Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.12022
Peer-review started: August 4, 2022
First decision: September 27, 2022
Revised: September 30, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 16, 2022
Processing time: 96 Days and 5.1 Hours
Retroperitoneal leiomyoma is a rare benign tumor. Retroperitoneal leiomyomas located in the latissimus uterine ligament are even rarer. Retroperitoneal leiomyomas have similar characteristics to uterine leiomyomas in terms of tissue, which results in confusion during diagnosis.
A 47-year-old female with 3 years of pain in the right lower quadrant and discovery of a pelvic mass 13 d ago underwent open abdominal exploration. In the right broad ligament, a solid mass with well circumscribed boundaries, approximately 15 cm × 10 cm × 10 cm in size was bluntly peeled off. The pathological result was a spindle cell tumor, morphologically considered to originate from smooth muscle. Immunohistochemical results supported a deep soft tissue leiomyoma.
Retroperitoneal leiomyoma is a rare benign tumor, and surgical treatment can have a good therapeutic effect.
Core Tip: Retroperitoneal leiomyoma is a rare tumor, with more than 100 cases reported. Preoperative diagnosis is difficult, and resection is diagnostic and therapeutic. Our patient was diagnosed with retroperitoneal leiomyoma and underwent surgical treatment with a good outcome.
- Citation: Zhang XS, Lin SZ, Liu YJ, Zhou L, Chen QD, Wang WQ, Li JY. Retroperitoneal leiomyoma located in the broad ligament: A case report. World J Clin Cases 2022; 10(32): 12022-12027
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/12022.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.12022
Leiomyoma is a benign non-epithelial mesenchymal monoclonal tumor that originates in myoblast smooth muscle cells or muscle vessel walls or interstitium composed of fibrous connective tissue[1]. The most common type of these tumors is uterine leiomyomas, most of which are located posterior to the visceral peritoneum (serous membrane) of the uterus and occasionally in the pelvic or posterior peritoneal wall of the abdomen[2]. The signs and symptoms caused by uterine leiomyomas include pain, flatulence, menstrual irregularities, infertility, and uterine bleeding during the postmenopausal period. Retroperitoneal-abdominal leiomyomas are similar to uterine leiomyomas, but are relatively rarer, with more than 100 cases described in the literature since 1941[2]. They consist of elongated smooth muscle cells, occasionally arranged in a cord or reticulated arrangement. Compared to the most common uterine leiomyomas, the pathological features are similar to those of uterine leiomyomas, but the pathogenesis is unclear and the cytogenetics and molecular genetics of the tumor are almost unknown.
Retroperitoneal leiomyomas have similar tissue characteristics[3]. Retroperitoneal leiomyomas and uterine leiomyomas usually both have hyaluronic fibrosis, mucoid changes, or alternating trabecular changes, and are positive for estrogen and progesterone receptors. In addition, they all show low mitosis activity, little or no atypia and necrosis, and the immunohistochemical characteristics are consistent with smooth muscle tumors[2,4,5]. However, estrogen receptors may be strongly expressed in uterine leiomyosarcomas, but are uncommon in retroperitoneal-abdominal leiomyosarcomas and are usually weakly focal[4]. The most common clinical indicator of retroperitoneal leiomyoma compared to uterine leiomyomas is palpation of a pelvic mass, present in almost 90% of patients. Although many symptoms of retroperitoneal leiomyomas are also common in uterine leiomyomas, there are also some important differences. For example, the most common symptoms of uterine leiomyomas are abnormal uterine bleeding, pelvic pain and pressure, while uncommon in retroperitoneal leiomyomas[2].
The patient had pain in the right lower quadrant for 3 years, aggravated recently, and a pelvic mass was found at our outpatient clinic.
The patient had pain in the right lower quadrant three years ago without an obvious precipitating cause, but she did not seek medical advice. The pain was aggravated after activity 2 mo ago, and she was examined in our outpatient clinic 13 d ago.
The patient had previously been in good health.
The patient had 2 pregnancies, 1 birth, and 1 daughter in good health. Her menstrual cycle was regular.
Physical examination revealed no significant abnormalities.
No abnormalities were noted after blood count, routine urine, liver and kidney function, electrolytes, blood glucose, lipids, carcinoembryonic antigen, alpha-fetoprotein, cancer antigen 125 (CA125), and human immunodeficiency virus testing.
Ultrasound results were as follows: preutertal position, approximately 59 cm × 50 cm × 50 cm in size, uneven echo of the uterine muscle wall, unclear contour of the right wall and posterior wall, uneven echo of the endometrium, thickness of 12.5 mm. Color ultrasound examination showed that the right adnexal area demonstrated a mixed echo of 16 cm × 10 cm × 10 cm. It was considered as uterine leiomyoma based to the ultrasound images.
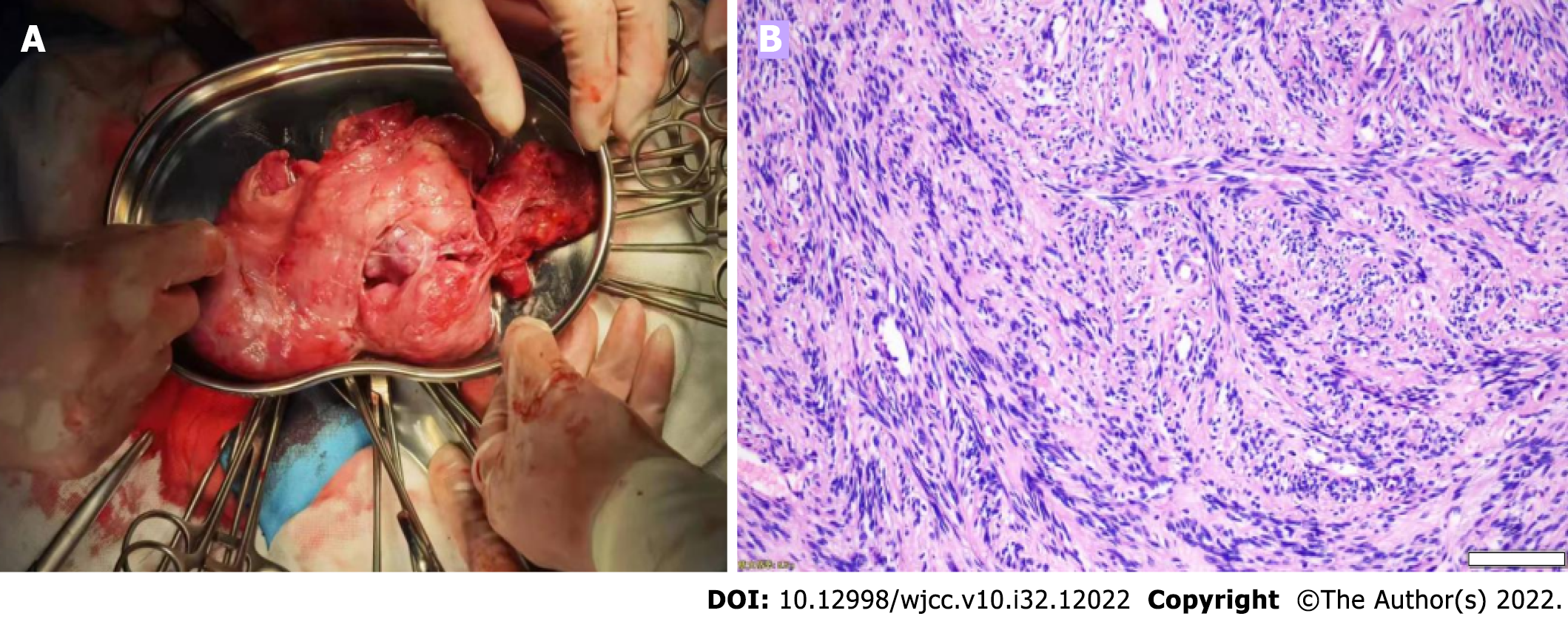
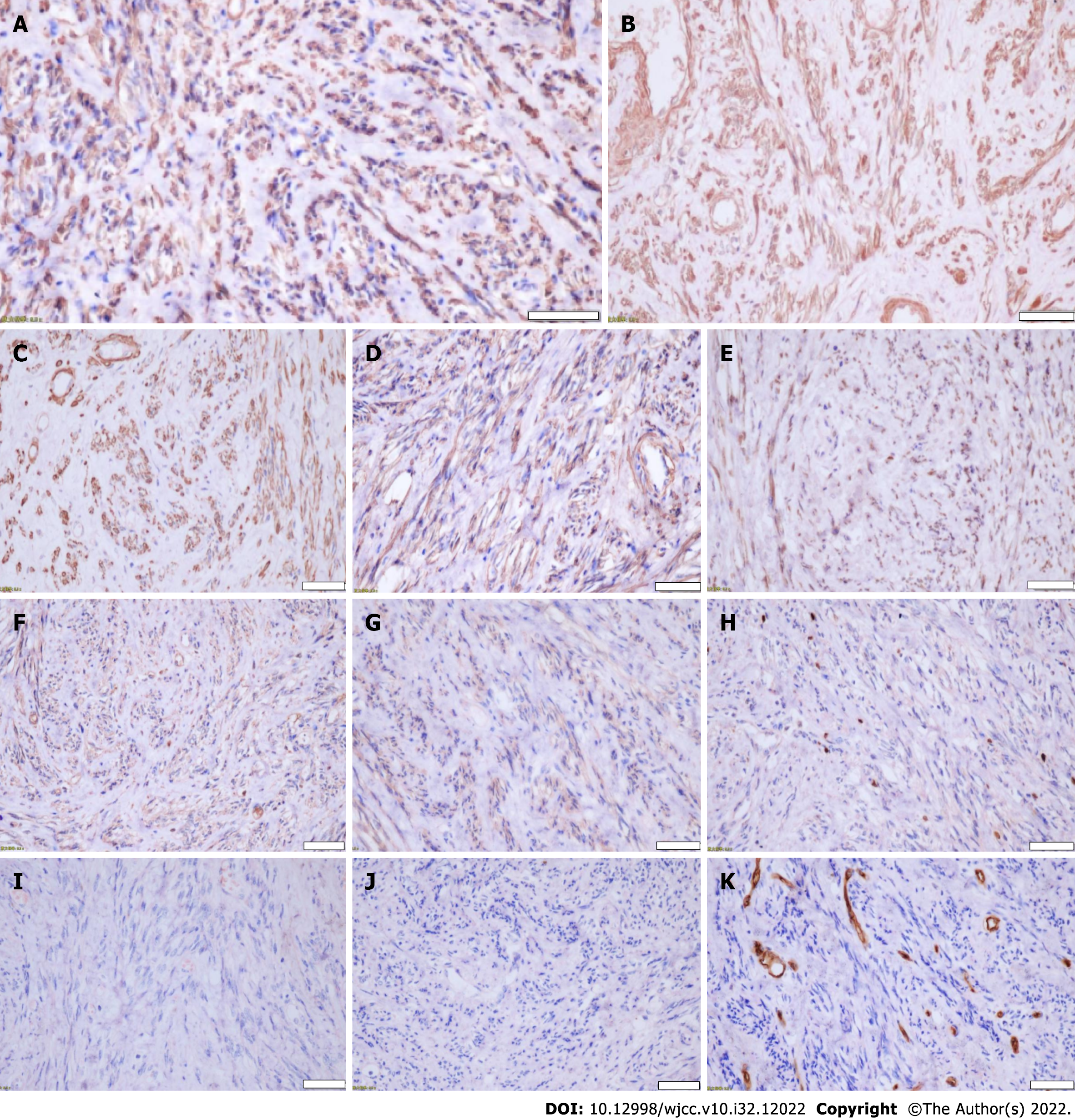
Low Midline laparotomy was performed, and uterine size and morphology, bilateral fallopian tubes and ovarian size and morphology were all normal. In the right broad ligament a 15 cm × 10 cm × 10 cm well defined mass was observed, and no adhesions, the tumor was resected (Figure 1A). Pathological results were as follows: Spindle cell tumor (Figure 1B), each cell had the same morphology, bundle arrangement, mild cell morphology, no nucleus division, no bleeding and necrosis. Immunohistochemistry results were: Desmin (+) (Figure 2A), Calponin (+) (Figure 2B), Caldesmon (+) (Figure 2C), SMA (+) (Figure 2D), ER (+) (Figure 2E), CD117 (partially weak +) (Figure 2F), DOG1 (partially weak +) (Figure 2G), K1-67 (+ 1%) (Figure 2H), GFAP (-) (Figure 2I), S100 (-) (Figure 2J), and CD34 (-) (Figure 2K).
Retroperitoneal leiomyoma was diagnosed based on the pathological and immunohistochemical findings.
With the active cooperation of the patient, surgical resection was finally performed with good recovery.
At 8 mo follow-up, there were no signs of recurrence of the tumor.
Retroperitoneal leiomyoma is a rare benign tumor, and most retroperitoneal tumors are considered malignant[5]. Retroperitoneal leiomyomas located in the broad ligament parauterine are very rare[1,5,6]. There are two main types of benign leiomyomas in deep soft tissues, namely somatic soft tissue leiomyomas and retroperitoneal leiomyomas, which are composed of closed mature leiomyocytes[7], which are more common in perimenopausal women[4]. Our patient was also perimenopausal. Retroperitoneal leiomyomas mainly need to be distinguished from leiomyosarcomas, which differ in terms of clinical, morphological, and imaging manifestations. In addition, we performed CA125 for this patient and had normal results, which may be a means of distinguishing retroperitoneal leiomyomas from uterine fibroids. The results of immunohistochemistry helped us to classify the tumor body that were removed, and in conjunction with the results of pathological examination, identified our patient as having a retroperitoneal leiomyoma. The patient presented with pain in the right lower quadrant and underwent a color ultrasound examination, which suggested the presence of a mass near the uterus, but did not help us to determine the specific nature and source of the mass. During laparotomy exploration, we performed a rapid pathological examination, the pathological results suggested spindle cells, and subsequent immunohistochemical results supported the diagnosis of retroperitoneal leiomyoma. The preferred treatment for retroperitoneal leiomyoma is surgery, a previously reported conservative approach showed that the tumor was prone to recurrence[8].
In summary, we report a rare case of retroperitoneal leiomyoma located in the broad ligament approximately 15 cm × 10 cm × 10 cm in size in a 47-year-old female. Retroperitoneal leiomyoma located in the broad ligament is a rare and benign tumor and resection of the tumor confers good outcomes. And our case adds reference on this disease.
We would like to thank the patient and her family members for their contributions to this report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Agrawal P, United States; Dayan D, Israel S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Chmaj-Wierzchowska K, Buks J, Wierzchowski M, Szymanowski K, Opala T. Leiomyoma cellulare in the broad ligament of the uterus--case report and review of literature. Ginekol Pol. 2012;83:301-304. [PubMed] |
| 2. | Poliquin V, Victory R, Vilos GA. Epidemiology, presentation, and management of retroperitoneal leiomyomata: systematic literature review and case report. J Minim Invasive Gynecol. 2008;15:152-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Panagopoulos I, Gorunova L, Bjerkehagen B, Heim S. Novel KAT6B-KANSL1 fusion gene identified by RNA sequencing in retroperitoneal leiomyoma with t(10;17)(q22;q21). PLoS One. 2015;10:e0117010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Billings SD, Folpe AL, Weiss SW. Do leiomyomas of deep soft tissue exist? Am J Surg Pathol. 2001;25:1134-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 101] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Paal E, Miettinen M. Retroperitoneal leiomyomas: a clinicopathologic and immunohistochemical study of 56 cases with a comparison to retroperitoneal leiomyosarcomas. Am J Surg Pathol. 2001;25:1355-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Vieira SC, França JC, Fé JA, Santos LG, Almeida NM. [Benign metastasizing uterine leiomyoma: case reports]. Rev Bras Ginecol Obstet. 2009;31:411-414. [PubMed] |
| 7. | Sabrine D, Hafsa E, Omar M, Jahid A, Znati K, Zakia B, Zouaidia F. Retroperitoneal leiomyoma of gynecologic type: a case report and review of the litterature. J Surg Case Rep. 2020;2020:rjaa489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Hague WM, Abdulwahid NA, Jacobs HS, Craft I. Use of LHRH analogue to obtain reversible castration in a patient with benign metastasizing leiomyoma. Br J Obstet Gynaecol. 1986;93:455-460. [PubMed] |