Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11908
Peer-review started: July 26, 2022
First decision: September 5, 2022
Revised: September 19, 2022
Accepted: October 19, 2022
Article in press: October 19, 2022
Published online: November 16, 2022
Processing time: 105 Days and 3.4 Hours
Multiple rice bodies in the wrist is a rare disorder that requires surgery, and there are still many uncertainties regarding its diagnosis and treatment.
We described a rare case of chronic idiopathic tenosynovitis with rice bodies of the wrist in a 71-year-old man and reviewed similar topics in the literature. A total of 43 articles and 61 cases were included in the literature review. Our case had a usual presentation: it was similar to those in the literature. The affected popu
We reported a case of wrist idiopathic tenosynovitis with rice body formation, and established a clinical management algorithm for wrist tenosynovitis with rice bodies, which can provide some reference for our clinical diagnosis and tr
Core Tip: We report a rare case of wrist idiopathic tenosynovitis with rice bodies formation. The rice body formation in the wrist is a sporadic disease that requires surgical treatment. Its symptoms are insidious, nonspecific and difficult to identify. And we did the literature review, which can provide a reference for the diagnosis and treatment of the wrist rice-body bursitis.
- Citation: Tian Y, Zhou HB, Yi K, Wang KJ. Idiopathic tenosynovitis of the wrist with multiple rice bodies: A case report and review of literature. World J Clin Cases 2022; 10(32): 11908-11920
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11908.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11908
Riese[1] first described rice bodies in tuberculous arthritis in 1895 and named the condition so because it resembled polished white rice. Microscopically, the rice bodies are composed of eosinophilic nuclei and fibrin due to a non-specific reaction to chronic joint inflammation[2]. Rice body formation has no significant correlation with disease progression, severity, or prognosis[3]. It is commonly seen in tuberculous arthritis, rheumatoid arthritis, and seronegative rheumatoid arthritis, and has also been reported in hip replacement surgery[4], fungal infections[5], and systemic lupus erythematosus[6]. It mainly occurs in the joint capsule or the surrounding synovial sac of the shoulder and knee, but rarely in the wrist. Herein, we present a case of wrist tenosynovitis with rice body formation; the patient underwent surgery and had no recurrence during the twelve-month follow-up. In addition, we review the relevant literature to further appreciate the condition’s epidemiological characteristics.
A 71-year-old man complained of increased swelling of his left wrist and exercise restriction.
The patient was admitted to our orthopaedic outpatient department because of increased swelling and restricted movements of his left wrist for half a month.
The patient had no recent history of trauma, except for an injury to the back of the left hand more than ten years earlier that resulted in the flexion of the left hand's fingers in a semi-clenched fist shape. He had had a history of eczema for three years, had been treated with traditional Chinese medicine, and denied a history of tuberculosis.
The patient had no special personal and family history.
Physical examination revealed a cystic mass on the palmar side of the left wrist with unclear borders and mild tenderness. The left hand's fingers were not weak or numb, and Tinel’s sign was negative. The range of motion of left wrist flexion was 0°-45°.
Laboratory tests were normal. The erythrocyte sedimentation rate was 18 mm/L, and the C-reactive protein was 0 mg/L.
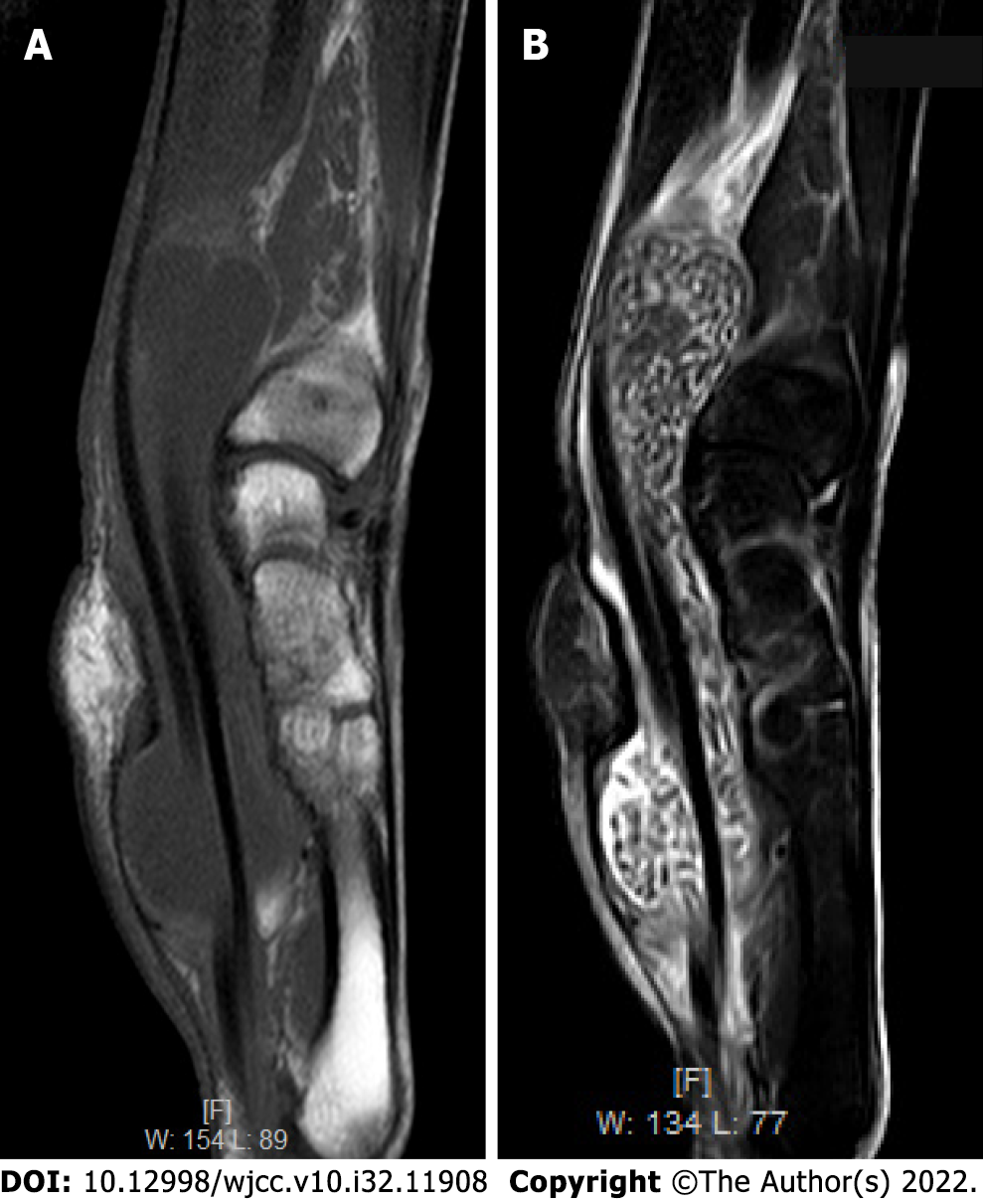
Ultrasound examination in other hospitals showed a cystic hypoechoic mass on the palmar side of the left wrist, with clear borders, an uneven internal echo, noticeable enhancement of the posterior sound, and spot-like blood flow signals around it (Figure 1). We then performed a magnetic resonance imaging (MRI) examination and found a large cystic mass in the volar flexor tendon and carpal tunnel of the left wrist. The mass was filled with rice-sized particles that showed low signals both on the T1 and T2 weighted images (Figure 2). The left carpal tunnel volume had increased, the median nerve structure was unclear, and the left transverse carpal ligament showed an arcuate bulge. Soft tissue swelling of the distal left forearm, around the wrist and the left palm, was observed, with a patch-like long T1 and high T2 weighted-signal shadow.
On histopathological examination of the resected cyst wall, chronic, nonspecific inflammation was observed. The postoperative rheumatoid factor test was normal, at 1.40 IU/mL. The final diagnosis was idiopathic tenosynovitis with multiple rice bodies. Two weeks after the operation, the wound healed, and the stitches were removed. During the twelve-month follow-up period, the symptoms resolved without recurrence.
Idiopathic tenosynovitis.
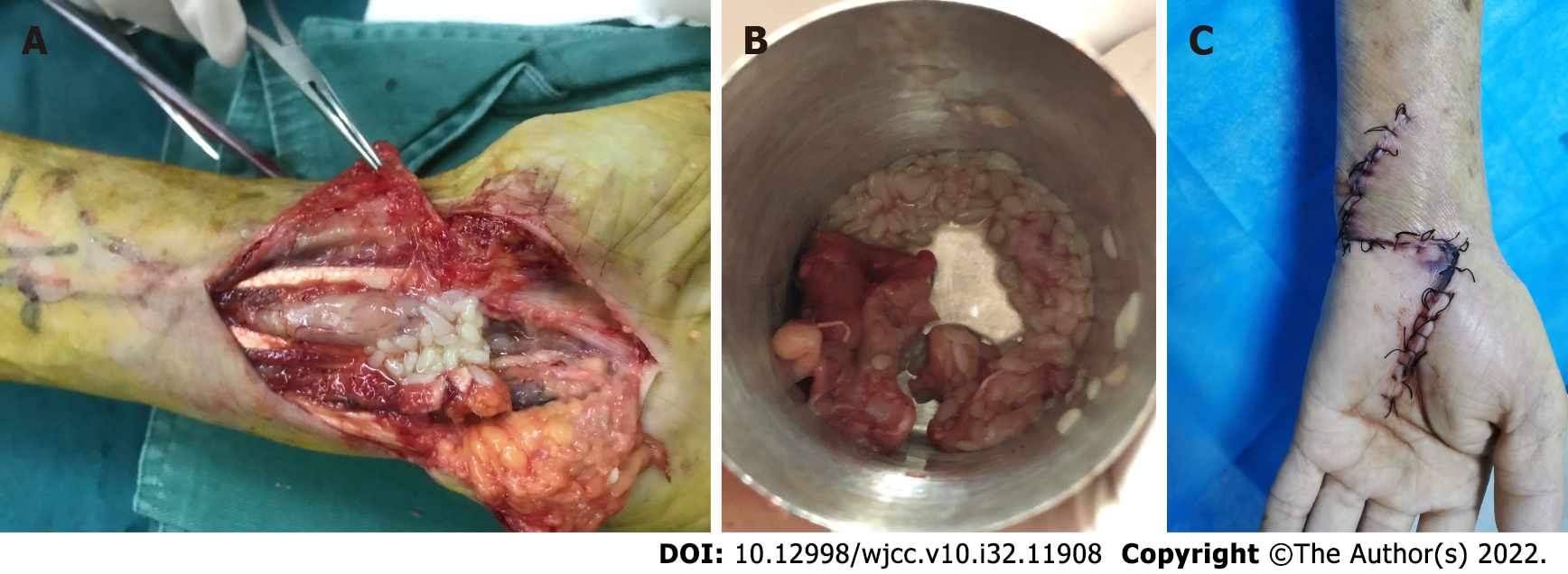
An excision biopsy was performed, with an "N" incision along the left wrist. Intraoperative incision of the carpal tunnel revealed a cystic mass originating from the tendon sheath of the flexor carpal tendon throughout the palm, carpal tunnel, and distal end of the forearm. After the cyst wall was cut open, many white rice-sized loose bodies were observed (Figure 3). All the rice bodies and the whole bursa were removed. The acid-fast bacilli smear test of the cyst fluid was negative, and the mycobacterial culture was negative too.
Two weeks after the operation, the wound healed, and the stitches were removed. During the twelve-month follow-up period, the symptoms resolved without recurrence.
Rice bodies are loose fibrous particles of various sizes and shapes in the synovial bursa around a joint. They can float freely in joint fluid or attach to the synovium and are considered non-specific reactions and final products of chronic inflammation, hyperplasia, and secondary degeneration[2]. Most rice bodies are mainly composed of fibrin and a small amount of collagen; only a tiny part is wholly composed of fibrin. Some also contain neuraminidase and lipids on the surface[2,7]. The mechanism of rice body formation is still controversial. Cheung et al[8] found that rice bodies and the synovium contained equal proportions of types I and III collagen and type AB collagen and speculated that the formation of rice grains is related to synovial microinfarction. Berg et al[7] also observed that some rice bodies contain vascular tissue, indicating that they were previously connected to the synovium. Non-vascular-type rice bodies are likely to be further degraded from vascular-type ones. However, a study on rice bodies from a patient with JIA (Juvenile rheumatoid arthritis) showed that they contain a large number of synovial B-type cells, which are located in a matrix composed of collagen fibres, fibrin, and amorphous substances, and may be responsible for the secretion of collagen and fibrin[9]. Popert et al[3] subsequently proposed that rice bodies are formed independently of the synovium, and synovial B cells may play an essential role in this process. In summary, we consider that synovial microinfarction and synovial B cells work together to lead to the formation of rice bodies. After synovial microinfarction, sloughing of the infarcted tissue into the synovial fluid forms the initial rice bodies-synovial fragments that contain inflammatory cells, synovial B cells, and vascular tissue. The final rice bodies are gradually formed by the secretion of fibrin from synovial B cells and the deposition of fibrin in the synovial fluid.
In diagnostic imageology, the principal differential diagnoses of rice bodies are synovial chondromatosis and pigmented villonodular synovitis. Ultrasonography and MRI are the most effective diagnostic imaging modalities. On ultrasonography, rice granules appear as low-to-anechoic spherical intracapsular nodules but are almost indistinguishable from synovial chondromatosis[10]. On MRI, rice bodies show low signal T1 and T2 weighted sequences. In contrast, the nodules of synovial chondromatosis show a high signal on the T2-weighted sequence because of the presence of cartilage components. Meanwhile, the signal cavity of pigmented villous nodular synovitis reflects hemosiderin deposition and the lack of sensitivity artefacts of the gradient echo sequence, which can be distinguished from rice bodies[10].
However, the biggest challenge of wrist rice-body bursitis is to find the relevant cause-rheumatoid, tuberculosis, idiopathic tenosynovitis, or other diseases-which is important for postoperative drug treatment and patient prognostication. To solve this problem, we conducted a literature search in the PubMed, MEDLINE and CNKI (China National Knowledge Infrastructure) databases and used "rice body," "rice bodies," "rice body formation," and "wrist" as search terms. A total of 43 articles and 61 cases were included; their characteristics are summarized in Tables 1 and 2. Our case was similar to those in the literature, with a usual presentation. The affected population was mainly older adults, with an average age of 59.43 (range, 3 to 90) years. The male-to-female ratio was 1.54:1 (37/24). The presentation was insidious, most of them showed limited swel
| Numbers | Percent | |
| Gender | ||
| Male | 37 | 60.7 |
| Female | 24 | 39.3 |
| Involved site | ||
| Flexor tendon sheath | 58 | 95.1 |
| Extensor tendon sheath | 3 | 4.90 |
| Pathogenesis | ||
| TB | 21 | 34.4 |
| NTM | 15 | 24.6 |
| Idiopathic tenosynovitis | 19 | 31.1 |
| Other reasons | 6 | 9.8 |
| ESR | ||
| Normal | 13 | 21.3 |
| High | 14 | 23.0 |
| ND | 34 | 55.7 |
| CRP | ||
| Normal | 21 | 34.4 |
| High | 4 | 6.60 |
| ND | 36 | 59.0 |
| CTS | ||
| Negative | 14 | 23.0 |
| Positive | 15 | 24.5 |
| ND | 32 | 52.5 |
| Surgical treatment | ||
| Yes | 60 | 98.4 |
| No | 1 | 1.6 |
| Recurrence | ||
| Yes | 10 | 16.4 |
| No | 35 | 57.4 |
| ND | 16 | 26.2 |
| Ref. | Gender/ age (yr) | Location | Symptoms/duration | Laboratory testing | Histological findings | Pathogenesis | Surgical treatment | Duration-antibiotics | Outcome |
| Suso et al[18], 1988 | M/41 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS | Elevated ESR of 51 mm/h | Tuberculous granuloma, langerhan’s cells | TB | Yes | I + R-9 mo | No recurrence during 3 yr follow-up |
| Sugano et al[19], 2000 | M/81 | Flexor tendon sheath | Swelling/24 mo | Normal | giant cell, granuloma | IT | Yes | No | ND |
| Ohtani et al[6], 2002 | F/54 | Flexor tendon sheath | Pain, swelling, restricted ROM/12 mo | ND | Chronic nonspecific inflammation | SLE | Yes | No | No recurrence during 1 yr follow-up |
| Chau et al[20], 2003 | M/50 | Flexor tendon sheath | Swelling/13 mo | ND | Granuloma, giant cell | NTM | Yes | Anti-tuberculous chemotherapy | Recurrence 5 mo later and re-operation |
| M/69 | Flexor tendon sheath | Swelling/13 mo | ND | Granuloma, giant cell | NTM | Yes | Anti-tuberculous chemotherapy | No recurrence | |
| F/71 | Flexor tendon sheath | Pain, swelling, CTS/13 mo | ND | Granuloma, giant cell | NTM | Yes | Anti-tuberculous chemotherapy | No recurrence | |
| Lee et al[21], 2004 | M/62 | Flexor tendon sheath | Swelling, restricted ROM/30 mo | ND | Granuloma | NTM | Yes | Biaxin | Recurrence 2 yr later and re-operation |
| Huang et al[22], 2005 | M/21 | Flexor tendon sheath | Swelling/24 mo | ND | Granuloma, langerhan’s cells | TB | Yes | I + R + E-9 mo | No recurrence during 9 mo follow-up |
| Tyllianakis et al[23], 2006 | F/61 | Flexor tendon sheath | Pain, swelling, restricted ROM/6 mo | Elevated ESR of 40 mm/h | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 1 yr follow-up |
| Ergun et al[24], 2008 | M/32 | Flexor tendon sheath | Swelling/4 mo | Elevated ESR of 37 mm/h | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 2 yr follow-up |
| Teo et al[25], 2008 | F/49 | Flexor tendon sheath | Pain, swelling, restricted ROM/7 mo | Elevated ESR of 36 mm/h | Caseous necrosis | TB | Yes | No | ND |
| Nagasawa et al[26], 2009 | M/68 | Flexor tendon sheath | Pain, swelling, restricted ROM/1 mo | Normal | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 5 yr follow-up |
| Sanal et al[27], 2009 | M/22 | Flexor tendon sheath | Pain, swelling/30 mo | ND | ND | NTM | Yes | Tetracycline | ND |
| Hung et al[28], 2011 | F/56 | Flexor tendon sheath | Pain, swelling/60 mo | Normal | Granuloma | TB | Yes | Anti-tuberculous chemotherapy for 3 mo | No recurrence during 1 yr follow-up |
| Iyengar et al[29], 2011 | F/72 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/6 mo | Elevated ESR of 50 mm/h | Fibrinoid necrosis | Serum-negative RA | Yes | No | Recurrence 5 mo later and re-operation |
| Woon et al[30], 2011 | M/87 | Flexor tendon sheath | Swelling/14 mo | ND | Granuloma | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up |
| M/70 | Flexor tendon sheath | Swelling/14 months | ND | Granuloma | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up | |
| F/30 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/14 mo | ND | Tuberculous granuloma, multinucleate giant cell | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up | |
| M/44 | Flexor tendon sheath | Swelling/14 mo | ND | Epithelioid granuloma, multinucleate giant cell | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up | |
| F/24 | Flexor tendon sheath | Swelling/14 mo | ND | Epithelioid granuloma, multinucleate giant cell, central caseation | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up | |
| F/70 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/14 mo | ND | Granuloma, central caseation | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 yr follow-up | |
| Chavan et al[31], 2012 | M/57 | Flexor tendon sheath | Pain, swelling/36 mo | Elevated ESR of 45 mm/h | Granuloma, caseous necrosis | TB | Yes | Anti-tuberculous chemotherapy | ND |
| Catherine et al[32], 2012 | M/51 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/24 mo | Normal | Granuloma | IT | Yes | No | No recurrence during 1 yr follow-up |
| Chan et al[33], 2014 | M/76 | Flexor tendon sheath | Pain, swelling, restricted ROM/12 mo | Elevated ESR of 48 mm/h and CRP of 22.5 mg/L | Chronic nonspecific inflammation | NTM | Yes | CAM + R + E-2 mo | No recurrence during 1.5 yr follow-up |
| De Groote et al[34], 2014 | M/69 | Flexor tendon sheath | Pain, swelling, restricted ROM | ND | ND | RA | Yes | No | ND |
| Hong et al[35], 2015 | M/80 | Flexor tendon sheath | Swelling/36 mo | Normal | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 1 yr follow-up |
| Weber et al[36], 2015 | M/66 | Flexor tendon sheath | Pain, swelling, restricted ROM/6 mo | Elevated CRP of 16 mg/L | Granuloma, giant cell | TB | Yes | I + R-7 mo, P + E-1 mo | No recurrence during 7 mo follow-up |
| Bayram et al[37], 2016 | M/50 | Flexor tendon sheath | Pain, swelling, restricted ROM/24 mo | Elevated ESR of 24 mm/h and CRP of 18 mg/L | Granuloma | TB | Yes | Anti-tuberculous chemotherapy for 12 mo | Recurrence 6 mo later and re-operation |
| Sbai et al[38], 2016 | M/45 | Extensor tendon sheath | Pain, swelling/6 mo | Elevated ESR of 50 mm/h | Giant cell, granuloma, caseous necrosis | TB | Yes | E + P-2 mo, I + R-8 mo | No recurrence during 2 yr follow-up |
| Sulaiman et al[39], 2016 | F/71 | Extensor tendon sheath | Swelling, restricted ROM/36 mo | ND | ND | NTM | Yes | Anti-tuberculous chemotherapy and azithromycin for 9 mo | No recurrence during 9 mo follow-up |
| Namkoong et al[40], 2016 | M/76 | Flexor tendon sheath | Tendernerss, swelling/2 mo | ND | Granuloma | NTM | Yes | Anti-tuberculous chemotherapy | Recurrence 12 mo later and re-operation |
| Nabet et al[41], 2017 | M/3 | Flexor tendon sheath | pain, swelling, restricted ROM/2 mo | Normal | Chronic nonspecific inflammation | JIA | Yes | NSAID-14 mo | No recurrence during 2.5 yr follow-up |
| Yamamoto et al[42], 2017 | M/70 | Flexor tendon sheath | ND | ND | ND | IT | Yes | No | ND |
| M/70 | Flexor tendon sheath | ND | ND | Granuloma | NTM | Yes | Anti-tuberculous chemotherapy | Recurrence and re-operation of 2 times during 37 mo follow-up | |
| M/53 | Flexor tendon sheath | ND | ND | Granuloma | TB | Yes | Anti-tuberculous chemotherapy | Recurrence 14 mo later and re-operation | |
| M/63 | Flexor tendon sheath | ND | ND | Granuloma | TB | Yes | Anti-tuberculous chemotherapy for 12 mo | ND during 1 yr follow-up | |
| F/83 | Flexor tendon sheath | ND | ND | Fibrin deposition | Candida | Yes | Anti-tuberculous chemotherapy and CAM | Recurrence 4 mo later and re-operation | |
| F/73 | Flexor tendon sheath | ND | ND | Granuloma | NTM | Yes | F-8 mo | No recurrence during 8 mo follow-up | |
| M/90 | Flexor tendon sheath | ND | ND | Granuloma | NTM | Yes | F + CAM + E | No recurrence during 6 mo follow-up | |
| F/77 | Flexor tendon sheath | ND | ND | Granuloma | NTM | Yes | F + CAM + E | No recurrence during 1 yr follow-up | |
| F/80 | Flexor tendon sheath | ND | ND | Granuloma | IT | Yes | F + CAM + E | No recurrence during 6 mo follow-up | |
| Baidoo et al[43], 2018 | F/65 | Flexor tendon sheath | pain, swelling, restricted ROM, CTS/24 mo | Elevated ESR of 94 mm/h | Granuloma, langerhan’s cells | TB | Yes | E + P-3 mo, I + R-9 mo | No recurrence during 1 yr follow-up |
| Celikyay et al[44], 2018 | M/34 | Flexor tendon sheath | ND | ND | Granuloma, caseous necrosis | TB | Yes | No | ND |
| Gupta et al[11], 2018 | F/50 | Flexor tendon sheath | Pain, swelling, restricted ROM/9 mo | Elevated ESR of 50 mm/h | ND | TB | No | Anti-tuberculous chemotherapy for 6 mo | No recurrence during 6 mo follow-up |
| Hashimoto et al[45], 2018 | M/79 | Flexor tendon sheath | Swelling/3 mo | ND | Caseous necrosis, langerhan’s cells | TB | Yes | Anti-tuberculous chemotherapy for 2 mo | No recurrence during 1 yr follow-up |
| Mohammed Reda et al[46], 2018 | M/69 | Flexor tendon sheath | Pain, swelling, CTS/24 mo | Normal | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 1 yr follow-up |
| Saraya et al[47], 2018 | F/74 | Flexor tendon sheath | Swelling, restricted ROM/48 mo | Elevated ESR of 35 mm/h | Granuloma | NTM | Yes | R + E + CAM-6 mo | Recurrence 5 yr later and Remedication for 1.5 yr |
| Kurra et al[48], 2019 | F/44 | Extensor tendon sheath | Pain, swelling/12 mo | ND | Chronic nonspecific inflammation | Candida | Yes | No | ND |
| Matcuk et al[49], 2020 | F/80 | Flexor tendon sheath | Pain, swelling, restricted ROM/6 mo | Elevated ESR of 65 mm/h | Chronic nonspecific inflammation | NTM | Yes | Azithromycin+ E + moxifloxacin + linezolid | Recurrence 3 mo later and re-operation |
| Perţea et al[50], 2020 | F/65 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/2 mo | Normal | Epithelioid granuloma, langerhan’s cells | IT | Yes | No | No recurrence during 30.4 mo follow-up |
| F/70 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/4 mo | Normal | Epithelioid granuloma, langerhan’s cells | IT | Yes | No | No recurrence during 30.4 mo follow-up | |
| M/56 | Flexor tendon sheath | Swelling/24 mo | Normal | Epithelioid granuloma, langerhan’s cells | IT | Yes | No | No recurrence during 30.4 mo follow-up | |
| M/47 | Flexor tendon sheath | Swelling/48 mo | Normal | Epithelioid granuloma, langerhan’s cells | IT | Yes | No | No recurrence during 30.4 mo follow-up | |
| Daoussis et al[51], 2021 | F/63 | Flexor tendon sheath | ND | ND | ND | NTM | Yes | Anti-tuberculous chemotherapy | ND |
| Tomala et al[52], 2021 | F/86 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/24 mo | ND | Chronic nonspecific inflammation | IT | Yes | No | ND |
| Zeng et al[53], 2018 | M/67 | Flexor tendon sheath | Pain, swelling, restricted ROM/24 mo | Elevated CRP of 32.8 mg/L | Chronic nonspecific inflammation | IT | Yes | No | No recurrence |
| Li and Zhang et al[54], 2019 | M/55 | Flexor tendon sheath | Pain, swelling, restricted ROM/36 mo | ND | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 3 mo follow-up |
| Cheng et al[55], 2020 | M/41 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/0.5 mo | Elevated ESR of 17 mm/h | ND | IT | Yes | No | ND |
| Liang et al[56], 2020 | F/45 | Flexor tendon sheath | Pain, swelling, restricted ROM, CTS/24 mo | Normal | Chronic nonspecific inflammation | IT | Yes | No | No recurrence during 1 yr follow-up |
| Liu et al[57], 2021 | M/56 | Flexor tendon sheath | Pain, swelling, CTS/24 mo | ND | Prominent acidophilic, amorphous necrotic areas | IT | Yes | No | ND |
| Korkmaz et al[58], 2021 | M/42 | Flexor tendon sheath | Pain, swelling/24 mo | Normal | Granulomatous lesions with central necrosis | TB | Yes | Anti-tuberculous chemotherapy | No recurrence during 4 mo follow-up |
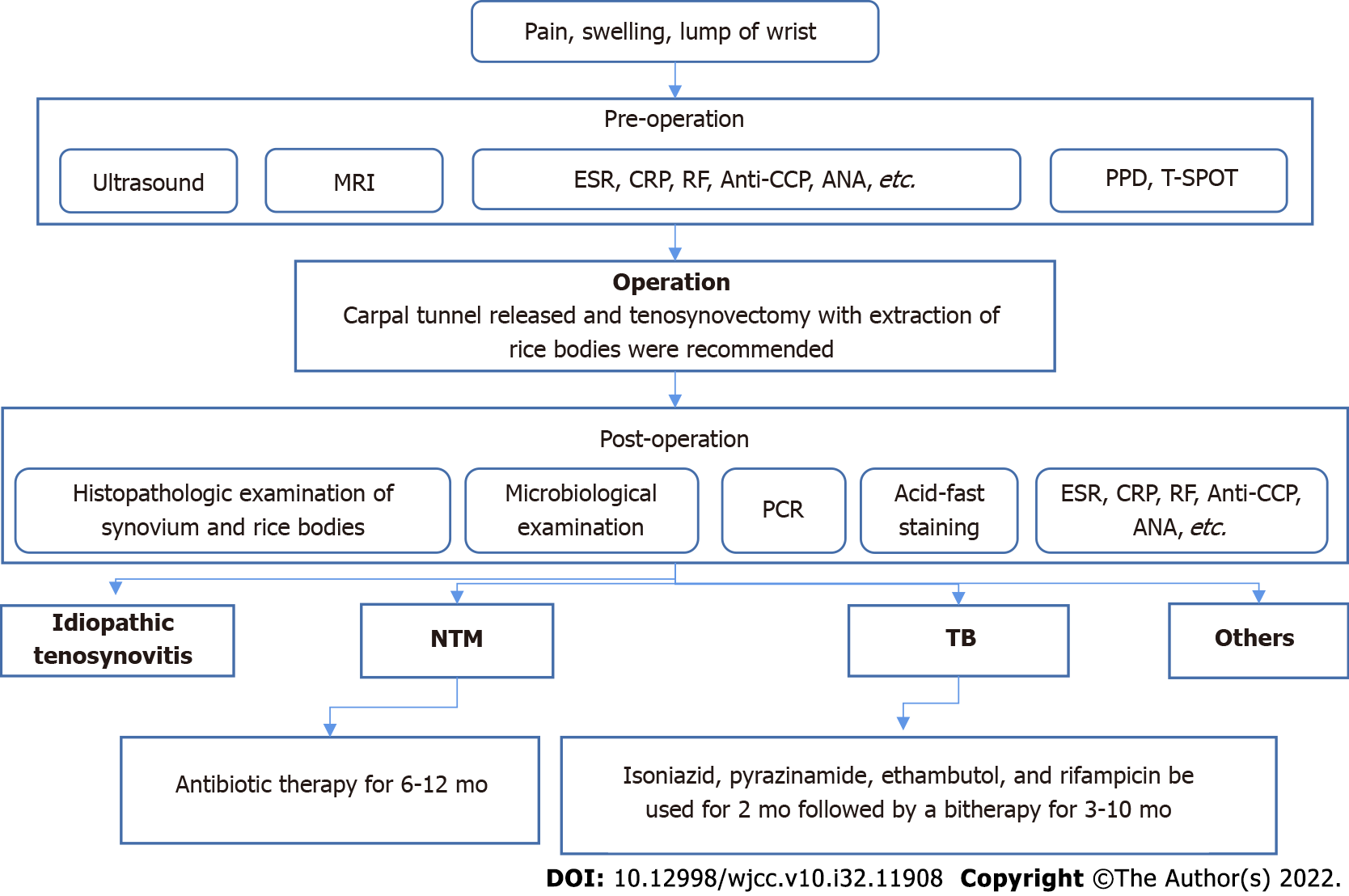
Finally, we summarized a clinical management algorithm for wrist tenosynovitis with rice bodies (Figure 4). Carpal tunnel release and tenosynovectomy with the extraction of rice bodies were recommended. Before surgery, ultrasonography and MRI examination are necessary; they are the most important standard for diagnosis. In addition, we need to take note of the laboratory tests, especially erythrocyte sedimentation rate, C-reactive protein, and the biomarkers of rheumatoid arthritis-antinuclear antibody, anti-cyclic citrullinated peptide, and rheumatoid factor. Purified protein derivative and T-SPOT tests are important for screening for tuberculosis. If necessary, we also need to perform chest X-ray or lung computed tomography imaging examinations. We should perform further pathological examination of the synovium and the rice bodies, bacterial culture, polymerase chain reaction, and acid-fast staining postoperatively. Patients with mycobacterial infections must strictly be on standardized, long-term, combined drug treatment to avoid recurrence. Because there are few such cases and related studies, this management algorithm can only provide a certain reference and needs to be further improved.
We reported a case of wrist idiopathic tenosynovitis with rice body formation and established a clinical management algorithm for wrist tenosynovitis with rice bodies, which provides a reference for clinical diagnosis and treatment. Rice body formation in the wrist is a sporadic disease that requires surgical management. Its symptoms are insidious, nonspecific, and difficult to identify. Idiopathic tenosynovitis and mycobacterial (tuberculosis or non-tuberculous) infections are the main causes, so, before a diagnosis of idiopathic tenosynovitis is made, we must exclude other causes, especially mycobacterial infections. We should especially take notice of non-tuberculous mycobacterial infections because they are difficult to treat and have poor prognoses and high recurrence rates. Therefore, anti-nontuberculous mycobacterial drug treatment is also a key issue that needs to be resolved.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jeevannavar SS, India; Pace V, Italy S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Riese H. Die Reiskorperchen in tuberculkoserkrankten Synovalsacken. Deut Zeit Chir. 1895;42:1-99. |
| 2. | Albrecht M, Marinetti GV, Jacox RF, Vaughan JH. A biochemical and electron microscopy study of rice bodies from rheumatoid patients. Arthritis Rheum. 1965;8:1053-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Popert AJ, Scott DL, Wainwright AC, Walton KW, Williamson N, Chapman JH. Frequency of occurrence, mode of development, and significance or rice bodies in rheumatoid joints. Ann Rheum Dis. 1982;41:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 98] [Reference Citation Analysis (0)] |
| 4. | Issack PS. Formation of a large rice body-containing cyst following total hip arthroplasty. BMC Res Notes. 2012;5:294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Jeong YM, Cho HY, Lee SW, Hwang YM, Kim YK. Candida septic arthritis with rice body formation: a case report and review of literature. Korean J Radiol. 2013;14:465-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Ohtani K, Fukuda K, Hamanishi C. A case of systemic lupus erythematosus associated with trigger wrist. Mod Rheumatol. 2002;12:69-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Berg E, Wainwright R, Barton B, Puchtler H, McDonald T. On the nature of rheumatoid rice bodies: an immunologic, histochemical, and electron microscope study. Arthritis Rheum. 1977;20:1343-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Cheung HS, Ryan LM, Kozin F, McCarty DJ. Synovial origins of Rice bodies in joint fluid. Arthritis Rheum. 1980;23:72-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Wynne-Roberts CR, Cassidy JT. Juvenile rheumatoid arthritis with rice bodies: light and electron microscopic studies. Ann Rheum Dis. 1979;38:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Joshi PS. Severe Sub-Acromial Bursitis with Rice Bodies in a Patient with Rheumatoid Arthritis: A Case Report and Review of Literature. Malays Orthop J. 2018;12:52-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Gupta L, Gupta V, Kumar T. Rice Bodies in Tuberculous Tenosynovitis of Wrist. Reumatol Clin (Engl Ed). 2018;14:314-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | McCarthy DJ, Cheung HS. Origin and significance of rice bodies in synovial fluid. Lancet. 1982;2:715-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Popert J. Rice-bodies, synovial debris, and joint lavage. Br J Rheumatol. 1985;24:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee, Treatment of Tuberculosis: Guidelines. Geneva: World Health Organization Copyright, 2010. |
| 15. | Bachoura A, Zelouf DS. Mycobacterial Infections in the Hand and Wrist. Hand Clin. 2020;36:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Cheung JP, Fung BK, Ip WY. Mycobacterium marinum infection of the deep structures of the hand and wrist: 25 years of experience. Hand Surg. 2010;15:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Balagué N, Uçkay I, Vostrel P, Hinrikson H, Van Aaken I, Beaulieu JY. Non-tuberculous mycobacterial infections of the hand. Chir Main. 2015;34:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Suso S, Peidro L, Ramon R. Tuberculous synovitis with "rice bodies" presenting as carpal tunnel syndrome. J Hand Surg Am. 1988;13:574-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Sugano I, Nagao T, Tajima Y, Ishida Y, Nagao K, Ohno T, Ooishi S. Variation among giant rice bodies: report of four cases and their clinicopathological features. Skeletal Radiol. 2000;29:525-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Chau CL, Griffith JF, Chan PT, Lui TH, Yu KS, Ngai WK. Rice-body formation in atypical mycobacterial tenosynovitis and bursitis: findings on sonography and MR imaging. AJR Am J Roentgenol. 2003;180:1455-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Lee EY, Rubin DA, Brown DM. Recurrent Mycobacterium marinum tenosynovitis of the wrist mimicking extraarticular synovial chondromatosis on MR images. Skeletal Radiol. 2004;33:405-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Huang GS, Lee CH, Chen CY. Clinical images: Tuberculous rice bodies of the wrist. Arthritis Rheum. 2005;52:1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Tyllianakis M, Kasimatis G, Athanaselis S, Melachrinou M. Rice-body formation and tenosynovitis of the wrist: a case report. J Orthop Surg (Hong Kong). 2006;14:208-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Ergun T, Lakadamyali H, Aydin O. Multiple rice body formation accompanying the chronic nonspecific tenosynovitis of flexor tendons of the wrist. Radiat Med. 2008;26:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Teo SC, George J, Kamarul T. Tubercular synovitis mimicking rheumatoid nodules. Med J Malaysia. 2008;63:159-161. [PubMed] |
| 26. | Nagasawa H, Okada K, Senma S, Chida S, Shimada Y. Tenosynovitis with rice body formation in a non-tuberculosis patient: a case report. Ups J Med Sci. 2009;114:184-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Sanal HT, Zor F, Kocaoğlu M, Bulakbaşi N. Atypical mycobacterial tenosynovitis and bursitis of the wrist. Diagn Interv Radiol. 2009;15:266-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Hung MH, Ho KC, Huang KF. Tuberculous tenosynovitis with rice body formation. ANZ J Surg. 2011;81:572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Iyengar K, Manickavasagar T, Nadkarni J, Mansour P, Loh W. Bilateral recurrent wrist flexor tenosynovitis and rice body formation in a patient with sero-negative rheumatoid arthritis: A case report and review of literature. Int J Surg Case Rep. 2011;2:208-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Woon CY, Phoon ES, Lee JY, Puhaindran ME, Peng YP, Teoh LC. Rice bodies, millet seeds, and melon seeds in tuberculous tenosynovitis of the hand and wrist. Ann Plast Surg. 2011;66:610-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Chavan S, Sable SS, Tekade S, Punia P. Tuberculous tenosynovitis presenting as ganglion of wrist. Case Rep Surg. 2012;2012:143921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Forse CL, Mucha BL, Santos ML, Ongcapin EH. Rice body formation without rheumatic disease or tuberculosis infection: a case report and literature review. Clin Rheumatol. 2012;31:1753-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Chan HT, Tseng CC, Chen PY, Chao CM, Lai CC. Rice body--Mycobacterium intracellulare tenosynovitis. QJM. 2014;107:395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | De Groote J, Ovreeide P, Mermuys K, Casselman J. Flexor tendon tenosynovitis with rice body formation in rheumatoid arthritis. JBR-BTR. 2014;97:123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 35. | Hong SE, Pak JH, Suh HS, Kang SR, Park BY. Rice Body Tenosynovitis without Tuberculosis Infection after Multiple Acupuncture Procedures in a Hand. Arch Plast Surg. 2015;42:502-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 36. | Weber E, Gagneux-Brunon A, Jacomo V, Rousselon T, Lucht F, Botelho-Nevers E. Tenosynovitis: a rare presentation of tuberculosis better known by hand surgeons than infectious diseases specialists. Infection. 2015;43:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 37. | Bayram S, Erşen A, Altan M, Durmaz H. Tuberculosis tenosynovitis with multiple rice bodies of the flexor tendons in the wrist: A case report. Int J Surg Case Rep. 2016;27:129-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Sbai MA, Benzarti S, Msek H, Boussen M, Khorbi A. Pseudotumoral form of soft-tissue tuberculosis of the wrist. Int J Mycobacteriol. 2016;5:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Sulaiman H, Atiya N, Loi KW, Ng KP. Rice bodies in the wrist joint. Eur J Intern Med. 2016;35:e7-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 40. | Namkoong H, Fukumoto K, Hongo I, Hasegawa N. Refractory tenosynovitis with 'rice bodies' in the hand due to Mycobacterium intracellulare. Infection. 2016;44:393-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Nabet A, Faruqui S, Hogan CJ. Rice Bodies and a Partial Flexor Tendon Rupture in a Patient with Juvenile Idiopathic Arthritis: A Case Report and Review of the Literature. JBJS Case Connect. 2017;7:e41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Yamamoto D, Tada K, Suganuma S, Ikeda K, Tsuchiya H. Non-tuberculous Mycobacterium or Fungus Induced Chronic Tenosynovitis with Rice Body of the Hand. J Hand Surg Asian Pac Vol. 2017;22:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Baidoo PK, Baddoo D, Ocloo A, Agbley D, Lartey S, Baddoo NA. Tuberculous tenosynovitis of the flexor tendons of the wrist: a case report. BMC Res Notes. 2018;11:238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Celikyay F, Yuksekkaya RZ, Bostan B. Flexor tenosynovitis of the wrist including rice bodies. Joint Bone Spine. 2018;85:373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Hashimoto K, Nishimura S, Oka N, Kakinoki R, Akagi M. Tuberculoma with phlegmon-like symptoms mimicking soft tissue sarcoma in the wrist: A case report. Mol Clin Oncol. 2018;9:207-210. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 46. | Mohammed Reda F, Talal G, Moncef B, Reda-Allah B, Moulay Omar L, Mohammed Saleh B. Mass of the thenar eminence hiding idiopathic massive rice bodies formation with a compression of the median nerve: Case report and review of the literature. Int J Surg Case Rep. 2018;50:28-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 47. | Saraya T, Fukuoka K, Maruno H, Komagata Y, Fujiwara M, Kaname S, Arimura Y, Yamada A, Takizawa H. Tenosynovitis with Rice Body Formation Due to Mycobacterium Intracellulare Infection After Initiation of Infliximab Therapy. Am J Case Rep. 2018;19:656-662. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Kurra C, Caldwell M, Taylor K, Nwachukwu C, Salar M, Kaye MB, Gopinath A, Altunkaynak C, Wasserman P. Candida Parapsilosis associated rice bodies in the extensor compartment of the wrist--an emerging finding. Radiol Case Rep. 2019;14:1539-1544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Matcuk GR Jr, Patel DB, Lefebvre RE. Horseshoe abscess of the hand with rice bodies secondary to mycobacterium avium intracellulare infection. Clin Imaging. 2020;63:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Perţea M, Veliceasa B, Velenciuc N, Terinte C, Mitrea M, Ciobanu P, Alexa O, Luncă S. Idiopathic tenosynovitis with rice bodies. Rom J Morphol Embryol. 2020;61:457-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Daoussis D, Kraniotis P, Diamantakis G, Panos G, Panagiotopoulos E. Rice bodies in MRI. Joint Bone Spine. 2021;88:105079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 52. | Tomala L, Wintzer HO, Elsner J. [Rice bodies : Case report of a rare finding in chronic tenosynovitis]. Unfallchirurg. 2021;124:853-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 53. | Zeng DJ, Chi WD, Weidong, Zheng CX. A rare case of myochondrial bursitis in the left wrist. Guangdong Yixue. 2018;39:345. [DOI] [Full Text] |
| 54. | Li LJ, Zhang LM. Surgical treatment of rice body synovitis of wrist joints in one case. Linchuang Guke Zazhi. 2019;22:250. |
| 55. | Cheng XG, Li DX, Cao Y, Zeng XC. Bursitis with rice bodies formation in wrist joint: Case report. Zhongguo Jieru Yingxiang Yu Zhiliao Xue. 2020;17:512. [DOI] [Full Text] |
| 56. | Liang XS, Li JH, Wu B. A case report of chronic tenosynovitis of the wrist with rice body formation. Zhongguo Jiaoxing Waike Zazhi. 2020;28:959-960. |
| 57. | Liu J, Cheng X, Wang R, Zeng X. Rice Bodies in Cinematic Rendering. Arthritis Rheumatol. 2021;73:2077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 58. | Korkmaz MÇ, Tolu S, Şimşek S. A Rare Case of Flexor Tenosynovitis Due to Tuberculosis in Hand and Wrist: a Case Report. Acta Chir Orthop Traumatol Cech. 2021;88:237-239. [PubMed] |