Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11139
Peer-review started: June 25, 2022
First decision: August 1, 2022
Revised: August 9, 2022
Accepted: September 20, 2022
Article in press: September 20, 2022
Published online: October 26, 2022
Processing time: 117 Days and 17.4 Hours
Perirectal epidermoid cysts are rare masses arising from the ectodermal germ cell layer of the hindgut and are predominantly found in middle-aged women. It is often difficult to make an accurate diagnosis of these cysts and it is equally challenging to distinguish it from other developmental cysts.
We report the case of an 18-year-old female patient with a perirectal mass who presented to the hospital with constipation. The patient experienced sacrococcygeal falls and burns on the left buttocks during growth. Three-dimensional computed tomography scans indicated abnormal sacral vertebrae with the sacral canal partially enlarged and opened. Pelvic magnetic resonance imaging showed a 55 mm × 40 mm × 35 mm unilocular cystic mass in the perirectal space and a solitary sinus in the left ischiorectal fossa. The cyst was completely resected posteriorly using the sacrococcygeal approach. The pathology was verified to be an epidermoid cyst. The patient remained recurrence-free after 6 mo of follow-up.
Successful treatment of perirectal epidermoid cysts depends on comprehensive evaluation. This is significant for the surgical approach and prognosis.
Core Tip: Perirectal cystic mass is a rare congenital developmental abnormality. An 18-year-old female was found with a perirectal mass due to defecation difficulties. She had suffered from sacrococcygeal falls and burns on the left buttocks during the growth experience. We performed a complete preoperative evaluation of this patient. Three-dimensional computed tomography scans showed that there was no damage to the sacral surface bone. Pelvic magnetic resonance imaging showed that the perirectal mass had a complete membrane without enhancement signs and no potential connection with the perianal sinus and sacral canal. Finally, the mass was completely removed through the sacrococcygeal approach and verified as an epidermoid cyst in histology. This case highlights the need to improve evaluation in the differential diagnosis of perirectal mass.
- Citation: Ji ZX, Yan S, Gao XC, Lin LF, Li Q, Yao Q, Wang D. Perirectal epidermoid cyst in a patient with sacrococcygeal scoliosis and anal sinus: A case report. World J Clin Cases 2022; 10(30): 11139-11145
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11139.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11139
Epidermoid cysts are commonly found in different parts of the body; however, perirectal epidermoid cysts are extremely rare. Perirectal cysts are congenital abnormalities considered to originate from caudal embryonic vestiges[1]. Perirectal epidermoid cysts occur mostly in middle-aged women; however, they are rare in younger women[2]. An abnormal mass in the pelvic floor space is often in
An 18-year-old female patient presented to the clinic with a complaint of constipation.
The patient had difficulty in evacuating her bowels for 2 mo.
Three months after birth, the patient suffered from sacrococcygeal deformity due to an accidental fall and underwent an imaging examination at the local hospital without any therapy. At age five, her left buttock was scalded with boiling water.
The patient had no family history of inflammatory bowel disease or hereditary tumors.
No abnormalities were found upon abdominal examination. Her buttocks were asymmetrical with irregular scar hyperplasia and shrinkage observed at the four o'clock position, which was approximately 3 cm away from the anal opening. Physical examination revealed a soft, mobile and poorly circumscribed mass without tenderness in the right perirectal region. The sacrum and coccyx were displaced to the right. Digital rectal examination revealed a bulge in the retrorectal area resulting in mild stenosis of the lumen (Figure 1).
Laboratory test results were normal.
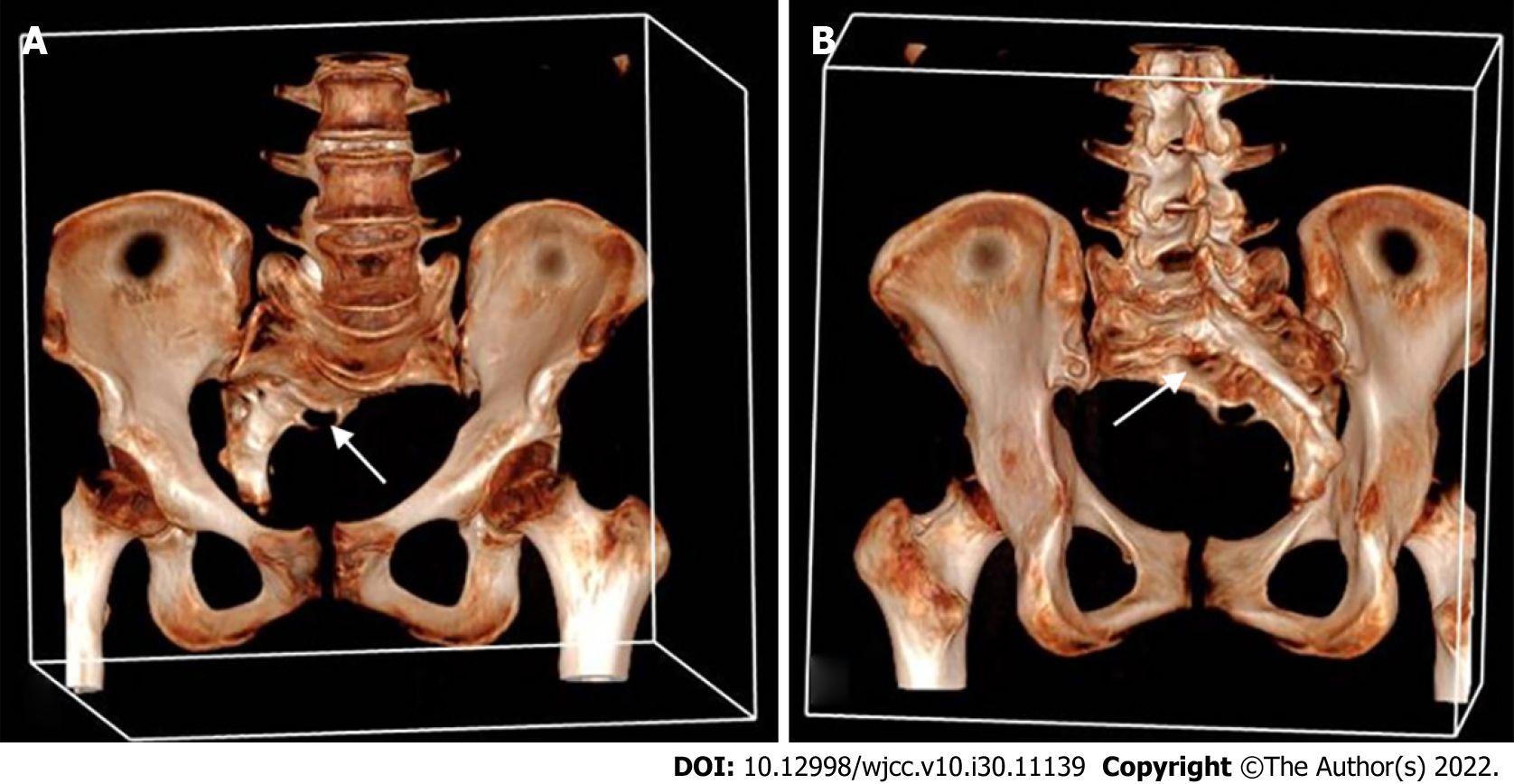
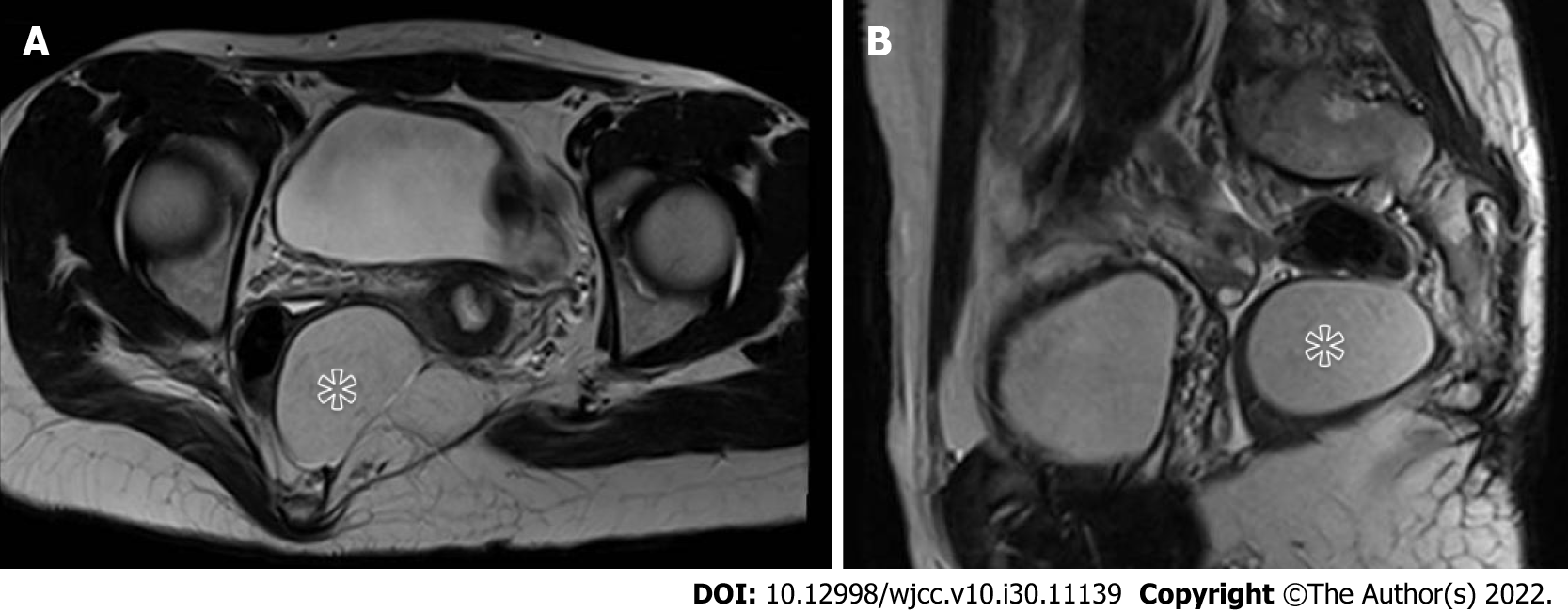
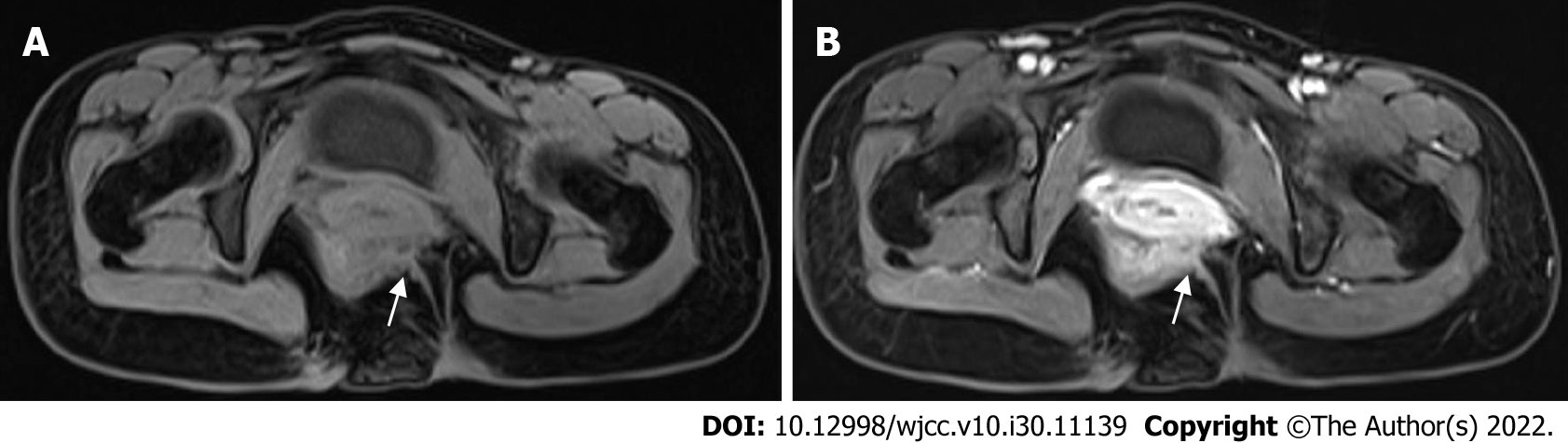
Colonoscopy revealed a slight stenosis of the area between the rectum and anal canal without erosion, ulceration or tumor formation. Three-dimensional (3D) computed tomography (CT) revealed abnormal sacral vertebrae with the sacral canal partially enlarged and opened. No destruction of the local sacral bone was observed (Figure 2). Magnetic resonance imaging (MRI) revealed a 55 mm × 40 mm × 35 mm well-circumscribed unicameral cystic mass in the pelvis that adhered to the left rectal wall posteriorly to the sacrum resulting in a right anterior displacement of the rectum. The vaginal wall was compressed and wrinkled (Figure 3). Enhanced strips in the scan extended from the levator ani muscle to the skin of the left buttock (Figure 4). Based on the MRI findings, preoperative diagnoses included a presacral epidermoid cyst, anal sinus and sacrococcygeal scoliosis.
The cystic mass was identified to be an epidermoid cyst.
The cystic mass did not affect the patient’s spine and the sinus in her left buttock showed no signs of infection. Complete surgical excision was performed using the posterior transsacrococcygeal approach. The patient was placed in the jackknife position after spinal anesthesia. A longitudinal median incision was made over the mass of the body surface on the left side of the coccyx. The skin, subcutaneous tissue, fat layer and levator ani muscle were cut layer by layer to reveal the space of pelvic floor. The cystic mass was firmly attached to the puborectalis and left posterior wall of the lower rectum. Using both blunt and sharp dissection to carefully dissect the surrounding anatomical structures, the cyst was completely excised. The cyst measured 55 mm × 40 mm × 35 mm and was filled with a soybean curd residue-like material. The rectum was confirmed to be intact by using an intraoperative anoscope. The space of the pelvic floor was stitched into layers with a drainage tube left in situ. Histologically, the cystic cavity was covered with squamous epithelium and composed of gray and white cheese-like layered keratinocytes mixed with exfoliated broken epidermal cells, keratin and cholesterol.
After surgery, the patient was hospitalized for purgative and preventive antibacterial treatment. We changed the dressing after defecation twice daily. The patient was discharged 2 wk after the surgery with a drain and the stitches were removed.
Six months after surgery, the patient remained recurrence-free.
The presacral space is a triangular space between the posterior sacrum and anterior rectum that is bounded by the peritoneal reflection superiorly and levator ani muscles inferiorly[4]. Developmental cystic masses arising from the presacral space include several kinds of tumors including dermoid cysts, epidermoid cysts, chordomas, adrenal rest tumors, anterior sacral meningoceles, cystic hamartomas, tailgut and rectal duplication cysts[5]. Epidermoid cysts in the presacral space are uncommon with an incidence of 1 in 40000-63000 hospital admissions and 60% of perirectal epidermoid cysts are congenital developmental cysts[6].
Perirectal epidermoid cysts are typically slow-growing; approximately 26%-50% of patients are asymptomatic and they are usually incidentally discovered during imaging[7]. Compression of pelvic structures by an enlarging cyst may present with urinary complaints, constipation, perianal pain or a palpable mass in the precoccygeal region. When there is an infection, these masses may result in per
Elevated levels of AFP or HCG may be indicative of germ cell tumors. Colonoscopy may reveal extrinsic rectal compression and exclude intestinal space-occupying lesions. Transrectal ultrasonography may be useful for assessing the location and extent of small cystic masses and their connection with the anal sphincter[11]. CT examination clearly showed bone destruction by malignant presacral masses. MRI is superior to CT in differentiating between any bone, spinal canal or meningeal involvement and its relationship with surrounding soft tissues and organs to determine the appropriate surgical plan[12]. Although infections, hemorrhages or calcifications in these lesions may alter the signal intensity, subtle changes in the signal intensity favor epidermoid cysts. However, these findings are not specific. Except for suspicious cancerous lesions, preoperative biopsy should not be performed to prevent tumor dissemination, abscess, fecal fistula or meningitis[1].
Choosing a surgical plan for presacral tumors largely depends on the tumor’s location, size and relationship with surrounding tissues and organs. Common surgical approaches are transsacrococcygeal, transabdominal, transsphincter and combined transabdominal and transsacral approaches[13]. If the mass is small (≤ 10 cm), located at the caudal level (below S4) and does not invade surrounding structures, the sacral approach is usually adopted[14]. When the mass is located at a high spinal level (above S3), the transabdominal approach is a better option. When the mass is large, its location near surrounding organs such as the ureter and iliac vessels is unclear and it is difficult to employ a single approach; thus, the combined abdominal sacrococcygeal approach can be selected[A4]. The sphincter approach is an option for patients with small, low-lying lesions[15]. Gynecologists choose the transvaginal approach because it provides a sufficient field of vision, shorter operative time and lower blood loss in low-lying retrorectal lesions[16].
The differential diagnoses of perirectal cystic lesions include tailgut cysts, cystic teratomas, chordomas and anterior sacral meningoceles[17-20]. In female patients, a high (in terms of location) perirectal mass is misdiagnosed as ovarian cystadenoma[21]. The unique feature of this case is that a perirectal mass with perianal sinus and sacrococcygeal malformation was found in a young female patient. To accurately determine the extent of the mass lesion and rule out other pathologies, the patient underwent several imaging examinations. MRI revealed a solitary abscess in the left ischiorectal fossa which had no sinus interacting with the presacral mass. Given the patient’s history of scalding, sterile necrotic tissue may have accumulated in the perianal sinus. Three-dimensional CT scans revealed an abnormal sacral vertebra with the sacral canal partially enlarged and opened; however, there was no damage to the sacral surface bone. The wall of the cyst was remote from the sacral canal, the opened sacral canal was at the S3 Level and the cyst was below S4. Evidence of an anterior sacral meningocele is insufficient. Although extremely rare, benign cysts can also progress into malignant tumors[22]. In our case, a well-defined smooth margin with an absence of invasion may have helped differentiate it from malignant masses. This case highlights the importance of pre-operative imaging and evaluation to identify the nature of the presacral mass which is crucial for surgery and prognosis.
Laparoscopic surgery is an option because of its minimal invasiveness, low risk of complications and complete tumor removal. Considering that the patient was a young female who had not given birth, surgery was performed using the transsacrococcygeal approach to avoid damaging the pelvic organ. During surgery, we cut the cystic mass to reduce its volume for a larger operative space. In cases of suspected malignant tumors, it should be carefully stripped along the capsule to prevent rupture and metastasis. In this regard, the importance of preoperative differential diagnosis is emphasized.
Distinguishing an epidermoid cyst from other perirectal cystic masses is a significant diagnostic challenge. The clinical manifestations of presacral masses vary and once found, colonoscopy, sacrococcygeal CT and pelvic MRI findings should be further evaluated. Using the tumor’s location, size and relationship with the surrounding organs, an appropriate surgical plan should be selected.
We would like to thank Dr. He De, a chief physician from General Surgery, The Second Affiliated Hospital of Shenzhen University, Shenzhen, China.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Grossi U, Italy; Jain N; Koukoulis GD, Greece; Mijwil MM, Iraq S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Hawkins WJ, JACKMAN RJ. Developmental cysts as a source of perianal abscesses, sinuses and fistulas. Am J Surg. 1953;86:678-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 31] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Riojas CM, Hahn CD, Johnson EK. Presacral epidermoid cyst in a male: a case report and literature review. J Surg Educ. 2010;67:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Yang DM, Yoon MH, Kim HS, Oh YH, Ha SY, Oh JH, Chung HS. Presacral epidermoid cyst: imaging findings with histopathologic correlation. Abdom Imaging. 2001;26:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Atolagbe AO, Ogunleye O, Apakama CT. Bi-lobed Perirectal Epidermoid Cyst: An Unusual Cause of Hematochezia in a Middle-aged Woman. Ann Med Health Sci Res. 2016;6:190-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Yang BL, Gu YF, Shao WJ, Chen HJ, Sun GD, Jin HY, Zhu X. Retrorectal tumors in adults: magnetic resonance imaging findings. World J Gastroenterol. 2010;16:5822-5829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors. Mayo Clinic experience, 1960-1979. Dis Colon Rectum. 1985;28:644-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 229] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Baek SW, Kang HJ, Yoon JY, Whang do Y, Park DH, Yoon SG, Kim HS, Lee JK, Lee JD, Kim KY. Clinical Study and Review of Articles (Korean) about Retrorectal Developmental Cysts in Adults. J Korean Soc Coloproctol. 2011;27:303-314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Morgan MB, Stevens GL, Somach S, Tannenbaum M. Carcinoma arising in epidermoid cyst: a case series and aetiological investigation of human papillomavirus. Br J Dermatol. 2001;145:505-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Bullard Dunn K. Retrorectal tumors. Surg Clin North Am. 2010;90:163-171, Table of Contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Abramson RC, Morawetz RB, Schlitt M. Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery. 1989;24:574-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Glasgow SC, Birnbaum EH, Lowney JK, Fleshman JW, Kodner IJ, Mutch DG, Lewin S, Mutch MG, Dietz DW. Retrorectal tumors: a diagnostic and therapeutic challenge. Dis Colon Rectum. 2005;48:1581-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Paul PG, Pravinkumar T, Sheetal B. Sacrococcygeal neurofibroma: rare cause for chronic pelvic pain. J Minim Invasive Gynecol. 2012;19:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Saxena D, Pandey A, Bugalia RP, Kumar M, Kadam R, Agarwal V, Goyal A, Kankaria J, Jenaw RK. Management of presacral tumors: Our experience with posterior approach. Int J Surg Case Rep. 2015;12:37-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Akbulut S. Unusual cause of defecation disturbance: a presacral tailgut cyst. Eur Rev Med Pharmacol Sci. 2013;17:1688-1699. [PubMed] |
| 15. | Kanemitsu T, Kojima T, Yamamoto S, Koike A, Takeshige K, Naruse T. The trans-sphincteric and trans-sacral approaches for the surgical excision of rectal and presacral lesions. Surg Today. 1993;23:860-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Aslan E. Transvaginal excision of a retrorectal tumor presenting as rectocele. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1715-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Grossi U, Santoro GA, Sarcognato S, Iacomino A, Tomassi M, Zanus G. Perianal Tailgut Cyst. J Gastrointest Surg. 2021;25:558-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Park YJ. Multiple Presacral Teratomas in an 18-year-old Girl: A Case Report. J Korean Soc Coloproctol. 2011;27:90-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Permi HS, Kishan Prasad H, Veena S, Teerthanath S. Presacral chordoma diagnosed by transrectal fine-needle aspiration cytology. J Cytol. 2011;28:89-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Rege S, Tadghare J, Jatav G, Pounikar M. An Unusual Presentation as Recurrent Abortions in a Case of Giant Presacral Epidermoid Cyst Mimicking an Anterior Sacral Meningocele. World Neurosurg. 2019;122:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Jha A, Khalid M, Gupta P, Saud M, Gupta G. Presacral epidermoid cyst in an elderly female, mistaken for ovarian cystadenoma. J Obstet Gynaecol India. 2014;64:118-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Wu X, Chen C, Yang M, Yuan X, Chen H, Yin L. Squamous Cell Carcinoma Malignantly Transformed From Frequent Recurrence of a Presacral Epidermoid Cyst: Report of a Case. Front Oncol. 2020;10:458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |