Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.12036
Peer-review started: August 16, 2022
First decision: September 5, 2022
Revised: September 17, 2022
Accepted: October 13, 2022
Article in press: October 13, 2022
Published online: November 16, 2022
Processing time: 83 Days and 19.4 Hours
Root canal variations frequently occur in maxillary first molars, which greatly affects the success of its treatment. The second mesiobuccal (MB) root canal is the most common root canal variation. However, only a few studies have been con
A 39-year-old woman complained of pain in the maxillary right region for 1 year, which recently worsened. Clinical examination revealed a poorly restored right maxillary first molar and caries detected at the filling marginal. Cold and heat test results indicated severe pain in the right maxillary first molar. The patient was diagnosed with irreversible pulpitis, and subsequently, root canal treatment (RCT) was performed. In total, five root canals were found in the maxillary first molar, including two separate root canals in the palatal root. RCT was suc
An endodontic microscope and CBCT are useful in effectively identifying and treating root canal variations.
Core Tip: This report presents a case of non-surgical root canal treatment of the right maxillary first molar. Five root canals were identified in the maxillary first molar, including two separate root canals in the palatal root. Endodontic microscope and cone-beam computed tomography were helpful in the localization and treatment of complex canal variations.
- Citation: Chen K, Ran X, Wang Y. Endodontic treatment of the maxillary first molar with palatal canal variations: A case report and review of literature. World J Clin Cases 2022; 10(32): 12036-12044
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/12036.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.12036
Root canal treatment (RCT) is currently the most widely used endodontic procedure and has been effective against apical periodontitis and pulpitis. Furthermore, RCT is performed to completely treat the infection in the root canals and seal canals tightly to preserve the affected tooth. However, this procedure can also fail due to inadequate removal of the infected pulp, insufficient filling, or missed root canals due to anatomical variations[1]. Therefore, the diagnosis and localization of variant root canals are crucial to RCT's success.
In general, maxillary first molars have three roots, but their root canal structures vary greatly. The most common root canal variation is the presence of a second mesiobuccal (MB2) canal, resulting in four root canals in the maxillary first molars[2]. Current extensive studies are focused on MB2 canals. The incidence of MB2 canals is high (> 50%) but varies among different ethnic groups[3-5]. Another common root canal variation in maxillary first molars is C-shaped root canals, which can be located in mandibular molars, first premolars, or maxillary molars and usually in mandibular second molars[6]. Furthermore, the incidence of C-shaped root canals in maxillary molars is approximately 1.8%[7], of which are in maxillary first molars (0.091%–0.8%)[7,8]. However, the second palatal root or the second palatal root canal in maxillary molars are extremely rare. In 1981, Stone and Stroner[9] first proposed the palatal root variations of maxillary molars. The maxillary first molars have complex palatal root canal morphology. For example, a single palatal root has two separate canals, or two separate palatal roots have one canal each. According to Qun et al[10], the incidence of palatal root variation in maxillary molars is only 1.4%. Examining the internal morphology of the root canal system is a major part of planning and implementing RCT, in which palatal canal variations should be considered.
At present, advanced technology and machines have been useful in clinical and dental treatments. In particular, the cone-beam computed tomography (CBCT) and the endodontic microscope have greatly improved the therapeutic effect of RCT.
This case report presents the non-surgical RCT of the right maxillary first molar with palatal canal variations, performed using an endodontic microscope and CBCT.
A 39-year-old woman presented to the Department of Adult Dentistry for endodontic treatment. The chief complaint of the patient was pain in the maxillary right region for the past 1 year.
The patient reported occasional pain in the maxillary right region for 1 year. Three months prior to visiting our department, she had received tooth-filling treatment for the right maxillary first molar from another clinic. Recently, the patient experienced severe pain that occurred under hot or cold stimulation.
The patient had received tooth-filling treatment of the right maxillary first and second molars.
The patient denied any history of systemic diseases and allergies.
Clinical examination revealed a class II resin filling on the right maxillary first molar, with caries detected at the filling margin. All cold and heat tests revealed severe pain in the right maxillary first molar.
No laboratory examinations were necessary.
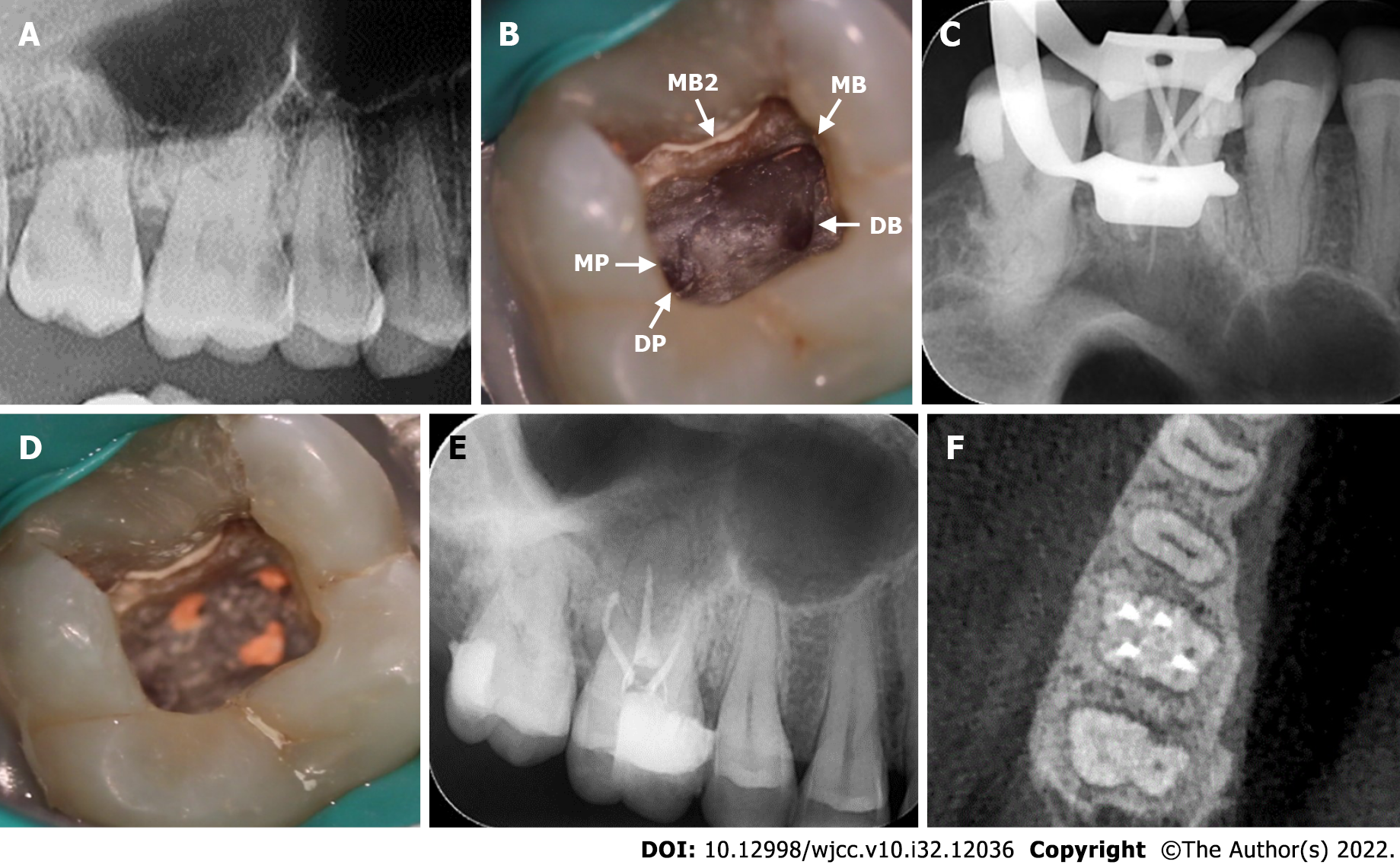
A preoperative digital panoramic radiograph taken 3 mo ago revealed carious lesions in the mesio-occlusion of the right maxillary first molar, which was close to the pulp (Figure 1A).
A diagnosis of irreversible pulpitis of the right maxillary first molar was made. The treatment recommendations included RCT and follow-up crown restoration. Subsequently, the treatment regimen was explained to the patient, and the patient's consent was obtained.
The carious lesion was removed using bur and a high-speed handpiece, and the pulp was exposed following the administration of 4 mL of 2% lidocaine as a local anesthetic (Produits Dentaires Pierre Rolland, Merignac, France). After rubber dam (Coltene, Altstatten, Switzerland) isolation, a routine RCT procedure was performed. The pulp chamber was opened, and an access cavity was prepared. Under the endodontic microscope (OPMI® Pico Zeiss, Carl Zeiss Meditec AG, Jena, Germany), the following four root canals were explored: MB, MB2, distobuccal (DB), and distopalatal (DP) canals (Figure 1B). In addition, unusual anatomical location of the root canal orifices were observed; the canal orifice of the DP canal was not located in the middle corresponding to the MB and DB canals. Under the endodontic microscope, the pulp chamber floor was carefully probed with a DG-16 explore (KaVo, Biberach, Germany), and a suspected fifth canal was discovered, which was named the mesiopalatal (MP) canal (Figure 1B). All treatment procedures were performed with an endodontic microscope with 10 × to 30 × magnification.
In the DP canal, calcification was detected at the apical region, and the canal was dredged with 17% ethylenediaminetetraacetic acid solution (Pulpdent Corporation, Watertown, United States). The working length of the root canals was measured using an electronic apex locator (Dentsply Propex Pixi™, Ballaigues, Switzerland). The MB, MB2, DB, and DP canals were cleaned with 2.5% NaOCl solution and shaped using a Marc Ⅲ nickel-titanium rotary instrumentation (Bomedent, Changzhou, China). All four canals were thoroughly rinsed using endodontic irrigation tips (VDW EDDY™, Munich, Germany). After drying the root canals, the main gutta-percha (Beijing Dayading, Beijing, China) was used to confirm the working length (Figure 1C). Finally, the root canals of the MB, MB2, DB, and DP were obturated by injectable thermoplasticized gutta-percha technique (B&L-beta Gutta Percha Heating System, Gyeonggi-do, Korea) with AH Plus root canal sealer (Dentsply Detrey GmbH, Konstanz, Germany) (Figure 1D). The postoperative X-ray and CBCT image revealed that the MB, MB2, DB, and DP canals were properly filled (Figure 1E and F).
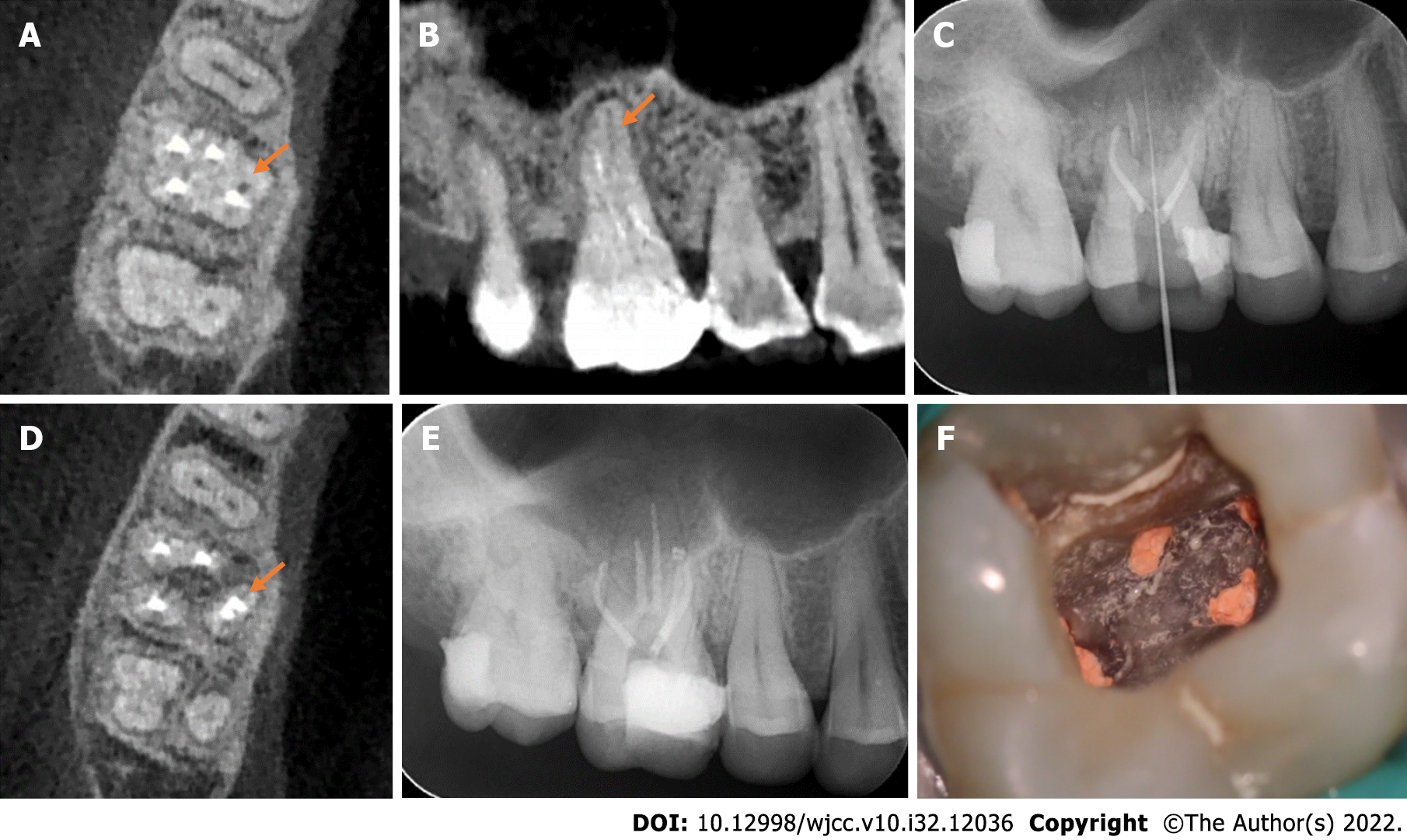
CBCT was performed to accurately assess the anatomical morphology of the MP canal. Moreover, the CBCT image revealed three roots in the right maxillary first molar and well obturated MB, MB2, DB, and DP canals (Figure 2A). However, in the palatal root, an unfilled root canal was identified (Figure 2B). We confirmed the presence of two separate palatal canals in the single palatal root. Next, the working length of the MP canal was measured (Figure 2C). The MP canal was mechanically shaped with a Marc Ⅲ nickel-titanium rotary instrumentation. After careful cleaning using the endodontic irrigation tip, the MP canal was dried with absorbent points. The injectable thermoplasticized gutta-percha technique was used for the obturation of the MP canal. The CBCT image revealed that the two separate root canals were well filled (Figure 2D). Both the X-ray and intraoral photograph revealed that the five canals of the maxillary first molar were well obturated after treatment (Figure 2E and F). Finally, the tooth was restored by resin composite filling.
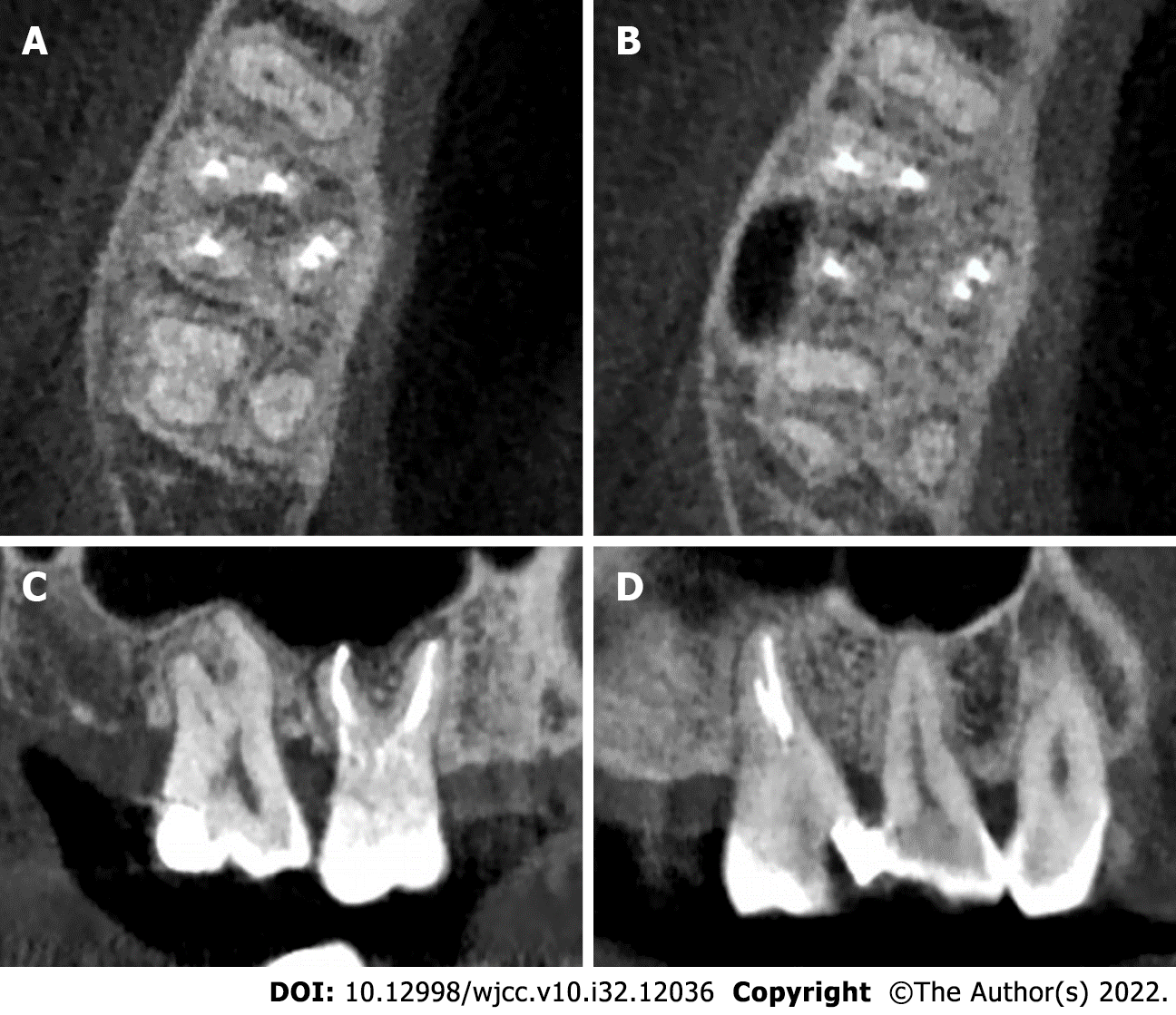
After the RCT, the quality of the obturation in the right maxillary first molar was evaluated using CBCT. The CBCT images revealed that the maxillary first molar contained three roots (MB, DB, and palatal roots; Figure 3A). The axial plane of the CBCT image showed that the MB and DB roots con
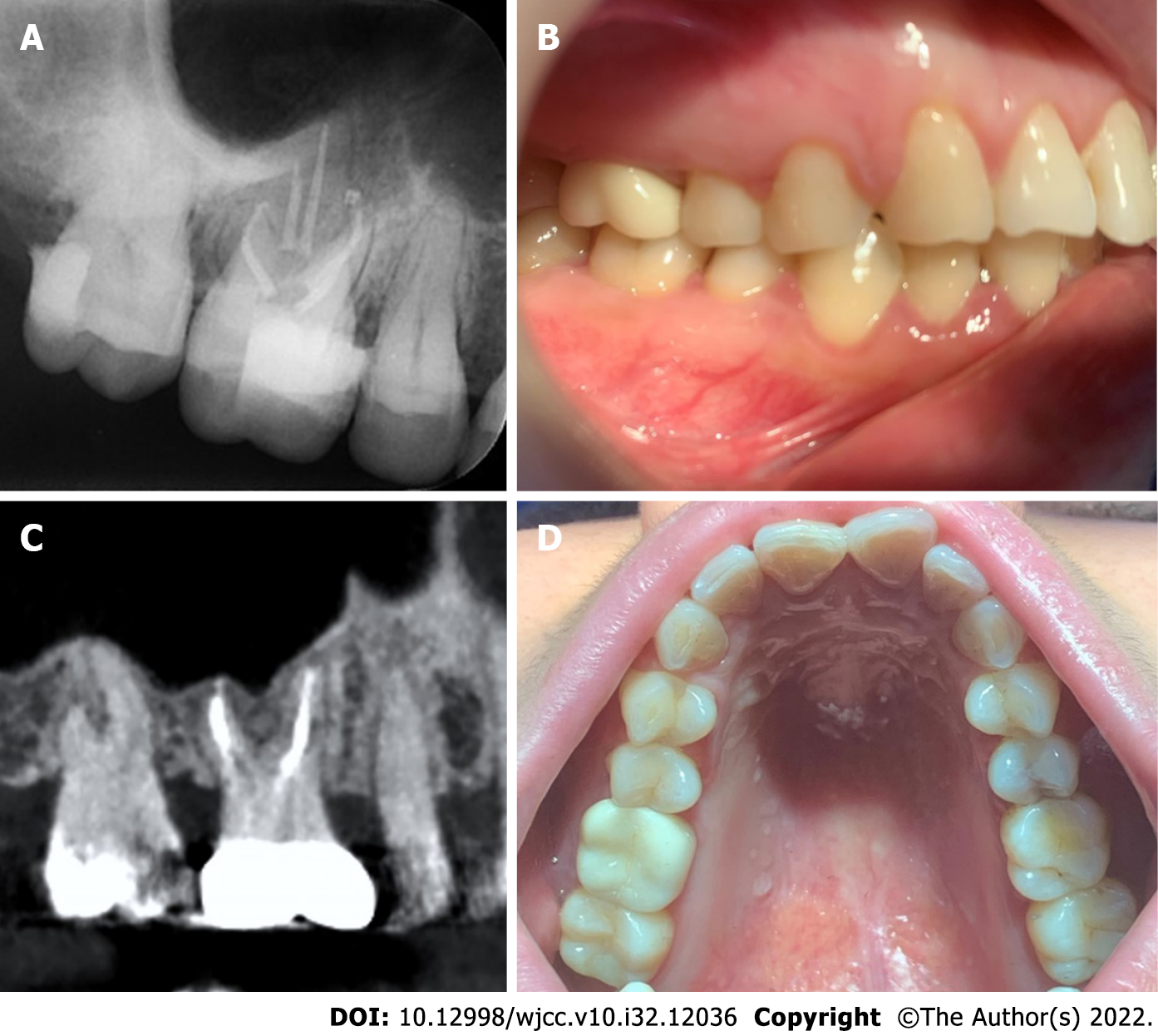
At the 1-mo follow-up, the maxillary first molar was completely asymptomatic, and the X-ray indicated that the RCT was successful (Figure 4A). As a result, tooth preparation and final ceramic crown restoration were performed (Figure 4B). After 9 mo, the tooth was clinically asymptomatic and radiographically sound (Figure 4C and D).
This case report demonstrates the RCT of the maxillary first molar with palatal root variations. Two separate canals were detected in a single palatal root, which indicated a type IV morphology (vertucci classification). Furthermore, both endodontic microscopes and CBCT helped detect root canal variations.
The maxillary first molars erupted earlier, and the pit and fissure morphology was more complicated than that of the front tooth. Thus, caries and apical periodontitis were more common in clinical presentation[11]. RCT, as an effective treatment method, has been widely used in clinical endodontics. In addition to mechanical techniques and new chemical materials, anatomical variations of the teeth should also be considered when improving the success rate of RCT. The most common root canal system of maxillary first molars was three roots with four canals[12]. The DB and palatal roots of maxillary first molars usually have only one root canal, while the MB root has two or more canals system[13,14]. MB2 canals are detected in 30%-95% individuals in different populations[15,16]. Despite the diversity of anatomical variations of maxillary first molars, studies on palatal root variations of maxillary molars are scarce.
The palatal root variations of the maxillary molars were mainly manifested as a single palatal root with double root canals, or two palatal roots with one canal each[9]. The majority of maxillary molars have three roots, although four roots can be detected occasionally, i.e., a second palatal root. Aydın[17] reported that the incidence of two palatal roots in maxillary first and second molars is 0.17% and 1.41%, respectively. However, in the northwestern Chinese population, Gu et al[18] proposed that the incidence of two palatal roots in the maxillary first and second molars was only 0.07% and 0.98%, respectively, suggesting the rarity of the palatal root variations in maxillary molars, especially in the maxillary first molars. Studies in the recent 10 years of maxillary molars with palatal root variations are summarized in Table 1. Majority of the studies suggested that maxillary molars have two palatal roots, and each palatal root has a single root canal[17,19-25]. However, only two reports have described the presence of double root canals in a single palatal root[26,27]. Kottoor et al[26] reported that two root canal orifices were identified in a single palatal root and that the palatal root canal had a type II morphology, while Shahi et al[28] suggested the incidence of a single palatal root of the maxillary first molars with two root canals is 0.73%, indicating a type V canal morphology. Neelakantan et al[29] revealed that the incidence of two root canals in the palatal root of maxillary first molars in the Indian population was 5.4%, of which 4% had a type IV morphology, while the remaining 1.4% had a type V morphology. Zheng et al’s study demonstrated that in the Chinese population, the incidence of two root canals in the palatal root of maxillary first molars was only 1.76%[30]. In this case report, we described the presence of two separate root canals in a single palatal root of the right maxillary first molar. The two palatal root canals demonstrated a type IV morphology, which presented as two separate root orifices extending from the pulp chamber to the apex and with two apical foramina.
| Ref. | Mesiobuccal canal (No.) | Distobuccal canal (No.) | Palatal variations | Molar type | |
| Palatal root (No.) | Palatal root canal (No.) | ||||
| Chakradhar et al[19], 2010 | 1 | 1 | 2 | 2 | Maxillary first molar |
| Kottoor et al[26], 2011 | 3 | 3 | 1 | 2 | Maxillary first molar |
| Fakhari and Shokraneh[20], 2013 | 1 | 1 | 2 | 2 | Maxillary second molar |
| Badole et al[27], 2014 | 3 | 2 | 1 | 2 | Maxillary first molar |
| Wu and Wu[21], 2015 | 1 | 1 | 2 | 2 | Maxillary first molar |
| Asghari et al[22], 2015 | 1 | 1 | 2 | 2 | Maxillary first molar |
| Mohammadzade Akhlaghi et al[23], 2017 | 1 | 1 | 2 | 2 | Maxillary second molar |
| Schryvers et al[24], 2019 | 1 | 1 | 2 | 2 | Maxillary second molar |
| M P et al[25], 2020 | 1 | 1 | 2 | 2 | Maxillary second molar |
| Aydın[17], 2021 | 1 | 1 | 2 | 2 | Maxillary first molar |
The use of endodontic microscopes has greatly contributed to the advancement of endodontic treatment. Through magnification using an endodontic microscope, clinicians can identify root canals that are difficult to locate or overlooked with normal vision. Especially for teeth with complex root canal variations, the endodontic microscope demonstrates superior effectiveness. Studies have reported that the use of endodontic microscopes in RCT can improve the detection rate of MB2 canals, and the 10-year survival rate of teeth treated by endodontists was significantly higher[31,32].
The development of radiographic techniques, especially the application of CBCT, has also been greatly helpful for complex endodontic treatments[33]. Traditional X-rays can only reveal the shape of the roots in two dimensions; however, CBCT can provide a three-dimensional image of the tooth, which can better describe root morphology and locate the anatomical variations in a complex root canal system. CBCT can detect the early stage of periapical lesions and improve tooth preservation through non-surgical treatment[34]. In molars, CBCT also demonstrated a higher detection capability for MB2 and C-shaped canals[3,6]. Through preoperative interpretation of CBCT images, the access cavity can be arranged more reasonably. Postoperative CBCT can also be used to evaluate the outcome of RCT. Shetty et al[35] recently found that CBCT showed potential application in regenerative endodontic procedures. CBCT has proven to be an effective and important assessment tool in endodontic treatment.
In this case, the distance between the orifices of MB and DP canals was shorter than that of MB and DB canals. This unusual situation suggests the possible presence of anatomical variation in the right maxillary first molar. Through careful exploration of the pulp chamber floor with an endodontic explorer, we successfully located the fifth root canal orifice of the palatal root. Although palatal root anatomical variations of the maxillary first molar are uncommon, clinicians should still consider such variations. For unusual root anatomy morphology, careful exploration should be performed with an endodontic microscope and CBCT to avoid missing variant root canals.
Palatal root variations of maxillary first molars, which may present as a single palatal root with two separate root canals, merit attention. Careful exploration of the pulp chamber floor can facilitate the detection of root canal variations. Moreover, endodontic microscopy and CBCT are effective adjunctive techniques for RCT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Arumugam EAP, India; Heboyan A, Armenia; Nath SG, India; Ullah K, Pakistan; Vyshka G, Albania S-Editor: Liu XF L-Editor: A P-Editor: Liu XF
| 1. | Miccoli G, Seracchiani M, Zanza A, Giudice AD, Testarelli L. Possible Complications of Endodontic Treatments. J Contemp Dent Pract. 2020;21:473-474. [PubMed] [DOI] [Full Text] |
| 2. | Tuncer AK, Haznedaroglu F, Sert S. The location and accessibility of the second mesiobuccal canal in maxillary first molar. Eur J Dent. 2010;4:12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Razumova S, Brago A, Khaskhanova L, Barakat H, Howijieh A. Evaluation of Anatomy and Root Canal Morphology of the Maxillary First Molar Using the Cone-Beam Computed Tomography among Residents of the Moscow Region. Contemp Clin Dent. 2018;9:S133-S136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Kim Y, Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a korean population: variations in the number of roots and canals and the incidence of fusion. J Endod. 2012;38:1063-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 5. | Alrahabi M, Sohail Zafar M. Evaluation of root canal morphology of maxillary molars using cone beam computed tomography. Pak J Med Sci. 2015;31:426-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Nejaim Y, Gomes AF, Rosado LPL, Freitas DQ, Martins JNR, da Silva EJNL. C-shaped canals in mandibular molars of a brazilian subpopulation: Prevalence and root canal configuration using cone-beam computed tomography. Clin Oral Investig. 2020;24:3299-3305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Jo HH, Min JB, Hwang HK. Analysis of C-shaped root canal configuration in maxillary molars in a Korean population using cone-beam computed tomography. Restor Dent Endod. 2016;41:55-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | De Moor RJ. C-shaped root canal configuration in maxillary first molars. Int Endod J. 2002;35:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Stone LH, Stroner WF. Maxillary molars demonstrating more than one palatal root canal. Oral Surg Oral Med Oral Pathol. 1981;51:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Qun L, Longing N, Qing Y, Yuan L, Jun W, Qingyue D. A case of asymmetric maxillary second molar with double palatal roots. Quintessence Int. 2009;40:275-276. [PubMed] |
| 11. | Que L, Jia M, You Z, Jiang LC, Yang CG, Quaresma AAD, das Neves EMAA. Prevalence of dental caries in the first permanent molar and associated risk factors among sixth-grade students in São Tomé Island. BMC Oral Health. 2021;21:483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Tzeng LT, Chang MC, Chang SH, Huang CC, Chen YJ, Jeng JH. Analysis of root canal system of maxillary first and second molars and their correlations by cone beam computed tomography. J Formos Med Assoc. 2020;119:968-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Vizzotto MB, Silveira PF, Arús NA, Montagner F, Gomes BP, da Silveira HE. CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molar teeth: Effect of voxel size and presence of root filling. Int Endod J. 2013;46:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Joshi N, Shrestha S, Sundas S, Prajapati K, Devi Wagle S, Gharti A. C-Shaped Canal in Second Molar of Mandible among Cases of Cone Beam Computed Tomography in Tertiary Care Centres: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2021;59:649-652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 15. | Kato A, Inagaki K, Utsumi M, Kato K, Honda M. Micro-computed tomography analysis of the relationship between root canal number and root concavity in maxillary first and second molars in a Japanese population. Odontology. 2021;109:193-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Martins JNR, Marques D, Silva EJNL, Caramês J, Mata A, Versiani MA. Second mesiobuccal root canal in maxillary molars-A systematic review and meta-analysis of prevalence studies using cone beam computed tomography. Arch Oral Biol. 2020;113:104589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 17. | Aydın H. Relationship between crown and root canal anatomy of four-rooted maxillary molar teeth. Aust Endod J. 2021;47:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Gu Y, Wang W, Ni L. Four-rooted permanent maxillary first and second molars in a northwestern Chinese population. Arch Oral Biol. 2015;60:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Chakradhar Raju RV, Chandrasekhar V, Singh CV, Pasari S. Maxillary molar with two palatal roots: Two case reports. J Conserv Dent. 2010;13:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Fakhari E, Shokraneh A. A maxillary second molar with two separate palatal roots: A case report. J Dent (Shiraz). 2013;14:87-89. [PubMed] |
| 21. | Wu D, Wu H. [Maxillary first molar with twin-root canal in palatal side: Two case reports]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2015;33:329-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Asghari V, Rahimi S, Ghasemi N, Talebzadeh B, Norlouoni A. Treatment of a Maxillary First Molar with Two Palatal Roots. Iran Endod J. 2015;10:287-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Mohammadzade Akhlaghi N, Fazlyab M. Treatment of a Four-Rooted Maxillary Second Molar Detected with Cone-Beam Computed Tomography. J Dent (Tehran). 2017;14:100-104. [PubMed] |
| 24. | Schryvers A, Govaerts D, Politis C, Lambrechts P. Endodontic management of a maxillary first molar with two palatal roots: A case report. Aust Endod J. 2019;45:420-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | M P, Sahoo H. Cone Beam Computed Tomography-aided Endodontic Management of Second Maxillary Molar with Two Separate Palatal Roots: A Case Report. Cureus. 2020;12:e7347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 26. | Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: A case report. J Endod. 2011;37:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Badole GP, Warhadpande MM, Shenoi PR, Lachure C, Badole SG. A rare root canal configuration of bilateral maxillary first molar with 7 root canals diagnosed using cone-beam computed tomographic scanning: A case report. J Endod. 2014;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Shahi S, Yavari HR, Rahimi S, Ahmadi A. Root canal configuration of maxillary first permanent molars in an Iranian population. J Dent Res Dent Clin Dent Prospects. 2007;1:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 29. | Neelakantan P, Subbarao C, Ahuja R, Subbarao CV, Gutmann JL. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010;36:1622-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 30. | Zheng QH, Wang Y, Zhou XD, Wang Q, Zheng GN, Huang DM. A cone-beam computed tomography study of maxillary first permanent molar root and canal morphology in a Chinese population. J Endod. 2010;36:1480-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 31. | Khalighinejad N, Aminoshariae A, Kulild JC, Williams KA, Wang J, Mickel A. The Effect of the Dental Operating Microscope on the Outcome of Nonsurgical Root Canal Treatment: A Retrospective Case-control Study. J Endod. 2017;43:728-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Burry JC, Stover S, Eichmiller F, Bhagavatula P. Outcomes of Primary Endodontic Therapy Provided by Endodontic Specialists Compared with Other Providers. J Endod. 2016;42:702-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 33. | Patel S, Durack C, Abella F, Shemesh H, Roig M, Lemberg K. Cone beam computed tomography in Endodontics - a review. Int Endod J. 2015;48:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 223] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 34. | Durack C, Patel S. Cone beam computed tomography in endodontics. Braz Dent J. 2012;23:179-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 35. | Shetty H, Shetty S, Kakade A, Shetty A, Karobari MI, Pawar AM, Marya A, Heboyan A, Venugopal A, Nguyen TH, Rokaya D. Three-dimensional semi-automated volumetric assessment of the pulp space of teeth following regenerative dental procedures. Sci Rep. 2021;11:21914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |