Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12793
Peer-review started: October 4, 2022
First decision: October 21, 2022
Revised: November 2, 2022
Accepted: November 8, 2022
Article in press: November 8, 2022
Published online: December 6, 2022
Processing time: 59 Days and 2.8 Hours
Endoscopic submucosal dissection (ESD) is the treatment of choice for early gastric cancer and premalignant gastric dysplasia. In some cases, ESD induced ulcer heals as a polypoid nodular scar (PNS). These scars may make the physicians raise several clinical implications such as post-ESD neoplastic recurrence.
We described a case of gastric ESD induced PNS which is regressed after Helicobacter pylori (H. pylori) eradication. A 58-year-old male patient was referred to the outpatient clinic for evaluation and treatment of gastric low-grade dysplasia (LGD). ESD was performed. A PNS was developed at the ESD site. An endoscopic biopsy was done and there was no histological evidence of remnant tumor or recurrence but a hyperplastic mucosal change. The PNS showed increase in size in follow-up endoscopy, and the biopsy specimen demonstrated H. pylori infestation. H. pylori eradication was done and the PNS was regressed.
H. pylori eradication is considerable for the regression of PNS if H. pylori infesta
Core Tip: We report a case of gastric endoscopic submucosal dissection induced polypoid nodular scar and regression after Helicobacter pylori eradication.
- Citation: Jin BC, Ahn AR, Kim SH, Seo SY. Regression of gastric endoscopic submucosal dissection induced polypoid nodular scar after Helicobacter pylori eradication: A case report. World J Clin Cases 2022; 10(34): 12793-12798
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12793.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12793
Endoscopic submucosal dissection (ESD) is the preferred treatment of choice for patients with early gastric cancer (EGC) or premalignant lesions such as gastric dysplasia[1]. It enables minimally invasive and organ-sparing en-bloc resection of the tumor lesions with invasion limited to the mucosal or submucosal layer and with little or no lymph node metastasis. After a curative gastric ESD, typically homogenous and whitish scar change is found on the ESD site. However, in some cases, particularly with lesions located in the antrum of the stomach, the hyperemic polypoid nodular overgrowths of mucosa have been noted after ESD[2,3]. Though the exact mechanism that causes polypoid nodular scar (PNS) is unknown, one study found that 57% of PNS cases were Helicobacter pylori (H. pylori) positive, implying a link between H. pylori infestation and PNS[4]. Herein, we present a case of gastric ESD induced PNS and regression after H. pylori eradication. This case report was approved by the Institutional Review Board of Jeonbuk National University Hospital (IRB No. 2022-07-028), and the patient has signed informed consent to the publication of the case.
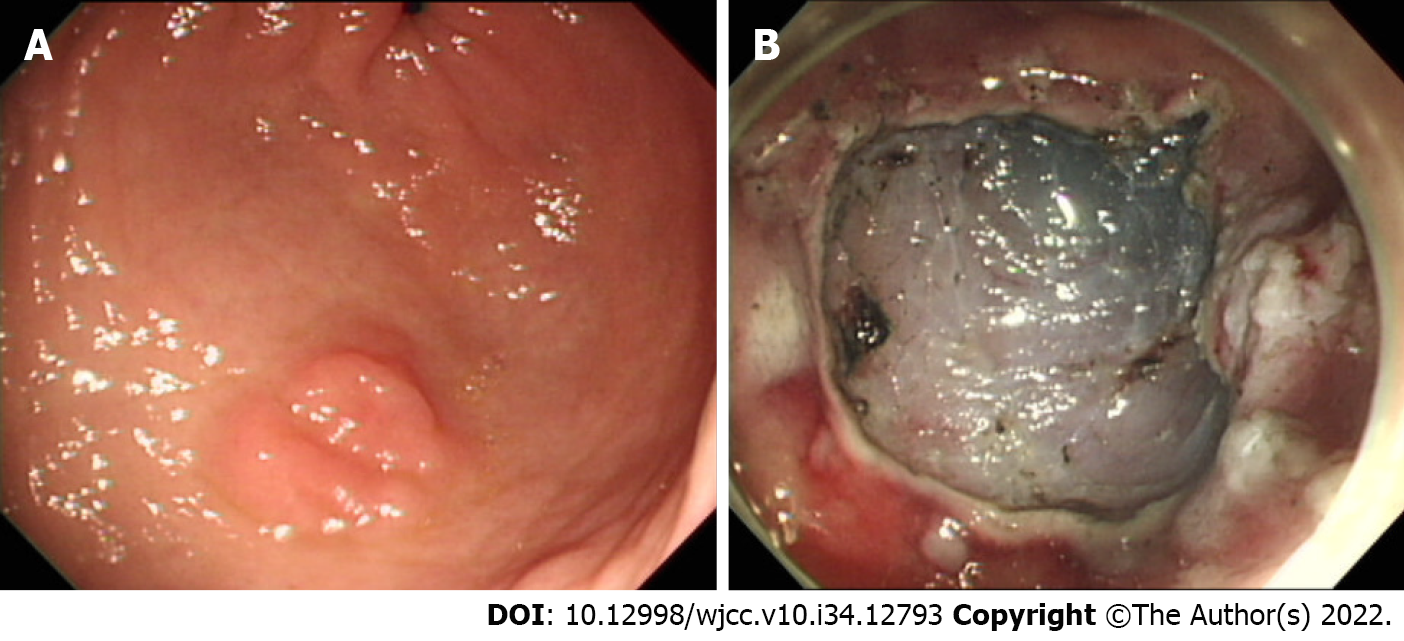
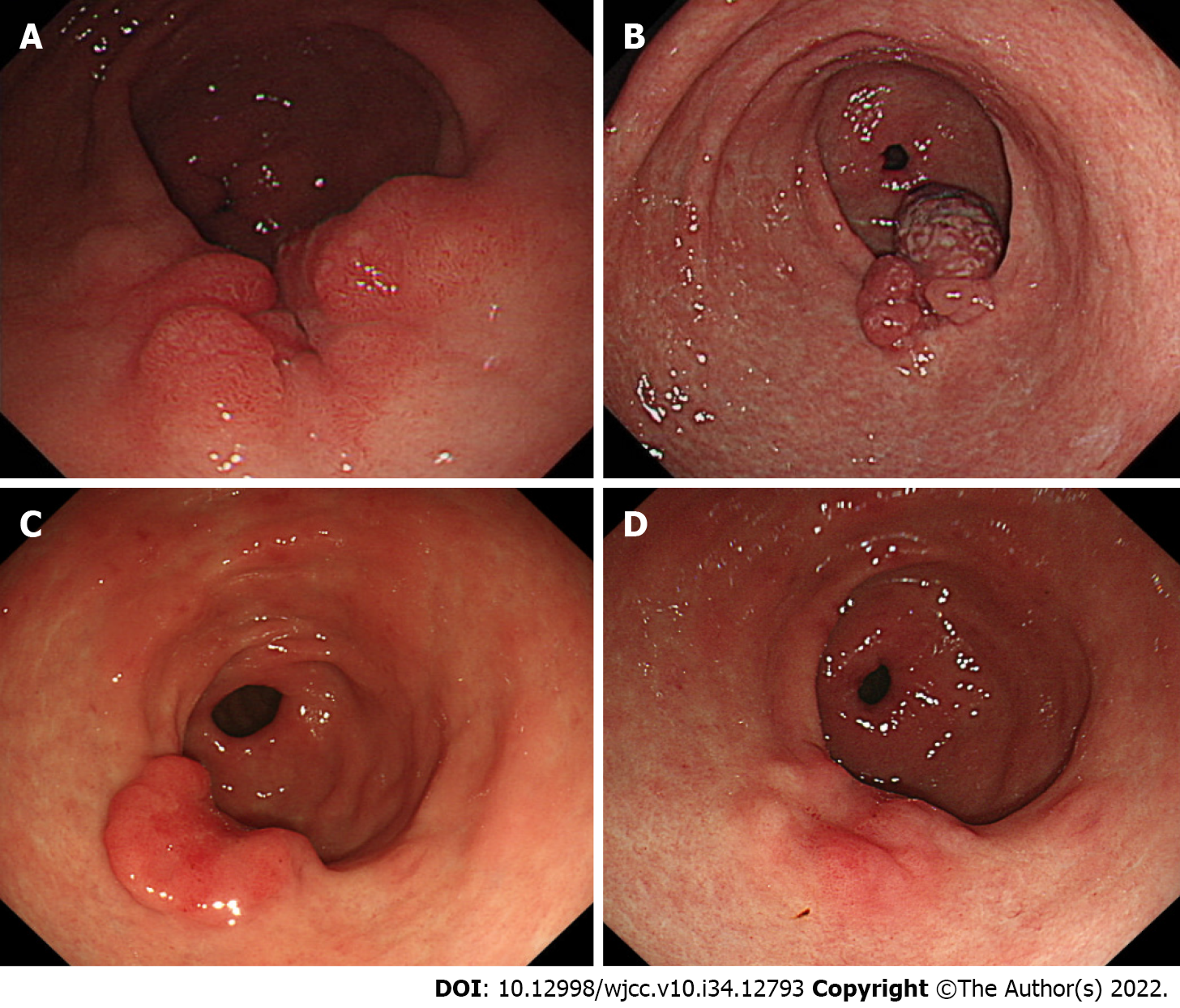
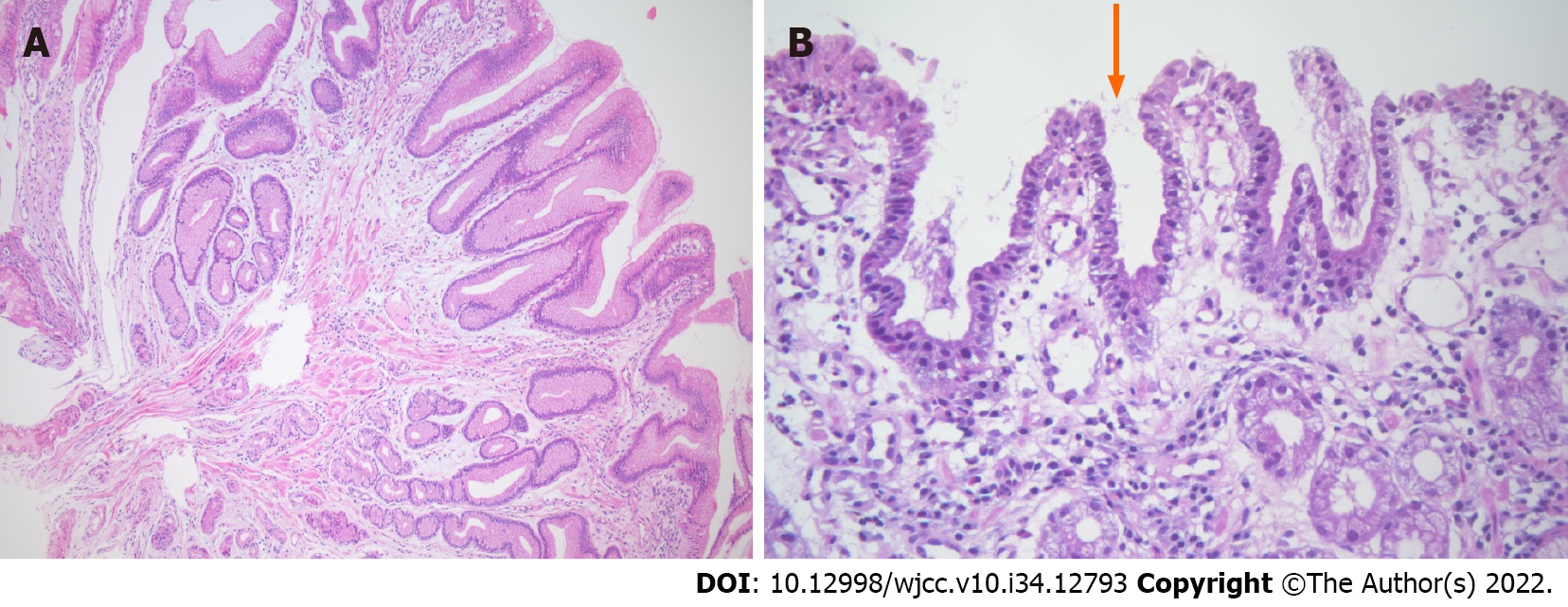
Esophagogastroduodenoscopy showed an elevated nodule of about 2 cm in diameter at the greater curvature side of the antrum, and it was histologically confirmed as LGD. ESD was performed without any complications such as perforation and bleeding (Figure 1). Post-ESD histologic findings showed curative resection. Proton pump inhibitor (esomeprazole 40 mg) was prescribed for the healing of iatrogenic gasrtric ulcer during 8 wk after ESD. A follow-up endoscopy was done after 3 mo and demonstrated a PNS on the previous ESD site (Figure 2A). An endoscopic biopsy was done and the result revealed a hyperplastic polyp. (Figure 3A). After a year, a follow-up esophagogastroduodenoscopy was done and found that the size of the PNS was larger than that of the previous esophagogastroduodenoscopy (Figure 2B). Biopsy was done and Helicobacter gastritis without dysplasia was confirmed (Figure 3B).
His laboratory evaluation revealed just a moderate rise (177 IU/L) of gamma-glutamyl peptidase.
Physical examination was unremarkable, and his abdomen was soft, nontender, and nondistended with no palpable mass.
His alcoholic history was notable, consuming about 2 pints of vodka per day, for 5-6 d in a week, with years of alcohol misuse.
A year before his first presentation, he was diagnosed with hypertension, type II diabetes, and left. Aldosterone-secreting adenoma, for which he received laparoscopic left adrenalectomy.
He denied having any accompanying symptoms.
A 58-year-old male patient was referred to our hospital for treatement of low-grade dysplasia (LGD) at the antrum of the stomach.
The patient received a final diagnosis of gastric ESD induced PNS which is associated with H. pylori infestation.
The patient was treated with the concomitant therapy (Lansoprazole 30 mg 1T bid + Amoxicillin 500 mg 2T bid + Clarithromycin 500 mg 1T bid + Metronidazole 250 mg 2T bid for 10 d) for H. pylori eradication. H. pylori eradication was assessed by a urea breath test.
Endoscopy was performed after 1 year of H. pylori eradication and revealed a significant decrease in the size of the PNS (Figure 2C). After two years of H. pylori eradication, the PNS was regressed (Figure 2D).
PNS, a protuberant polypoid nodule, which develops 3 to 18 mo after ESD mostly in the gastric antrum, is prevalent in men[2]. The incidence of PNS is not yet known due to its uncertainty during the follow-up, but a multi-centered study by Arantes et al[3] reports it to vary broadly from 1.7% to 13.3%. The mechanism of development of PNS is not fully understood. The healing process of post-ESD ulcers is thought to include the continuous growth of gastric mucosa and the convergence of folds at the ulcer rim[5]. This ulcer healing causes a progressive decrease in the size of the polypoid lesion, which eventually heals as a homogeneous, whitish flat scar after 8 wk, for which an oral proton pump inhibitor is administered following ESD[4]. However, the accelerated mucosal repair and pulling-out phenomenon of ulcer rim are suspected to contribute to the nodular overgrowth of mucosa and the development of PNS. Approximately 18% of the diagnosed PNS eventually disappeared, but the rest remained in various sizes[4]. A distinctive characteristic of PNS is its location, predominantly in the distal stomach such as the antrum, probably due to the locally thicker submucosal layer, generating more frequent inflammatory and regenerative reactions compared with other parts of the stomach[3].
There appear to be two primary clinical quandaries to resolve in PNS following the ESD operation. The first is the possibility of recurrence or persistent carcinoma following EGC removal; the second is the difficulty in distinguishing it from intramucosal carcinoma. However, in the studies undertaken by Arentes et al[4], all PNS cases located in the antrum exhibited no histological evidence of tumor recurrence but a hyperplastic alteration with intestinal metaplasia if curative resection was performed. In our case as wee, PNS developed after ESD showed the biopsy-confirmed hyperplastic mucosal change.
In a study by Nam et al[6], which included 183 patients for an average follow-up of 2.2 years, 83.7% of hyperplastic polyps had disappeared by the time H. pylori eradication was completed; without eradication, only 16.3% of polyps disappeared, and there were even cases where the size increased and removal was considered. H. pylori induces epidermal cell proliferation and foveolar hyperplasia, resulting in hyperplastic polyp. These hyperplastic polyps regress after eradiacation, with improvement in gastric mucosal inflammation[7]. Therefore, a successful eradication of H. pylori is thought to reduce the risk of developing hyperplastic polyp[8]. This demonstrates that the development of gastric hyperplastic polyp is associated with H. pylori infection at some instant and that the polyp regresses after eradication, as did with our case. Although reports on the relation between PNS and H. pylori are rare, as long as the biopsy of ESD induced PNS is histologically verified as benign and hyperplastic, H. pylori eradication should regress the nodule, as current guidelines indicate for stomach hyperplastic polyps[6]. Furthermore, the 2020 Korean guidelines for the treatment of H. pylori recommend eradication after the endoscopic resection of H. pylori-positive gastric tumors, including EGC and adenoma, because a lower rate of metachronous cancer recurrence was reported with the eradicated group[9]. Considering this clinical aspect, H. pylori eradication for ESD-induced PNS is reasonable in our case.
We present a case of ESD-induced PNS which was regressed after H. pylori eradication. Although reports on the relationship between PNS and H. pylori infection are rare and further study is needed to define it, the H. pylori eradication may be helpful for the PNS to regress. With the reduction of further injury to the gastric mucosa and less gastrointestinal morbidity, the prospective management of H. pylori could reduce the physician’s concerns for remnant or recurred tumors along with unnecessary endoscopic surveillance in patients with gastric ESD induced PNS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chiba H, Japan; Gao YL, China; Li P, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Park CH, Yang DH, Kim JW, Kim JH, Min YW, Lee SH, Bae JH, Chung H, Choi KD, Park JC, Lee H, Kwak MS, Kim B, Lee HJ, Lee HS, Choi M, Park DA, Lee JY, Byeon JS, Park CG, Cho JY, Lee ST, Chun HJ. Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer. Clin Endosc. 2020;53:142-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 2. | Arantes V, Uedo N, Salgado Pedrosa M. Polypoid nodular scar after endoscopic submucosal dissection in the gastric antrum. Rev Gastroenterol Mex. 2017;82:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Arantes V, Uedo N, Pedrosa MS, Tomita Y. Clinical relevance of aberrant polypoid nodule scar after endoscopic submucosal dissection. World J Gastrointest Endosc. 2016;8:628-634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Arantes V, Uedo N, Morita Y, Toyonaga T, Nakano Y, Pedrosa MS, Oda I, Saito Y, Suzuki H, Yamamoto K, Sato Y, Draganov PV. Polypoid nodule scar after gastric endoscopic submucosal dissection: results from a multicenter study. Endosc Int Open. 2018;6:E1198-E1203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Naomi Kakushima NY, Mitsuhiro Fujishiro, Atsushi Imagawa, Masashi Oka, Katsuya Kobayashi, Takuhei Hashimoto, Touru Motoi, Masao Omata. The Healing Process of Gastric Artificial Ulcers After Endoscopic Submucosal Dissection (JPN). Gastrointestinal Endoscopy. 2004;59. [DOI] [Full Text] |
| 6. | Nam SY, Park BJ, Ryu KH, Nam JH. Effect of Helicobacter pylori eradication on the regression of gastric polyps in National Cancer Screening Program. Korean J Intern Med. 2018;33:506-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Yasunaga Y, Shinomura Y, Kanayama S, Higashimoto Y, Yabu M, Miyazaki Y, Kondo S, Murayama Y, Nishibayashi H, Kitamura S, Matsuzawa Y. Increased production of interleukin 1 beta and hepatocyte growth factor may contribute to foveolar hyperplasia in enlarged fold gastritis. Gut. 1996;39:787-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Nam SY, Park BJ, Ryu KH, Nam JH. Effect of Helicobacter pylori infection and its eradication on the fate of gastric polyps. Eur J Gastroenterol Hepatol. 2016;28:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Jung HK, Kang SJ, Lee YC, Yang HJ, Park SY, Shin CM, Kim SE, Lim HC, Kim JH, Nam SY, Shin WG, Park JM, Choi IJ, Kim JG, Choi M; Korean College of Helicobacter and Upper Gastrointestinal Research. Evidence-Based Guidelines for the Treatment of Helicobacter pylori Infection in Korea 2020. Gut Liver. 2021;15:168-195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 90] [Article Influence: 22.5] [Reference Citation Analysis (0)] |