Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11204
Peer-review started: August 16, 2022
First decision: September 5, 2022
Revised: September 7, 2022
Accepted: September 23, 2022
Article in press: September 23, 2022
Published online: October 26, 2022
Processing time: 65 Days and 12.2 Hours
High-intensity focused ultrasound (HIFU) ablation is a minimally invasive approach in gynecology that is used to manage uterine fibroids. Although this procedure is safe and effective, adverse outcomes are becoming a major problem.
We present a case of ventral hernia that occurred as a rare and delayed com
High-intensity ultrasound ablation should be performed only on appropriate candidates. Patients should be educated about potential complications of the procedure and the possibility of subsequent treatment. Post-procedural long-term follow-up for detecting delayed adverse effects is important.
Core Tip: We report a case of ventral hernia induced by ultrasound-guided high-intensity focused ultrasound (HIFU) ablation for the management of uterine fibroids. The case highlights the importance of long-term follow-up for delayed and rare complications after HIFU ablation.
- Citation: Park JW, Choi HY. Ventral hernia after high-intensity focused ultrasound ablation for uterine fibroids treatment: A case report. World J Clin Cases 2022; 10(30): 11204-11209
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11204.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11204
High-intensity focused ultrasound (HIFU) is a nonsurgical therapeutic technique for uterine fibroids. It is a desirable option for patients who want to save the uterus, regardless of fertility preservation. Recent studies reported favorable clinical outcomes in HIFU compared to conventional surgery and other non-invasive treatments[1-3]. However, despite the proven safety and efficacy of HIFU, adverse responses remain a concern. Here, we present the case of a patient who presented with delayed abdominal bloating after ultrasound-guided HIFU (USgHIFU) ablation.
A 43-year-old woman presented to the outpatient clinic with abdominal bloating, which had started 6 mo prior.
She had undergone USgHIFU for treatment of uterine fibroids at a private hospital 1 year prior to presentation.
The patient had a uterine fibroid with a maximal diameter of 8 cm. She underwent USgHIFU ablation to reduce the size of the uterine fibroid, which decreased to 6.2 cm after the procedure. She did not have any history of trauma or weight change. She had no history of previous surgical procedures or relevant illnesses.
The patient denied having any relevant personal or familial history.
Her body mass index was 23.8 kg/m2. Her abdominal exam was significant for distension without tenderness and a 10 cm palpable mass in the lower left quadrant. She had no fever. The cervical examination presented no remarkable findings, such as vaginal discharge or odor.
Findings of laboratory examinations in blood and urine were unremarkable.
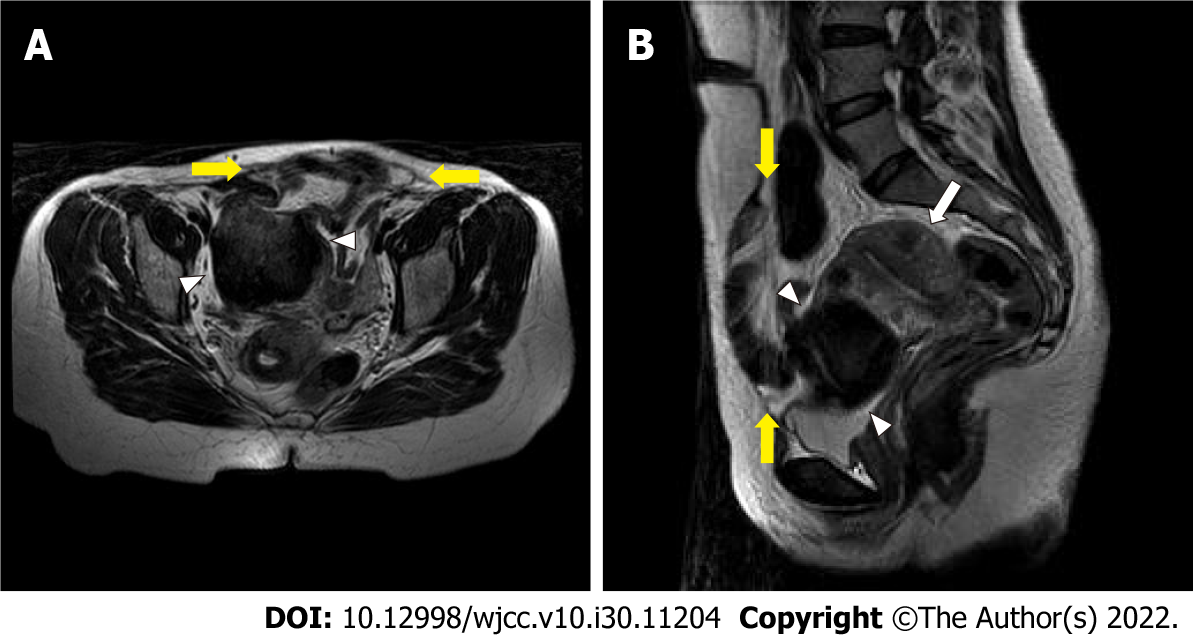
Transvaginal sonography revealed a 7-cm-sized uterine fibroid and a fascial defect in the left lower abdomen. Subsequent magnetic resonance imaging scans revealed that the uterine fibroid and the defect measuring 11 cm × 10 cm in the left rectus abdominis muscle were located at the USgHIFU treatment site (Figure 1A and B).
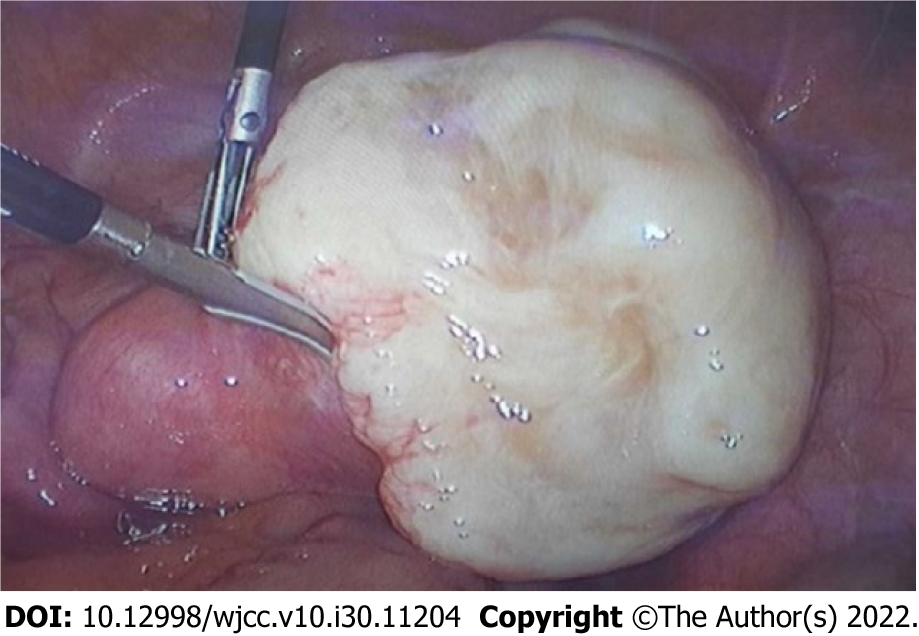
A diagnostic laparoscopy was performed, and subserosal fibroid and ventral hernia were identified in the operating room (Figures 2 and 3). The defect of the left rectus abdominis muscle measured 13 cm × 12 cm.
Considering intraoperative findings, the final diagnosis was a ventral hernia induced by USgHIFU.
We performed a total laparoscopic hysterectomy with bilateral salpingectomy for curative treatment of the uterine fibroid at the patient’s request. Concurrently, ventral herniorrhaphy was performed with a 20 cm × 15 cm sized composite mesh. Pathological examination confirmed the diagnosis of leiomyoma with red degeneration. The patient was discharged in good condition on postoperative day 5.
All the symptoms, including abdominal bloating and palpable mass, improved after the surgery. Follow-up was performed for 3 years in an outpatient setting, and no further complications were identified.
Uterine fibroid is one of the most common gynecologic diseases in reproductive women, with prevalence varying widely from 4.5% to 68.6% depending on countries and diagnostic methods[4]. The treatment goal is to improve fibroid-related symptoms, such as abnormal uterine bleeding, dysmenorrhea, and bulk symptoms, considering the patient’s health status and need for fertility preservation[5]. Management options include medical, interventional, and surgical therapies[5-6]. Traditionally, hysterectomy is an effective and definitive surgical treatment for uterine fibroid[6]. As the patient’s desire to retain the uterus increases regardless of fertility preservation, myomectomy and interventional treatments, which include myolysis, uterine artery embolization, and HIFU, tend to increase in all age groups, even in perimenopausal women[7].
HIFU ablation is a novel therapeutic modality that induces coagulative necrosis of the uterine fibroid and treats it. It has been widely used since the 2000s and has gained acceptance as an effective noninvasive treatment[8-10]. A recent study reported long-term outcomes of up to 8 years of HIFU treatment for symptomatic fibroids[11]. Patients who underwent HIFU ablation showed higher symptom relief rates, lower symptom recurrence rates, and fewer complications compared to those who underwent uterine-sparing surgeries[11].
Although the safety and efficacy of HIFU have been demonstrated, adverse outcomes remain a concern. Complications of HIFU ablation vary from mild to severe. The commonly experienced minor complaints include lower abdominal pain and vaginal discharge, which subside in most patients within one week[12-13]. However, major adverse effects are uncommon with incidences of 0.14% to 0.38%, including skin burns, leg pain, sciatic nerve injury, and bowel injury[12-13]. Given the advancements of HIFU since its introduction, the major complications have seemingly decreased[10]. However, unexpected and serious problems, such as vertebral osteomyelitis and incarcerated internal hernia, have been reported[14-15].
In our case, the abdominal muscles were atrophied following HIFU ablation, resulting in late ventral hernia, which is a rare and critical complication requiring surgical repair. An acquired ventral hernia is common after surgery but rare after a non-invasive procedure. It may be caused by inaccurate targeting and use of excessive power during USgHIFU. However, immediate detection of inappropriate power settings that cause thermal damage in USgHIFU is challenging, as it is difficult to monitor real-time temperature[9]. Yin et al[16] reported several susceptibility factors for thermal damage to the wall structure, including thick abdominal wall, presence of abdominal scar, and excessive total energy for ablation. Thermal injury following HIFU ablation can occur in any abdominal structure, but extensive destruction of the muscle layers is uncommon.
In addition to critical side effects, the possibility of requiring subsequent therapy is an inherent limitation of HIFU ablation as an interventional treatment for uterine fibroid. Choe et al[17] analyzed the characteristics of patients who underwent additional surgery after HIFU ablation to treat uterine fibroids[16]. Patients with uterine fibroids measuring greater than 10 cm and in multiple numbers, as well as persistent symptoms after HIFU ablation, have a higher risk of post-procedural operation[17]. In a recent study, the risk factors for reintervention, including secondary HIFU ablation and conventional surgeries, were reported as young age, large-sized uterine fibroid, and submucosal uterine fibroid[18]. In 72.2% of the patients, the reintervention occurred mainly between 2-4 years after the procedure[18]. Therefore, this period is critical for judging the patient’s progress during the follow-up period, particularly for patients who have risk factors for reintervention.
Enjoying the advantages of new treatments should not prevent efforts to achieve better outcomes. Therefore, HIFU ablation must only be performed on carefully selected patients. Although HIFU ablation is considered an optimal, conservative therapy, physicians should discuss the possible need for subsequent intervention with their patients. Patients must be educated and encouraged to report complaints after HIFU therapy to detect unexpected complications. A long-term follow-up may be required to monitor for delayed adverse outcomes and decide on appropriate additional treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yao J, China; Zhao K, China S-Editor: Wang DM L-Editor: A P-Editor: Wang DM
| 1. | Wang Y, Geng J, Bao H, Dong J, Shi J, Xi Q. Comparative Effectiveness and Safety of High-Intensity Focused Ultrasound for Uterine Fibroids: A Systematic Review and Meta-Analysis. Front Oncol. 2021;11:600800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Ji Y, Hu K, Zhang Y, Gu L, Zhu J, Zhu L, Zhu Y, Zhao H. High-intensity focused ultrasound (HIFU) treatment for uterine fibroids: a meta-analysis. Arch Gynecol Obstet. 2017;296:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Wang F, Tang L, Wang L, Wang X, Chen J, Liu X, Gong Y. Ultrasound-guided high-intensity focused ultrasound vs laparoscopic myomectomy for symptomatic uterine myomas. J Minim Invasive Gynecol. 2014;21:279-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Stewart EA, Cookson CL, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124:1501-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 679] [Cited by in RCA: 572] [Article Influence: 71.5] [Reference Citation Analysis (0)] |
| 5. | Giuliani E, As-Sanie S, Marsh EE. Epidemiology and management of uterine fibroids. Int J Gynaecol Obstet. 2020;149:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 303] [Article Influence: 60.6] [Reference Citation Analysis (1)] |
| 6. | American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Gynecology. Management of Symptomatic Uterine Leiomyomas: ACOG Practice Bulletin, Number 228. Obstet Gynecol. 2021;137:e100-e115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 116] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 7. | Lee M, Chung YJ, Kim HK, Hwang H, Park JY, Shin I, Kim C, Cho HH, Kim M, Jung CY, Chae KH, Kim S, Kim MR. Estimated Prevalence and Incidence of Uterine Leiomyoma, and Its Treatment Trend in South Korean Women for 12 years: A National Population-Based Study. J Womens Health (Larchmt). 2021;30:1038-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Chen J, Chen W, Zhang L, Li K, Peng S, He M, Hu L. Safety of ultrasound-guided ultrasound ablation for uterine fibroids and adenomyosis: A review of 9988 cases. Ultrason Sonochem. 2015;27:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 9. | Cheung VYT, Lam TPW, Jenkins CR, Lam SW, Cheung GKI, Chan SSY, Choi WK. Efficacy and safety of ultrasound-guided high-intensity focused ultrasound for uterine fibroids: a preliminary experience. J Obstet Gynaecol. 2019;39:833-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Chen J, Li Y, Wang Z, McCulloch P, Hu L, Chen W, Liu G, Li J, Lang J; Committee of the Clinical Trial of HIFU vs Surgical Treatment for Fibroids. Evaluation of high-intensity focused ultrasound ablation for uterine fibroids: an IDEAL prospective exploration study. BJOG. 2018;125:354-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 11. | Wang Y, Liu X, Wang W, Tang J, Song L. Long-term Clinical Outcomes of US-Guided High-Intensity Focused Ultrasound Ablation for Symptomatic Submucosal Fibroids: A Retrospective Comparison with Uterus-Sparing Surgery. Acad Radiol. 2021;28:1102-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Liu Y, Zhang WW, He M, Gong C, Xie B, Wen X, Li D, Zhang L. Adverse effect analysis of high-intensity focused ultrasound in the treatment of benign uterine diseases. Int J Hyperthermia. 2018;35:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Zhang L, Zhang W, Orsi F, Chen W, Wang Z. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: A review of safety and efficacy. Int J Hyperthermia. 2015;31:280-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 14. | Hwang DW, Song HS, Kim HS, Chun KC, Koh JW, Kim YA. Delayed intestinal perforation and vertebral osteomyelitis after high-intensity focused ultrasound treatment for uterine leiomyoma. Obstet Gynecol Sci. 2017;60:490-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Choi H, Ryu DH, Lee JY, Xu K. High-intensity focused ultrasound (HIFU) for uterine myoma ablation caused incarcerated internal hernia. Indian J Surg. 2022;1-3. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Yin N, Hu L, Xiao ZB, Liu C, Chen WZ, Roberts N, Chen JY, Wang ZB. Factors influencing thermal injury to skin and abdominal wall structures in HIFU ablation of uterine fibroids. Int J Hyperthermia. 2018;34:1298-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Choe YS, Lee WM, Choi JS, Bae J, Eom JM, Choi E. Clinical characteristics of patients with leiomyoma who undergo surgery after high intensity focused ultrasound (HIFU). Obstet Gynecol Sci. 2019;62:258-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Li W, Jiang Z, Deng X, Xu D. Long-term follow-up outcome and reintervention analysis of ultrasound-guided high intensity focused ultrasound treatment for uterine fibroids. Int J Hyperthermia. 2020;37:1046-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |