Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11877
Peer-review started: June 10, 2022
First decision: June 27, 2022
Revised: July 8, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 16, 2022
Processing time: 150 Days and 23.2 Hours
Haematoma is one of the main complications associated with pacemaker implantation. Pseudoaneurysm is a rare condition that is not easy to identify and is often overlooked.
A female patient diagnosed with high-grade atrioventricular block underwent permanent pacemaker implantation. During the operation, puncturing a small branch of the right subclavian artery developed into a pseudoaneurysm and resulted in further haematoma formation. Conventional treatment of compression haemostasis and haemostatic drugs was not effective. A series of timely trans
More possible conditions should be taken into consideration as haematoma is discovered, and timely treatment might prevent severe adverse events.
Core Tip: Haematoma is one of the main complications of permanent pacemaker implantation. We report a case of patient with permanent pacemaker implantation that presented with a haematoma without the conventional presentation of a pocket haematoma. After further examination, the subclavian artery pseudoaneurysm caused by puncture was found. The haematoma was successfully relieved after transcatheter arterial embolization. This case is a rare clinical condition, and the haematoma occurring in this situation is often not easily detected in clinical practice and cannot be treated in a timely and effective manner. Clinicians are reminded that when haematoma-related manifestations occur after permanent pacemaker implantation, as more possibilities are considered, timely targeted treatment can avoid serious adverse events.
- Citation: Zheng J, Tu XM, Gao ZY. Successful transcatheter arterial embolization treatment for chest wall haematoma following permanent pacemaker implantation: A case report. World J Clin Cases 2022; 10(32): 11877-11881
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11877.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11877
Implantable permanent cardiac pacemakers are the main treatment for bradyarrhythmia[1]. Whereas pacemaker implantation is an invasive operation, strict management is required to ensure its safety and effectiveness. Previous studies have shown that pacemaker postoperative adverse events include pacemaker device-related adverse events and complications such as pocket haematoma, pocket infection, skin ulceration, and diaphragm irritation[2]. Haematoma is one of the main complications associated with pacemaker implantation, mainly refers to pocket haematoma. The WRAP-IT trial analysis concluded that the risk of haematoma from cardiac implantable electronic device was 2.2%, representing a greater than 11-fold risk of infection[3]. There are some relevant studies among Chinese people. Chen et al[4] reported the incidence of pacemaker haematoma as 7.2% by a retrospective investigation among 139 patients in Beijing Renaissance Hospital, far higher than foreign data.
We report a case of a pseudoaneurysm and haematoma following permanent pacemaker implantation due to puncturing a small branch of the right subclavian artery during the operation. This is different from the common pacemaker associated pocket haematoma. The clinical symptoms and signs are not typical and are not easily detected. A series of timely treatments in this case was performed to prevent serious complications.
A 56-year-old woman suffered tenderness and pain at the right armpit after permanent pacemaker implantation.
The patient was admitted with repeated chest tightness and dizziness for more than 20 d. Routine laboratory examination on admission showed that routine blood, electrolyte, liver and kidney function and thyroid function were normal. Brain magnetic resonance imaging showed no abnormal appearance. The 24-h dynamic electrocardiogram monitoring results indicated sinus rhythm and grade II type II to high-grade atrioventricular block with a long RR interval of 4150 ms. This patient conformed with the indications of permanent pacemaker implantation. With the exception of contraindication, she underwent permanent pacemaker implantation smoothly. Approximately 3 h after the operation, she felt tenderness and pain at the right armpit.
She had a history of hypertension for 6 years and took irbesartan 150 mg daily for a long time with good control of blood pressure.
On physical examination, it was presumed that the tenderness was not obvious swelling with undulating sensation at the pacemaker pocket site but instead a local mass at the right armpit.
Additionally, haemoglobin decreased to 89 g/L from 113 g/L by routine blood tests.
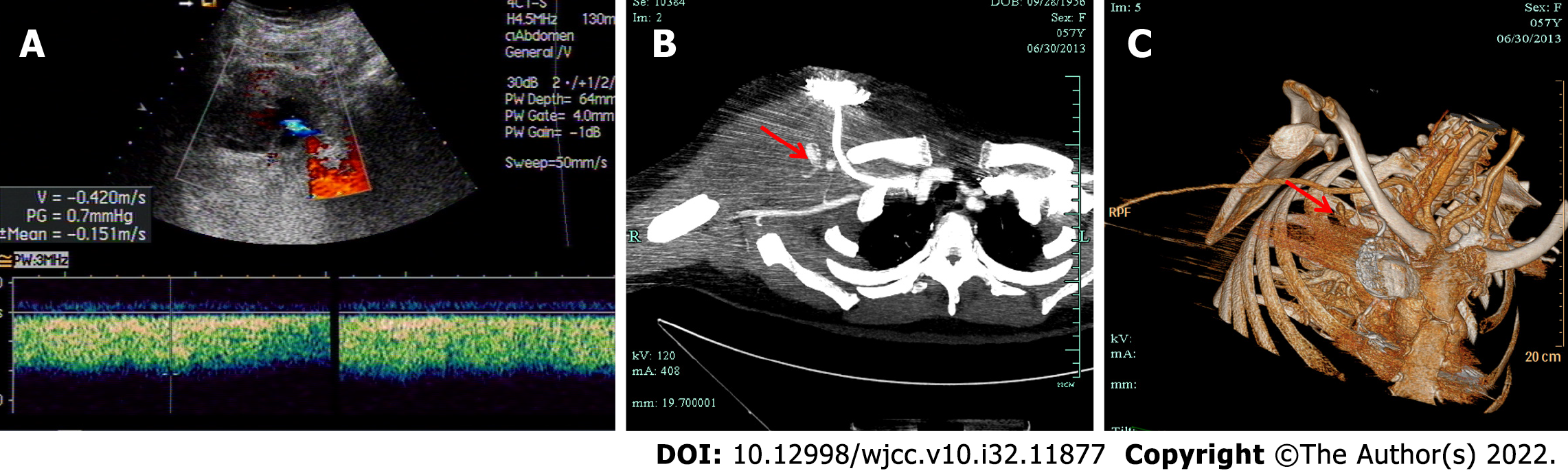
Ultrasonography showed an 11.0 cm × 5.0 cm haematoma under the right armpit, which was an unidentified source (Figure 1A). Computed tomography angiography (CTA) showed a pseudoanerysm of a small branch of the right subclavian artery, and there was no obvious abnormality of the right subclavian artery and axillary artery. A mass under the right chest wall had mixed density and was considered a haematoma (Figure 1B and C).
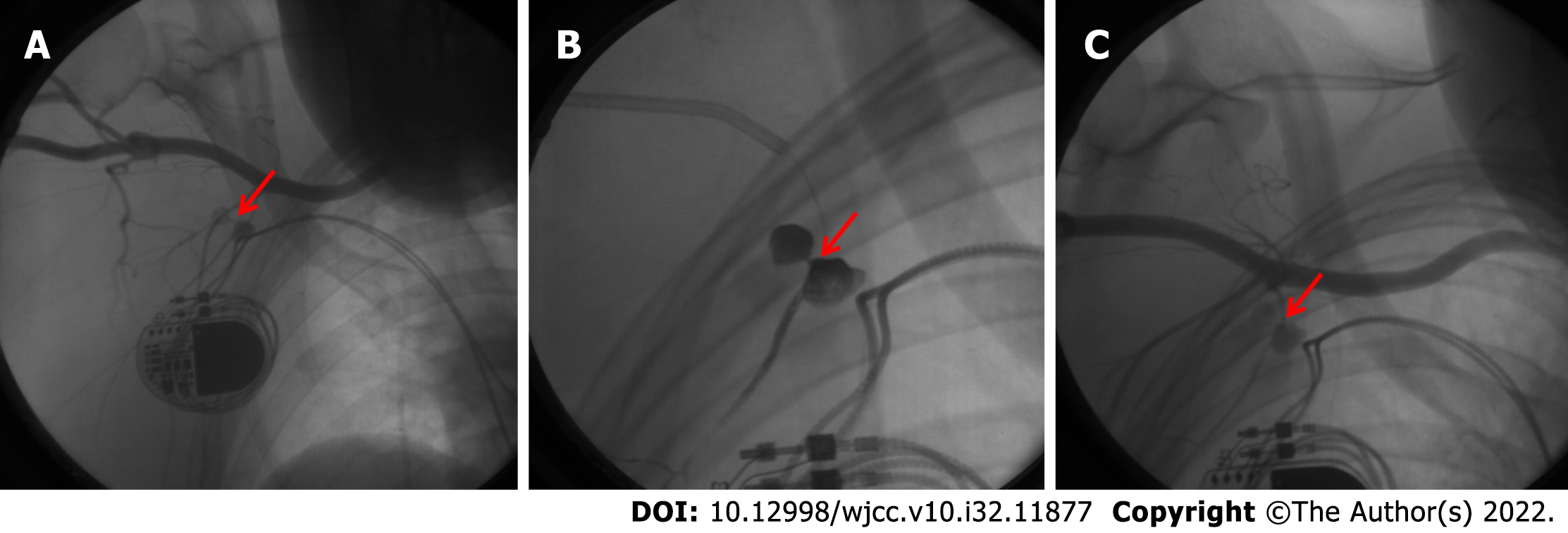
Conservative treatment, including local package compression, haemostatic drugs, and blood transfusions, was unsatisfactory. The next day, subclavian artery angiography in the digital subtraction angiography room showed that the first branch of the right subclavian artery was a trefoil pseudoaneurysm (Figure 2A).
This is a haematoma from complications of pseudoaneurysm due to axillary vein puncture during operation. The clinician considered the possible cause was accidental puncturing of a small branch of the right subclavian artery, which developed into a pseudoaneurysm and resulted in further haematoma formation.
Transcatheter arterial embolization by Onyx rubber was performed in the arterial aneurysm and distal vasculature (Figure 2B). Onyx rubber is a non-viscous embolic agent made from a mixture of ethylene-vinyl alcohol copolymer, dimethyl sulphoxide and tantalum powder[5]. It is a novel liquid embolism commonly used in the treatment of cerebrovascular diseases.
After the operation, angiography showed no aneurysm in the right subclavian artery (Figure 2C). During the follow-up, ultrasonography showed that the haematoma was absorbed gradually.
Haematoma is one of the major complications following pacemaker implantation. However, pocket haematoma is mostly represented in previous studies, and other forms of haematoma are relatively rare[6,7]. Haematoma will increase the risk of pacemaker infection, and may affect the pacemaker function, resulting in serious consequences[8]. Previous studies stated that the reasons for haematoma are as follows: (1) Coagulation disorder, long-term prescription of anticoagulant/antiplatelet drugs preoperatively and self-disorder of coagulation may lead to bleeding[9-11]; (2) Individual factors, including old age, marasmus, and underlying diseases, are more likely to produce a “dead cavity” of the pacemaker pocket because of thinner subcutaneous tissue, which increases the risk of bleeding. Guo et al[12] reported that a BMI < 23 kg/m2 was associated with a higher incidence of pocket haematoma; and (3) Intraoperation factors, including accidental injury of arterioles, venules and capillaries, incomplete haemostasis, oversize pocket, effective fixation of lead and insecure suture, may increase the risk of bleeding.
The chest wall haematoma in this case was not a common pocket haematoma. According to the results of ultrasonography and CTA, accidental injury of a small branch from the right subclavian artery is considered to be the reason for pseudoaneurysm. Pseudoaneurysm is a rare iatrogenic injury during pacemaker implantation, and only a few cases have been reported previously[13,14]. Pseudoaneurysms is a ruptured artery surrounded by unstable connective tissue containing a haematoma. The haematoma forms outside the arterial wall, so it is contained by the surrounding tissues, which is one of the complications of cardiovascular intervention. Untreated pseudoaneurysm may generate angiorrhexis, thromboembolism, local compression, tissue necrosis and even severe bleeding[15]. Therefore, it is essential to manage pseudoaneurysms in a timely, accurate and safe manner. More possible factors should be taken into consideration as haematoma is discovered in cases of severe adverse events.
Previous studies have shown that haematoma is one of the main complications following permanent pacemaker implantation, and most of them are pocket haematoma. As a relatively rare clinical condition, pseudoaneurysm is not easy to be detected due to its atypical symptoms and physical signs, which often leads to delayed treatment and serious adverse event. In this case, the haematoma caused by accidental injury to the subclavian artery branch was successfully treated by transcatheter arterial embolization and the prognosis was satisfactory. The aim of this case report is to remind clinicians to consider other rare conditions, including pseudoaneurysm, in addition to pocket haematoma, in the presence of suspected internal bleeding after pacemaker implantation.
We thank all the medical staff members who were involved in treating the patient. Special thanks to Qiang Hu from Department of Vsculr Surgery and Dan-Dan Mao from Department of Neurosurgery for their great supporting during this work.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Cardiovascular Branch of Zhejiang Medical Association; Association of Integrated Chinese and Western Medicine.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kubo T, Japan; Schoenhagen P, United States S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac Pacemakers: Function, Troubleshooting, and Management: Part 1 of a 2-Part Series. J Am Coll Cardiol. 2017;69:189-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 139] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 2. | Polyzos KA, Konstantelias AA, Falagas ME. Risk factors for cardiac implantable electronic device infection: a systematic review and meta-analysis. Europace. 2015;17:767-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 281] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 3. | Tarakji KG, Korantzopoulos P, Philippon F, Biffi M, Mittal S, Poole JE, Kennergren C, Lexcen DR, Lande JD, Seshadri S, Wilkoff BL. Infectious consequences of hematoma from cardiac implantable electronic device procedures and the role of the antibiotic envelope: A WRAP-IT trial analysis. Heart Rhythm. 2021;18:2080-2086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Chen P, Yang M, Han L. Cause analysis and prevention of pacemaker pocket hematoma. Zhejiang Linchuang Yixue. 15:1322-1323. |
| 5. | Lanzino G, Burrows AM, Cloft HJ. Onyx embolization. J Neurosurg. 2014;120:375-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | DE Sensi F, Miracapillo G, Cresti A, Severi S, Airaksinen KE. Pocket Hematoma: A Call for Definition. Pacing Clin Electrophysiol. 2015;38:909-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Mehta NK, Doerr K, Skipper A, Rojas-Pena E, Dixon S, Haines DE. Current strategies to minimize postoperative hematoma formation in patients undergoing cardiac implantable electronic device implantation: A review. Heart Rhythm. 2021;18:641-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Clémenty N, Fernandes J, Carion PL, de Léotoing L, Lamarsalle L, Wilquin-Bequet F, Wolff C, Verhees KJP, Nicolle E, Deharo JC. Pacemaker complications and costs: a nationwide economic study. J Med Econ. 2019;22:1171-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Chow V, Ranasinghe I, Lau J, Stowe H, Bannon P, Hendel N, Kritharides L. Peri-procedural anticoagulation and the incidence of haematoma formation after permanent pacemaker implantation in the elderly. Heart Lung Circ. 2010;19:706-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Thal S, Moukabary T, Boyella R, Shanmugasundaram M, Pierce MK, Thai H, Goldman S. The relationship between warfarin, aspirin, and clopidogrel continuation in the peri-procedural period and the incidence of hematoma formation after device implantation. Pacing Clin Electrophysiol. 2010;33:385-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Sohail MR, Uslan DZ, Khan AH, Friedman PA, Hayes DL, Wilson WR, Steckelberg JM, Stoner S, Baddour LM. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol. 2007;49:1851-1859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 500] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 12. | Guo JP, Shan ZL, Guo HY, Yuan HT, Lin K, Zhao YX, Wang YT. Impact of body mass index on the development of pocket hematoma: A retrospective study in Chinese people. J Geriatr Cardiol. 2014;11:212-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Vandenbulcke R, Marrannes J, Maleux G. Pseudo-aneurysm as rare complication after pacemaker implantation. Acta Cardiol. 2017;72:220. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Sharma A, Pandey NN, Kumar S. Pacemaker site pseudoaneurysm from superior thoracic artery: an uncommon offender. Acta Cardiol. 2019;74:538-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Peters S, Braun-Dullaeus R, Herold J. Pseudoaneurysm. Hamostaseologie. 2018;38:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |