) | 0.001a | 0.001a |
There was no significant difference in lower back pain VAS scores between the two groups at pre-operation and the final follow-up, but the lower back pain VAS score in the MIS-TLIF group at three months after surgery was significantly lower than that in the MIDLF group. There was also no significant difference in leg pain VAS scores between the two groups three months after surgery and at the final follow-up, though the pre-operation leg pain VAS score in the MIS-TLIF group was significantly greater than that in the MIDLF group. Both the lower back pain and leg pain VAS scores three months after surgery and at the final follow-up were significantly improved compared to the pre-operation scores in both groups (P > 0.05). The mean ODI scores of the two groups were significantly improved at three months after surgery and the final follow-up (P < 0.05). The mean ODI in the MIDLF group at three months after surgery was slightly higher than that in the MIS-TLIF group despite comparable preoperative values. However, there was no significant difference in ODI scores between the two groups at the final follow-up. The clinical outcomes of the two groups are shown in Table 3.
| MIDLF (n = 34) | MIS-TLIF (n = 29) | P value | |
| Back pain VAS score | |||
| Preoperative | 6.00 (0.00-8.00) | 6.00 (0.00-9.00) | 0.788 |
| 3 mo postoperation | 2.00 (0.00-5.00) | 1.00 (0.00-4.00) | 0.028a |
| Final follow-up | 1.00 (0.00-5.00) | 1.00 (0.00-3.00) | 0.928 |
| Leg pain VAS score | |||
| Preoperative | 7.00 (0.00-9.00) | 8.00 (2.00-10.00) | 0.039a |
| 3 mo postoperation | 2.00 (0.00-3.00) | 1.00 (0.00-3.00) | 0.270 |
| Final follow-up | 1.00 (0.00-2.00) | 0.00 (0.00-5.00) | 0.107 |
| ODI score | |||
| Preoperative | 63.50 ± 13.33 | 66.86 ± 14.61 | 0.343 |
| 3 mo postoperation | 23.47 ± 5.66 | 20.21 ± 6.83 | 0.042a |
| Final follow-up | 14.12 ± 6.10 | 13.28 ± 4.13 | 0.531 |
Lumbar fusion surgery can restore the spinal sagittal balance and improve lumbar-pelvic alignment, which is highly significant for alleviating lumbar symptoms and maintaining long-term clinical outcomes[10]. There is a correlation between LL and lower back pain; indeed, a previous study confirmed that a reduction in LL might lead to greater local stress and eventual aggravation of lower back discomfort, and the appropriate restoration of LL was proposed to achieve better clinical outcomes after surgery[11]. Lower LL could significantly increase the lordosis of the lumbosacral segment and restore the curve of the upper lumbar spine, which is helpful for improving the overall LL[12]. Additionally, as the loss of Lower LL might be relevant to adjacent segmental degeneration, the importance of improving Lower LL should be considered when performing lumbar fusion surgery[12,13]. In our study, LL and Lower LL in the MIDLF and MIS-TLIF groups were significantly refined and contributed to relief from postoperative symptoms at the final follow-up. Moreover, statistical analysis showed that there was no significant difference in ΔLL or ΔLower LL within the two groups. Therefore, it was considered that short-segment MIDLF and MIS-TLIF have an equal ability to improve LL and Lower LL in the treatment of lumbar degenerative diseases. This result was consistent with the findings of Elmekaty et al[14], who found that MIDLF and MIS-TLIF have an almost similar capability to improve the sagittal balance in the treatment of single-level lumbar spondylolisthesis.
L4S, L5S, and L5I could reflect the balance of the lower lumbar to some extent[15]. In our study, L5I in both groups and L4S in the MIDLF group significantly decreased at the final follow-up compared to pre-operation. Additionally, in terms of refining the balance of the lower lumbar vertebrae, the capacities of both minimally invasive surgeries were perhaps similar up to the point of the final follow-up. Moreover, the improvement in sagittal parameters such as LASD would be helpful for restoring the sagittal lumbar-pelvic alignment. Indeed, Funao et al[15] demonstrated that LASD contributed to pain relief after surgery. Both MIDLF and MIS-TLIF significantly improved the distance between the L1 axis and S1 after the operation, reducing the extra load caused by postoperative gravity compensation and eventually benefiting the restoration of sagittal balance. The improvements in LL and Lower LL, the reduction of spondylolisthesis, and the restoration of intervertebral height might be the factors that make a contribution to the improvement of LASD. Furthermore, we found that ΔLASD in the MIS-TLIF group was significantly larger than ΔLASD in the MIDLF, which might indicate that MIS-TLIF has a better ability to improve LASD.
The improved sagittal lumbar parameters could also reduce the compensation of PT. In our practice, MIDLF had a certain impact on the sagittal pelvic parameters, while MIS-TLIF made a limited difference. The results showed that SS significantly increased and PT significantly decreased after surgery in the MIDLF group. Notably, both groups acquired better PI-LL values compared to pre-operation. Some studies on fusion surgery have reported an improvement in sagittal lumbar parameters to some extent in the treatment of lumbar degenerative diseases, among which open-transforaminal lumbar interbody fusion (O-TLIF) could significantly improve LL and the intervertebral height; however, the improvement of pelvic parameters remains controversial[16]. Certain studies have also indicated that O-TLIF could significantly improve pelvic parameters, such as SS and PT, but others do not support this conclusion[17,18]. Considering MIS-TLIF, although some scholars contended that the minimally invasive approach will limit its ability to improve sagittal lumbar-pelvic parameters, previous studies found that it could still improve LL and pelvic parameters[19,20]. Champagne et al[21] demonstrated that, although the incision made during MIS-TLIF is significantly smaller than that made during O-TLIF, it was not inferior to TLIF for improving sagittal parameters. However, Hawasli et al[22] argued the short-segment MIS-TLIF does not affect the radiological pelvic parameters. Our results seem to concur with the results of Hawasli et al. Since the anchorage length of CBT screws in MIDLF is relatively shorter than that of the traditional pedicle screws in MIS-TLIF, the control force of the anterior column in MIDLF would be weaker than that during MIS-TLIF from a biomechanical perspective. However, we found a significantly superior position of MIDLF to MIS-TLIF in the improvement of the sagittal pelvic parameters, which confirmed that MIDLF could achieve excellent stability. Although the improvement of spinal sagittal alignment was important, it might not be the main purpose in the long term for short-segment lumbar fusion[23]. The relief of patients’ primary symptoms tended to depend more on the exact intraoperative decompression and the stability of internal fixation.
In terms of clinical outcomes, the patients in both groups showed improved VAS and ODI scores at three months after surgery and the final follow-up compared to those recorded prior to operation, although the mean ODI score in the MIDLF group at three months after surgery was slightly higher than that in the MIS-TLIF group, which might be attributable to a greater proportion of lumbar disc herniation cases in the MIS-TLIF group than the MIDLF group. The symptoms of lumbar disc herniation would be relieved better in the short term than those of other diseases, such as lumbar spinal stenosis.
This study has some limitations that warrant discussion. First, this was a single-cohort retrospective study, so it might be underpowered, limiting its ability to detect many changes. Second, the study contained a small sample size, and some patients with missing imaging data were excluded, which could have caused some selection bias. Furthermore, the follow-up time was short and long-term imaging data were lacking, which are necessary to continue the follow-up investigation.
Short-segment MIDLF and MIS-TLIF can equally improve sagittal lumbar parameters such as LL, Lower LL, L5I, and LASD in the treatment of lumbar degenerative diseases. However, MIDLF had a better ability than MIS-TLIF to improve pelvic parameters.
The impact of single-segment midline lumbar fusion (MIDLF) on sagittal lumbar-pelvic alignment for management of degenerative lumbar diseases is still unknown.
Comparing the impact of MIDLF and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) on sagittal lumbar-pelvic parameters can help to better understand minimally invasive lumbar surgery.
To compare the effects of single-segment MIDLF and MIS-TLIF on sagittal lumbar-pelvic parameters.
We retrospectively analyzed 63 patients with degenerative lumbar diseases who underwent single-segment MIDLF or MIS-TLIF. The sagittal lumbar-pelvic parameters and clinical outcomes of the two groups were compared.
Both MIDLF and MIS-TLIF can improve lumbar lordosis (LL), lower LL, L5 incidence (L5I), and L1 axis and S1 distance (LASD). Nevertheless, MIDLF showed a better ability to improve pelvic parameters than MIS-TLIF. However, there was no significant difference between the two groups in terms of clinical outcomes at the final follow-up.
Short-segment MIDLF and MIS-TLIF can equally improve sagittal lumbar parameters such as LL, Lower LL, L5I, and LASD in the treatment of lumbar degenerative diseases. However, MIDLF had a larger impact on pelvic parameters than MIS-TLIF.
MIDLF is a good choice for the treatment of short-segment degenerative lumbar diseases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fakhradiyev I, Kazakhstan; Zou Y, China S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Schnake KJ, Rappert D, Storzer B, Schreyer S, Hilber F, Mehren C. [Lumbar fusion-Indications and techniques]. Orthopade. 2019;48:50-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Teng I, Han J, Phan K, Mobbs R. A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci. 2017;44:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 160] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 3. | Kim CH, Easley K, Lee JS, Hong JY, Virk M, Hsieh PC, Yoon ST. Comparison of Minimally Invasive Versus Open Transforaminal Interbody Lumbar Fusion. Global Spine J. 2020;10:143S-150S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 4. | Li F, Li C, Xi X, Zeng Z, Ma B, Xie N, Wang H, Yu Y, Cheng L. Distinct fusion intersegmental parameters regarding local sagittal balance provide similar clinical outcomes: a comparative study of minimally invasive vs open transforaminal lumbar interbody fusion. BMC Surg. 2020;20:97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Su K, Luan J, Wang Q, Yang Y, Mei W, Zhang Z. Radiographic Analysis of Minimally Invasive Transforaminal Lumbar Interbody Fusion vs Conventional Open Surgery on Sagittal Lumbar-Pelvic Alignment for Degenerative Spondylolisthesis. World Neurosurg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Hoffman H, Verhave B, Jalal MS, Beutler T, Galgano MA, Chin LS. Comparison of Cortical Bone Trajectory Screw Placement Using the Midline Lumbar Fusion Technique to Traditional Pedicle Screws: A Case-Control Study. Int J Spine Surg. 2019;13:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Crawford CH 3rd, Owens RK 2nd, Djurasovic M, Gum JL, Dimar JR 2nd, Carreon LY. Minimally-Invasive midline posterior interbody fusion with cortical bone trajectory screws compares favorably to traditional open transforaminal interbody fusion. Heliyon. 2019;5:e02423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Momin AA, Steinmetz MP. Evolution of Minimally Invasive Lumbar Spine Surgery. World Neurosurg. 2020;140:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 9. | Matsukawa K, Yato Y. Lumbar pedicle screw fixation with cortical bone trajectory: A review from anatomical and biomechanical standpoints. Spine Surg Relat Res 2017; 1: 164-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Shin MH, Ryu KS, Hur JW, Kim JS, Park CK. Comparative study of lumbopelvic sagittal alignment between patients with and without sacroiliac joint pain after lumbar interbody fusion. Spine (Phila Pa 1976). 2013;38:E1334-E1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Kepler CK, Rihn JA, Radcliff KE, Patel AA, Anderson DG, Vaccaro AR, Hilibrand AS, Albert TJ. Restoration of lordosis and disk height after single-level transforaminal lumbar interbody fusion. Orthop Surg. 2012;4:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Marouby S, Coulomb R, Maury E, Assi C, Mares O, Kouyoumdjian P. Prospective Evaluation of Spino-Pelvic Parameters with Clinical Correlation in Patients Operated with an Anterior Lumbar Interbody Fusion. Asian Spine J. 2020;14:88-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Ohba T, Ebata S, Oba H, Koyama K, Haro H. Correlation Between Postoperative Distribution of Lordosis and Reciprocal Progression of Thoracic Kyphosis and Occurrence of Proximal Junctional Kyphosis Following Surgery for Adult Spinal Deformity. Clin Spine Surg. 2018;31:E466-E472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Elmekaty M, Kotani Y, Mehy EE, Robinson Y, Tantawy AE, Sekiguchi I, Fujita R. Clinical and Radiological Comparison between Three Different Minimally Invasive Surgical Fusion Techniques for Single-Level Lumbar Isthmic and Degenerative Spondylolisthesis: Minimally Invasive Surgical Posterolateral Fusion vs Minimally Invasive Surgical Transforaminal Lumbar Interbody Fusion vs Midline Lumbar Fusion. Asian Spine J. 2018;12:870-879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Funao H, Tsuji T, Hosogane N, Watanabe K, Ishii K, Nakamura M, Chiba K, Toyama Y, Matsumoto M. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J. 2012;21:2181-2187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 16. | Recnik G, Košak R, Vengust R. Influencing segmental balance in isthmic spondylolisthesis using transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2013;26:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Feng Y, Chen L, Gu Y, Zhang ZM, Yang HL, Tang TS. Influence of the posterior lumbar interbody fusion on the sagittal spino-pelvic parameters in isthmic L5-S1 spondylolisthesis. J Spinal Disord Tech. 2014;27:E20-E25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Ould-Slimane M, Lenoir T, Dauzac C, Rillardon L, Hoffmann E, Guigui P, Ilharreborde B. Influence of transforaminal lumbar interbody fusion procedures on spinal and pelvic parameters of sagittal balance. Eur Spine J. 2012;21:1200-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Massie LW, Zakaria HM, Schultz LR, Basheer A, Buraimoh MA, Chang V. Assessment of radiographic and clinical outcomes of an articulating expandable interbody cage in minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis. Neurosurg Focus. 2018;44:E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 20. | Rajakumar DV, Hari A, Krishna M, Sharma A, Reddy M. Complete anatomic reduction and monosegmental fusion for lumbar spondylolisthesis of Grade II and higher: use of the minimally invasive "rocking" technique. Neurosurg Focus. 2017;43:E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Champagne PO, Walsh C, Diabira J, Plante MÉ, Wang Z, Boubez G, Shedid D. Sagittal Balance Correction Following Lumbar Interbody Fusion: A Comparison of the Three Approaches. Asian Spine J. 2019;13:450-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 22. | Hawasli AH, Khalifeh JM, Chatrath A, Yarbrough CK, Ray WZ. Minimally invasive transforaminal lumbar interbody fusion with expandable vs static interbody devices: radiographic assessment of sagittal segmental and pelvic parameters. Neurosurg Focus. 2017;43:E10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 94] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 23. | Jia J, Zhao Y, Liu X. Impact of sagittal imbalance correction on clinical outcomes in patients undergoing MIS-TLIF for LSS. Clin Neurol Neurosurg. 2019;181:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |