Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11929
Peer-review started: June 24, 2022
First decision: August 21, 2022
Revised: September 16, 2022
Accepted: September 23, 2022
Article in press: September 23, 2022
Published online: November 16, 2022
Processing time: 137 Days and 1.3 Hours
Blue rubber bleb nevus syndrome is a rare vascular malformation syndrome with unclear etiopathogenesis and noncurative treatments. It is characterized by multiple vascular malformations of the skin, gastrointestinal tract, and other visceral organs. The most common symptoms are intermittent gastrointestinal bleeding and secondary iron deficiency anemia, thus requiring repeated blood transfusions and hospitalizations. It is easily missed and misdiagnosed, and there is no specific treatment.
We report a case of blue rubber bleb nevus syndrome combined with disseminated intravascular coagulation and efficacy of treatment with argon plasma coagulation under enteroscopy and sirolimus. A 56-year-old female patient was admitted to the hospital with 3-year history of fatigue and dizziness that had aggravated over the past 10 d with melena. The patient had a history of repeated melena and multiple venous hemangiomas from childhood. After treatment with argon plasma coagulation combined with sirolimus for nearly 8 wk, the patient’s serum hemoglobin increased to 100 g/L. At the 12-mo follow-up, the patient was well with stable hemoglobin (102 g/L) and no recurrent intestinal bleeding.
Argon plasma coagulation and sirolimus may be an efficacious and safe treatment for blue rubber bleb nevus syndrome, which currently has no recommended treatments.
Core Tip: We present a case of blue rubber bleb nevus syndrome (BRBNS) complicated with disseminated intravascular coagulation and intestinal obstruction. BRBNS is a rare disease characterized by multiple vascular malformations of the skin, gastrointestinal tract, and other visceral organs. It is easily missed and misdiagnosed, and there is no unified treatment. We treated the patient with antifibrinolytic medication, sirolimus and argon plasma coagulation under enteroscopy. We followed up the patient for 12 mo, she was well with stable hemoglobin level and the size of skin hemangioma became smaller. In a patient with obscure, recurrent intestinal bleeding a diagnosis of BRBNS should be considered.
- Citation: Zhai JH, Li SX, Jin G, Zhang YY, Zhong WL, Chai YF, Wang BM. Blue rubber bleb nevus syndrome complicated with disseminated intravascular coagulation and intestinal obstruction: A case report. World J Clin Cases 2022; 10(32): 11929-11935
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11929.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11929
Blue rubber bled nevus syndrome (BRBNS) is a rare vascular malformation syndrome with unclear etiopathogenesis and no cure. It is an autosomal dominant genetic disorder with an incidence of 1:14000[1], in which nearly 200 cases have been reported[2]. Onset of the disease typically occurs in early childhood, while the lesions increase in size and number with advancing age[3]. BRBNS can be life-threatening[4]. The symptoms of BRBNS are multiple blue rubber-like skin lesions, repeated gastrointestinal (GI) bleeding, chronic anemia without any diagnosis, repeated blood transfusions, and hospitalization. The blue- to purple-colored, compressible, soft lesions are primarily found in the skin and GI tract. However, the lesions can also be found in the central nervous system, muscle, visceral organs, etc. Some patients with BRBNS also have decreased fibrinogen, increased D-dimer, and dysfunctional coagulation.
BRBNS is easily missed and/or misdiagnosed. There are currently no guidelines outlining specific unified treatments. However, most patients with BRBNS respond well to supportive therapy. Some patients undergo surgical resection, endoscopic intervention, or laser photocoagulation. The immunosuppressant drug sirolimus may be a promising therapeutic. Herein, we report a patient with BRBNS who responded well to argon plasma coagulation and sirolimus treatment.
A 56-year-old female presenting with massive intestinal hemorrhage was admitted to hospital. The persistent and progressively worsening hemorrhage was complicated by disseminated intravascular coagulation.
The patient had a history of chronic constipation and multiple venous hemangiomas since childhood. The lesions increased in size and number with advancing age. She did not have hepatitis or liver cirrhosis.
In the prior 3 years, the patient was repeatedly admitted to hospital due to melena or fatigue and dizziness. No blood lesions were found under endoscopy or colonoscopy. After hemostatic treatment and multiple blood transfusions (14-64 units of red blood cell transfusions every year), the patient’s hemoglobin fluctuated between 39 g/L and 61 g/L.
She was again admitted to the emergency department with worsening symptoms, including 10 d of melena. The symptoms did not improve after treatment, and she was transferred urgently to our hospital.
There was no family history of venous hemangiomas or other relevant disorders.
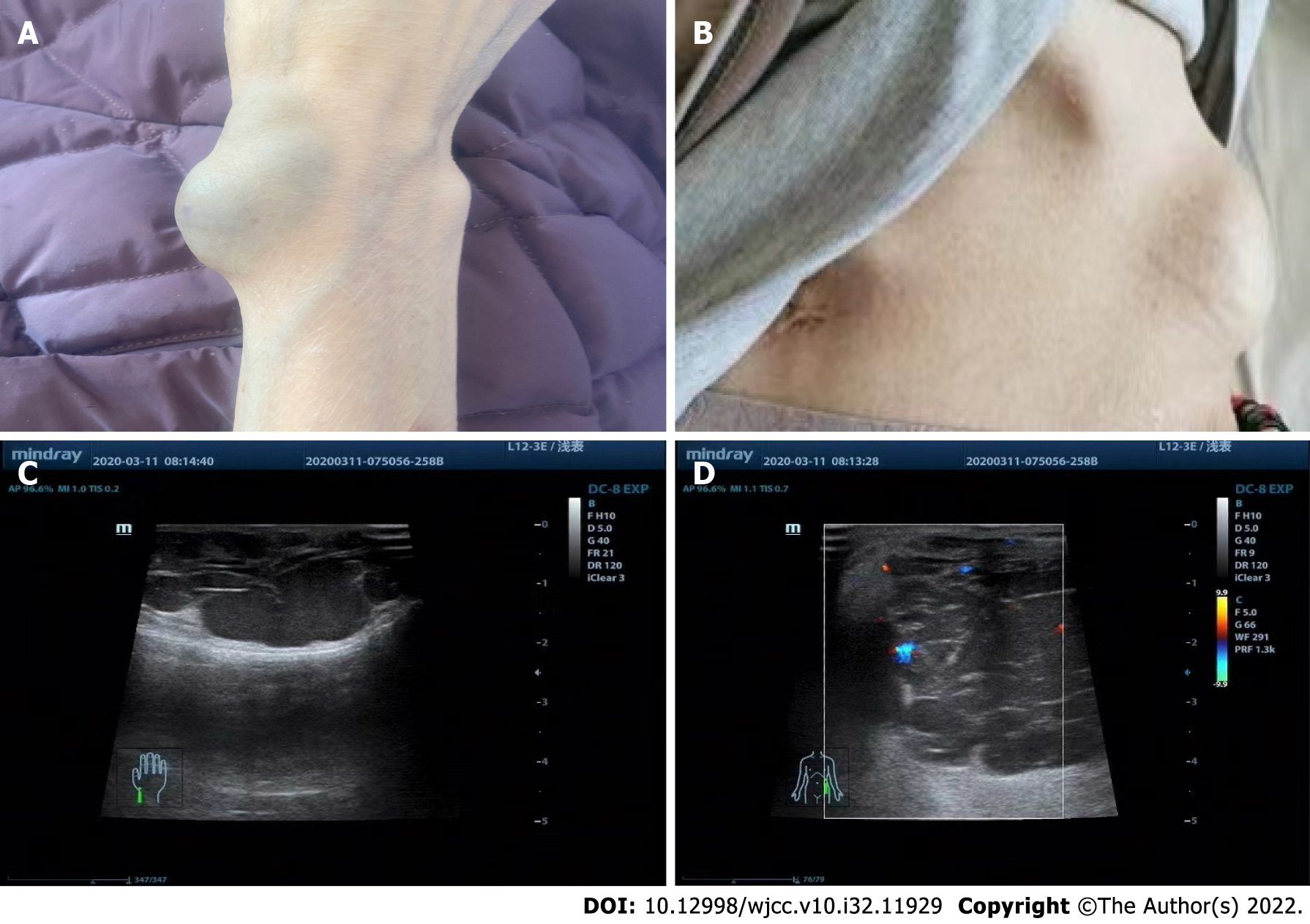
Physical examination revealed anemia and multiple blue hemangiomas protruding from the skin surface (Figure 1A and B). Skin ultrasound confirmed that the protrusions were hemangiomas (Figure 1C and D).
Laboratory examination showed white blood cell count of 1.78 × 1012/L (normal range: 3.80-5.10 × 1012/L), hemoglobin of 39 g/L (normal range: 115-150 g/L), platelets of 71 × 109/L (normal range: 125-350 × 109/L), and positivity for fecal occult blood. Additional testing revealed prothrombin time of 17.7 sec (normal range: 9.5-15.0 sec), activated partial thromboplastin time of 55.8 sec (normal range: 20.0-40.0 sec), prothrombin time-international normalized ratio of 1.65 (normal range: 0.80-1.50), fibrinogen of 0.349 g/L (normal range: 1.800-4.000 g/L), D-dimer of > 10000 ng/mL (normal range: 0-500 µg/mL), tissue plasminogen activator-inhibitor 1 complex of 14.10 ng/mL (normal range: 0.00-10.50 ng/mL), and plasmin-α2 cellulase inhibitor complex of 12.23 µg/mL (normal range: 0.00-0.80 µg/mL).
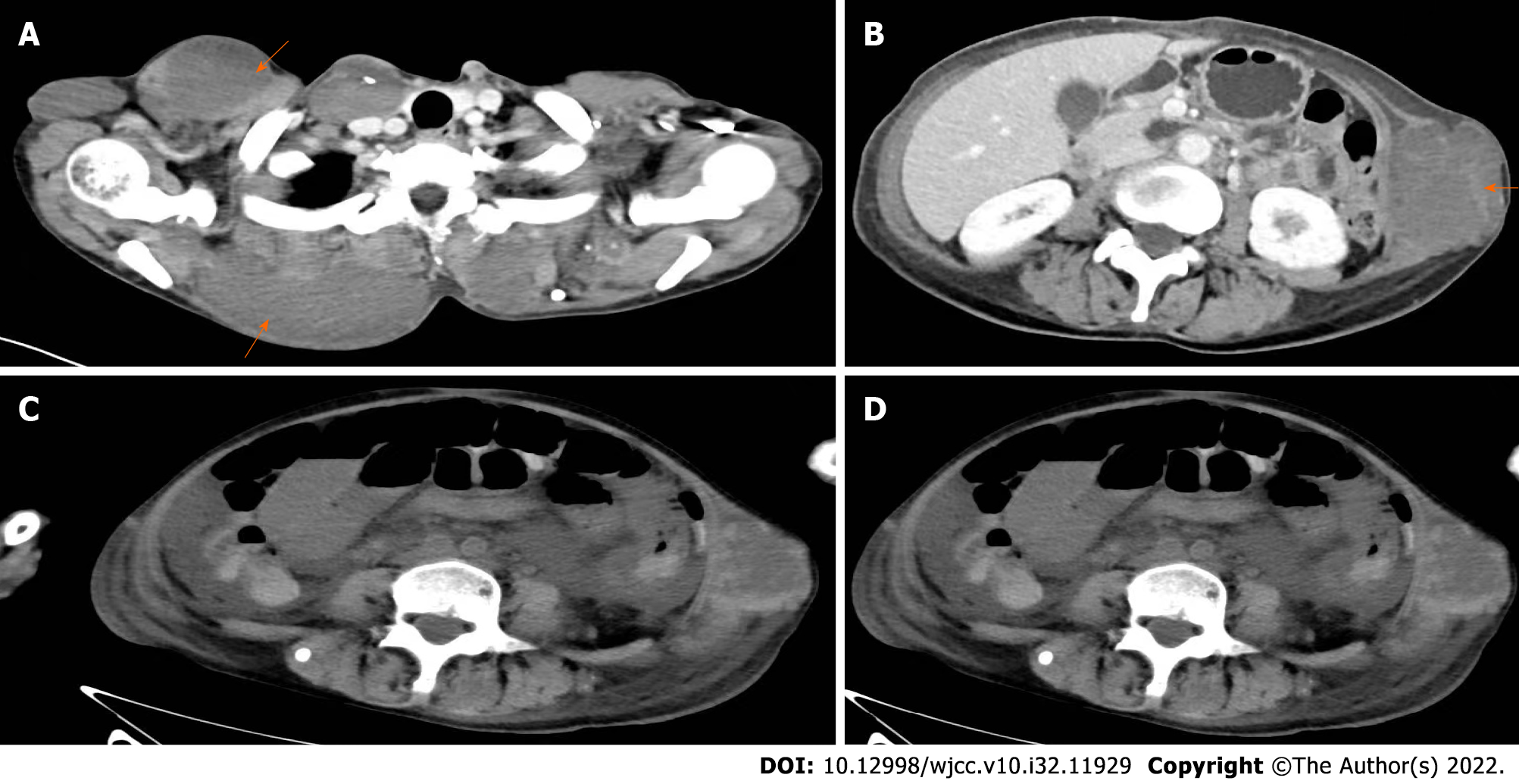
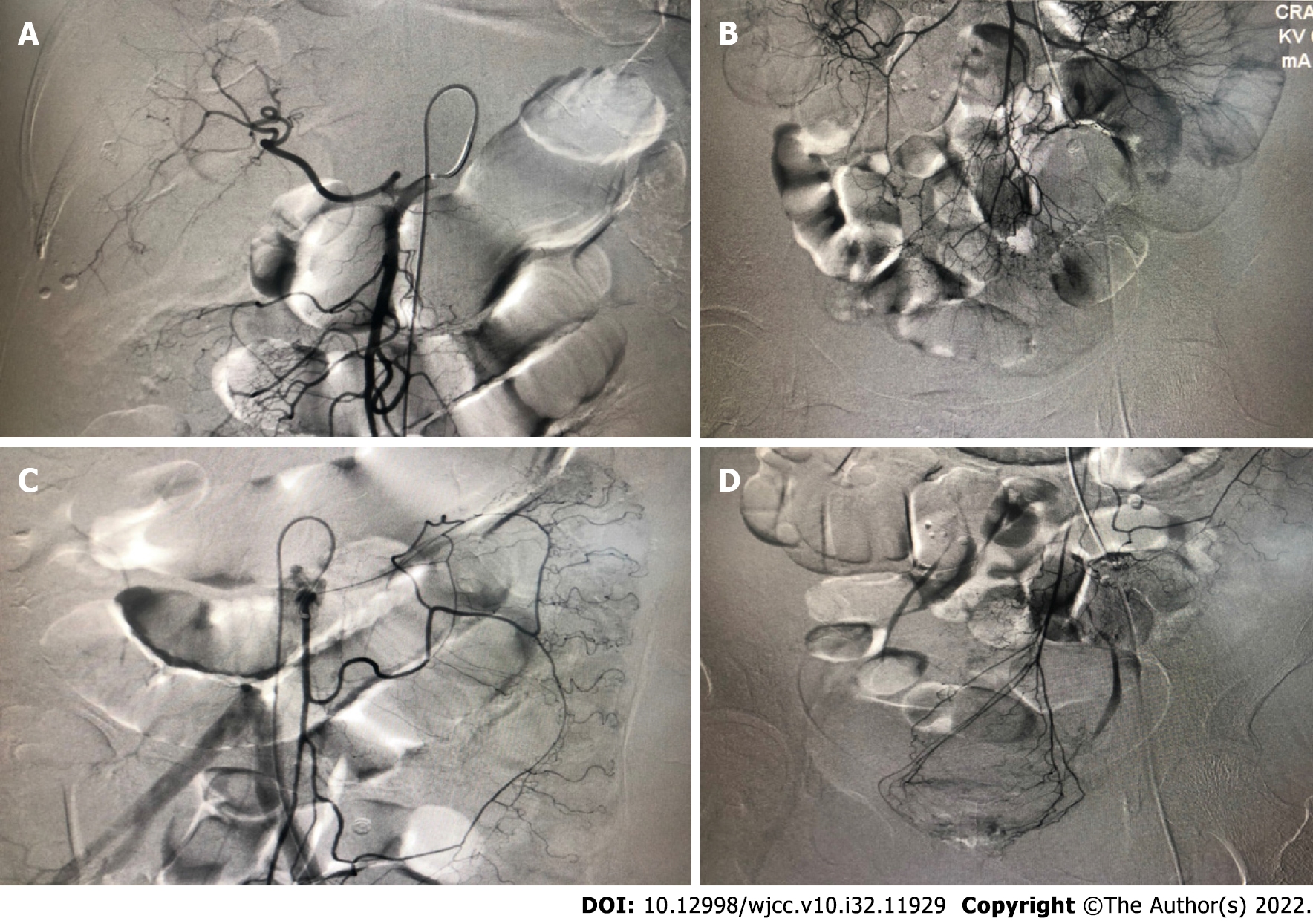
Imaging examination showed multiple hemangiomas throughout the body. Further examination showed hemorrhagic anemia with enhanced fibrinolytic type disseminated intravascular coagulation. No other bleeding causes were discovered after abdominal computed tomography examination (Figure 2A and B) or after digital subtraction angiography and mesenteric arteriography (Figure 3A-D). No definitive bleeding lesions were found by endoscopy and colonoscopy.
BRBNS with the complication of disseminated intravascular coagulation.
After admission, the patient was treated with symptomatic support including plasma, fibrinogen, vitamin K, aminosalicylic acid, tranexamic acid, octreotide, a proton pump inhibitor, thrombin, and a blood transfusion. Platelet and fibrinogen levels gradually returned to their normal ranges. The patient’s hemoglobin was stable at 60 g/L.
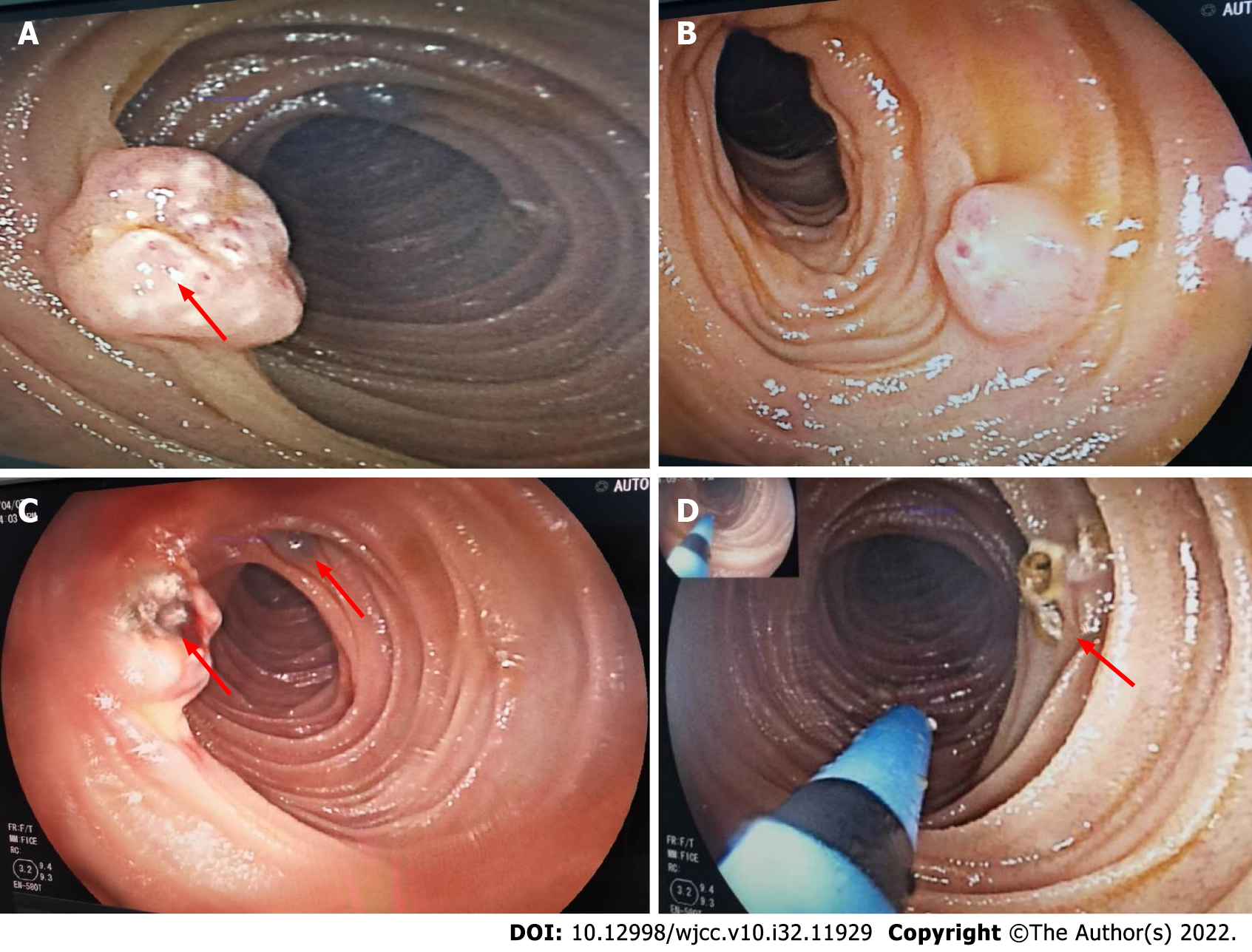
Sirolimus was also chosen for treatment. At the beginning of the sirolimus treatment, the patient still had frequent melena and the hemoglobin level decreased 40 g/L. After treatment with hemostasis and a blood transfusion, the patient’s vital signs were stable. We performed enteroscopy under general anesthesia. There were some erosions with fresh oozing blood and blue hemangiomas under enteroscopy. Argon plasma coagulation hemostasis was used to resolve the bleeding (Figure 4A-D).
After 1 mo of sirolimus administration, the melena had ceased. The concentration of sirolimus was monitored to ensure effective therapeutic concentration, in which the hemoglobin level gradually increased to 73 g/L. At this point, the stool occult blood test was negative. However, the patient had symptoms of constipation, abdominal distension, and abdominal pain. Abdominal computed tomography examination revealed intestinal obstruction (Figure 2C and D). The obstruction may have been caused by sirolimus side effects, which include constipation and intestinal hemangioma. Fasting, laxative and supportive treatment were recommended. The abdominal distension and pain improved gradually. Sirolimus treatment continued while the intestinal obstruction was resolved.
The patient’s condition improved gradually. She was discharged after 67 d when the hemoglobin levels were 73 g/L. One month after discharge, the fecal occult blood test was negative, the hemoglobin level was 72 g/L, and no further blood transfusion was performed. Six months later, the patient was well with stable hemoglobin (88 g/L) and no recurrent intestinal bleeding. At the 12-mo follow-up, the skin hemangiomas decreased in size, no recurrent intestinal bleeding was present, no intestinal obstruction was observed, and the hemoglobin level was 102 g/L.
BRBNS is a rare disease characterized by multiple vascular malformations of the skin, GI tract, and other visceral organs. The most common symptoms are intermittent GI bleeding and secondary iron deficiency anemia, requiring repeated blood transfusions and hospitalizations. GI hemorrhage usually occurs at an older age and is predominant in the small intestine and distal colon[5]. Some of the blebs have a homogenous, dark blue to purple color and appear slightly raised from the surface under endoscopy[6]. Some patients with BRBNS experience complications with decreased fibrinogen, increased D-dimer, and coagulation dysfunction[5,7].
Diagnosis of BRBNS is based on the presence of characteristic cutaneous lesions with or without GI bleeding and/or involvement of other organs. The small intestine has anatomical characteristics, such as long length, complex arrangement, and large intra-abdominal mobility. Because of this, the bleeding symptoms are often hidden. Endoscopy and colonoscopy exploration is difficult, and the rate of missed diagnoses and misdiagnoses are high[6]. The rate is also high because BRBNS is a rare cause of small bowel bleeding in the elderly[8].
No standard treatment exists for BRBNS and likely benefits from attention by a multidisciplinary team[2]. Treatments are focused on symptom relief. The choice of treatment varies depending on the intestine involved, the severity of the disease, and the site, size, and number of lesions[9]. Most patients respond to supportive therapy, such as iron supplementation and blood transfusion.
Progress in endoscopic technology has advanced medical practice. Techniques such as argon plasma coagulation, endoloops, or lauromacrogol injection (sclerotherapy) have been suggested for the treatment of vascular lesions[8]. The short-term effect of surgical resection is good. However, the intestinal lesions are typically scattered, resulting in multiple bleeding foci. Removal of all lesions is difficult to achieve and recurrence remains a likely risk. Lesions located in the small intestine and transmural lesions are relatively large and may have a higher risk of perforation; as such, they should be treated cautiously[4]. There are also reports of individual cases subjected to combined endoscopic treatment and surgery[8], but they lack long-term follow-up. A previous study indicated that surgery and endoscopic therapy can lead to recurrence[4].
It has been reported that patients may have recurrent intestinal obstruction due to intestinal hemangioma[10]. Some patients improve with symptomatic and supportive treatment, while some patients require surgical resection. Our patient developed intestinal obstruction during hospitalization, which was related to intestinal hemangioma and constipation (sirolimus side effect). The patient’s condition improved after symptomatic and supportive treatment. Surgery was not required in this case.
Sirolimus is a mammalian target of the rapamycin inhibitors, and it treats vascular abnormalities[11]. It can control angiogenesis and endothelial cell activity in lesions. It was first applied clinically in 2012[12]. Sirolimus reduces the size of venous hemangioma, thus alleviating GI bleeding and eliminating dependence on blood transfusions for patients with BRBNS[13]. The mean response time is 1.6 mo (95% confidence interval: 0.75-2.36 mo). Around 96% of patients achieve a therapeutic effect at the minimum dose (1.6 mg/m2/d, twice a day)[14].
Our patient had massive intestinal bleeding complicated with disseminated intravascular coagulation (ISTH score was 6 points). Our initial strategy was based on antifibrinolytic and hemostatic therapy (octreotide, proton pump inhibitor) along with a blood transfusion. Because the fibrinogen level of the patient significantly decreased, there was a clear contraindication to anticoagulation, and the patient had severe GI bleeding, we performed argon plasma coagulation to resolve the bleeding. The enteroscopy intervention stabilized the patient so that sirolimus treatment could begin. The patient still experienced intermittent melena after taking the sirolimus (1 mg once a day) for 1 mo. However, it was soon resolved and no further blood transfusions were required, suggesting that the intended effect of the sirolimus was achieved.
Due to case rarity and (common) symptoms overlapping with many GI diseases, BRBNS is easily missed and misdiagnosed. Therefore, it is difficult to conduct large-scale randomized controlled clinical studies, and no standard treatment exists. Endoscopic intervention, argon plasma coagulation, hemostasis, symptomatic treatment, and sirolimus were chosen to treat this patient. The patient responded well, indicating that sirolimus may be an efficacious treatment for BRBNS. However, an intestinal obstruction later occurred, likely due to side effects of sirolimus. To prevent this complication, patients with BRBNS receiving sirolimus should limit low-fiber foods and take laxatives to decrease constipation. A multidisciplinary approach should be adopted for BRBNS patients according to the severity and complexity of their disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Casella C, Italy; Totoki T, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Martinez CA, Rodrigues MR, Sato DT, Silveira Júnior PP, Gama RF, Mattavelli CB, Pereira JA. Blue rubber bleb nevus syndrome as a cause of lower digestive bleeding. Case Rep Surg. 2014;2014:683684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Baigrie D, Rice AS, An IC. Blue Rubber Bleb Nevus Syndrome. 2022 Jul 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] |
| 3. | Jin XL, Wang ZH, Xiao XB, Huang LS, Zhao XY. Blue rubber bleb nevus syndrome: a case report and literature review. World J Gastroenterol. 2014;20:17254-17259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 80] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Ur Rashid M, Muhammad Khan M, Ullah W, Hussain I, Hurairah A. Blue rubber bleb nevus: a rare cause of GI bleeding-review of management. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Chen W, Chen H, Shan G, Yang M, Hu F, Li Q, Chen L, Xu G. Blue rubber bleb nevus syndrome: our experience and new endoscopic management. Medicine (Baltimore). 2017;96:e7792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Jamali T, Choi K, Tasleem S, Mansour N. Endoscopic patterns of the blebs in blue rubber bleb nevus syndrome. Gastrointest Endosc. 2021;93:1181-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Yamada S, Arahata M, Morishita E, Asakura H. Blue Rubber Bleb Nevus Syndrome Complicated by Enhanced-Fibrinolytic-Type DIC: A Case Report. Ann Vasc Dis. 2021;14:252-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Malafaia MC, Heissat S, Jacob P, Le Gall C, Ruiz M, Saurin JC, Pioche M. Blue rubber bleb nevus syndrome: endoscopic treatment with sclerotherapy during double-balloon enteroscopy in a 9-year-old boy. Endoscopy. 2019;51:E98-E100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Li A, Chen FX, Li YQ. An Unusual Cause of Recurrent Melena. Gastroenterology. 2019;157:311-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Chen SM, Tsao TF, Lee HL. A Rare Cause of Chronic Anemia and Recurrent Bowel Obstruction. Gastroenterology. 2018;154:e4-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | AlNooh BM, AlQadri NG, Alghubayn M, AlAjlan SM. Sirolimus in the Management of Blue Rubber Bleb Nevus Syndrome: A Case Report and Review of the Literature. Case Rep Dermatol. 2021;13:417-421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Yuksekkaya H, Ozbek O, Keser M, Toy H. Blue rubber bleb nevus syndrome: successful treatment with sirolimus. Pediatrics. 2012;129:e1080-e1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Zhou J, Zhao Z, Sun T, Liu W, Yu Z, Liu J, Yu Y, Ning S, Zhang H. Efficacy and Safety of Sirolimus for Blue Rubber Bleb Nevus Syndrome: A Prospective Study. Am J Gastroenterol. 2021;116:1044-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Wong XL, Phan K, Rodríguez Bandera AI, Sebaratnam DF. Sirolimus in blue rubber bleb naevus syndrome: A systematic review. J Paediatr Child Health. 2019;55:152-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |