Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11128
Peer-review started: June 25, 2022
First decision: July 14, 2022
Revised: July 20, 2022
Accepted: September 14, 2022
Article in press: September 14, 2022
Published online: October 26, 2022
Processing time: 117 Days and 18.1 Hours
Light-induced retinal damage is a serious vision-threatening disease, resulting from unsuitable laser irradiation, high-power light and sustaining light exposure. Therefore, effectively evaluate the morphological and functional of retinal damage is urgently needed. Now, we mainly reported three patients suffered from typical light irradiations.
Patient 1 suffered from old laser pointer irradiation and followed with amblyopia treatment. Patient 2 suffered from acute high-energy light irradiation. Patient 3 suffered from sustaining optical fiber irradiation. Detailed morphological and functional examinations of the retina revealed that the lesions of the three patients had many similar characteristics, such as macular morphological changes, patent pattern visual monitoring amplitude or peak time abnormalities, multi-fucus electroretinograms macular central amplitude density decreased.
In conclusion, light-induced retinopathy has many common features, which can help clinical medical staff to diagnose retinal photodamage diseases.
Core Tip: In this case report, we reported three typical cases of retinal damage caused by light-related irradiations. Through the summary of their common characteristics, we can deepen the understanding of retinal diseases caused by light irradiation, and provide theoretical basis for the prevention, clinical diagnosis and treatment of such diseases.
- Citation: Zhang X, Luo T, Mou YR, Jiang W, Wu Y, Liu H, Ren YM, Long P, Han F. Morphological and electrophysiological changes of retina after different light damage in three patients: Three case reports. World J Clin Cases 2022; 10(30): 11128-11138
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11128.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11128
No matter in the living environment or working environment, people must be exposed to a variety of light sources. Prolonged and continuous exposure or accidental exposure to strong light often causes serious damage to the eyes, some of which are even irreversible[1,2]. Generally speaking, there are two aspects of light damage in the human eye, including the damage of the refractive system (cornea, lens, etc.) and the photosensitive system (retina). For example, some studies have found that the electric light generated in the welding process can directly lead to corneal epithelial necrosis, resulting in acute electro-ophthalmia[3]. Some researchers also found that the incidence of cataract increases significantly after long-term ultraviolet irradiation[4,5]. Moreover, long-term blue light irradiation can directly damage the macula through photochemical effect[6].
Remarkably, retinal damage is often the most common, but also relatively serious in the process of light damage to the eye[7]. Recent studies found the case of a 13-year-old boy looking at a green diode laser with an average output of 154 MW reflected in a mirror. Fundus examination and auxiliary examination showed fracture macular thermal damage[8]. In addition, Turaka et al[9] reported a case of macular photodamage and made a mini-review. In the article, the authors cited a report from the Food and Drug Association, which stated that handheld laser Pointers emitting > 5 mW of power carry the risk of irreversible eye damage and skin burns. Alsulaiman SM reported the natural history and treatment outcomes of full-thickness macular holes caused by transient exposure to high-power handheld blue laser devices and concluded that transient exposure to high-power handheld laser devices can result in full-thickness macular holes[10].
In this case reports, we reported three typical cases of retinal damage caused by light-related irradiation. Through the summary of their common characteristics, we may deepen the understanding of retinal diseases caused by various light irradiation, and provide theoretical basis for the prevention, clinical diagnosis and treatment of such diseases.
Patient 1: A 13-year-old female student who was in amblyopia treatment process for one year. However, her vision acuity didn’t benefit from the treatment and her parents asked us to perform total ophthalmological examination to make a decision whether to continue the amblyopia treatment or not.
Patient 2: A 22-year-old male soldier whose right eye was instantaneous irradiated by high energy flashlight one month ago. He didn’t pay close attention to it at that time. Then, his right eye vision decreased 5 d later without photophobia, tears, eye pain and other symptoms. No remission was found after self-administration of eye drops (unknown details). Therefore, he went to our hospital for further treatment.
Patient 3: A 33-year-old male communications engineer was in a history of physical fitness. Half a year ago, his left eye vision decreased without obvious photophobia, tears and eye pain. Although he found symptoms, he did not receive treatment. Recently, he went to our hospital and complained his vision decreased significantly.
Patient 1: There was a history of laser pointer exposure.
Patient 2: His right eye was instantaneous irradiated by high energy flashlight one month ago.
Patient 3: He had a long-term history of fiber-optic operation.
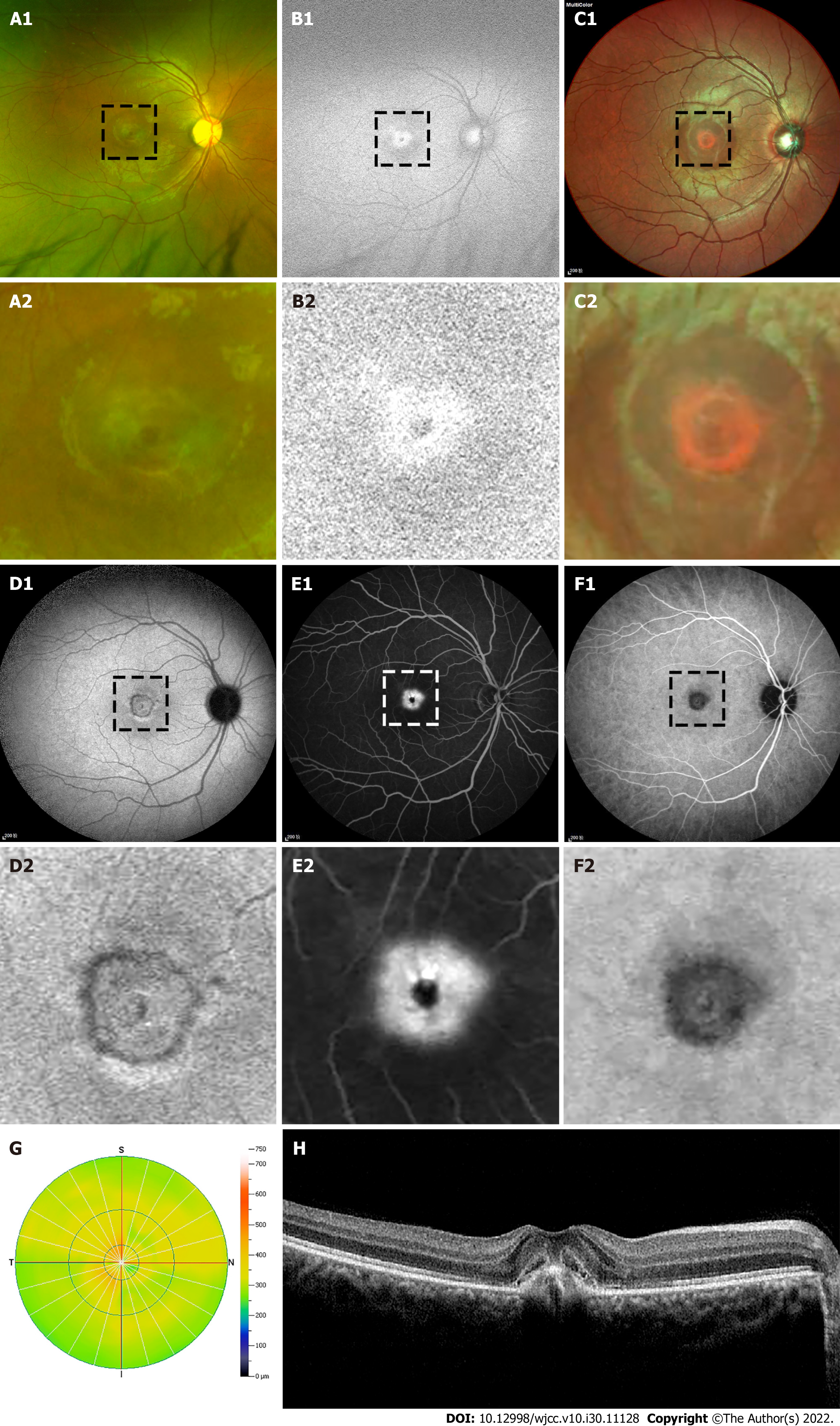
Patient 1: Then vision examination found the best corrected vision acuity (BCVA) was 1.0 in the right eye, and 0.4 in the left eye. In addition, the anterior segment was normal and the refractive medium was transparent in both eyes. Funduscopic and auto-fluorescence examination of left eye revealed a rough and uneven abnormality of macular (Figure 1A and B).
Patient 2: Specialist examination displayed that the patient’s BCVA was 0.3 in the right eye and 1.0 in the left eye. The anterior segment was normal and the refractive medium was transparent in both eyes.
Patient 3: Specialist examination found that the patient’s BCVA was 1.0 in the right eye and 0.6 in the left eye. The anterior segment was normal and the refractive medium was transparent in both eyes.
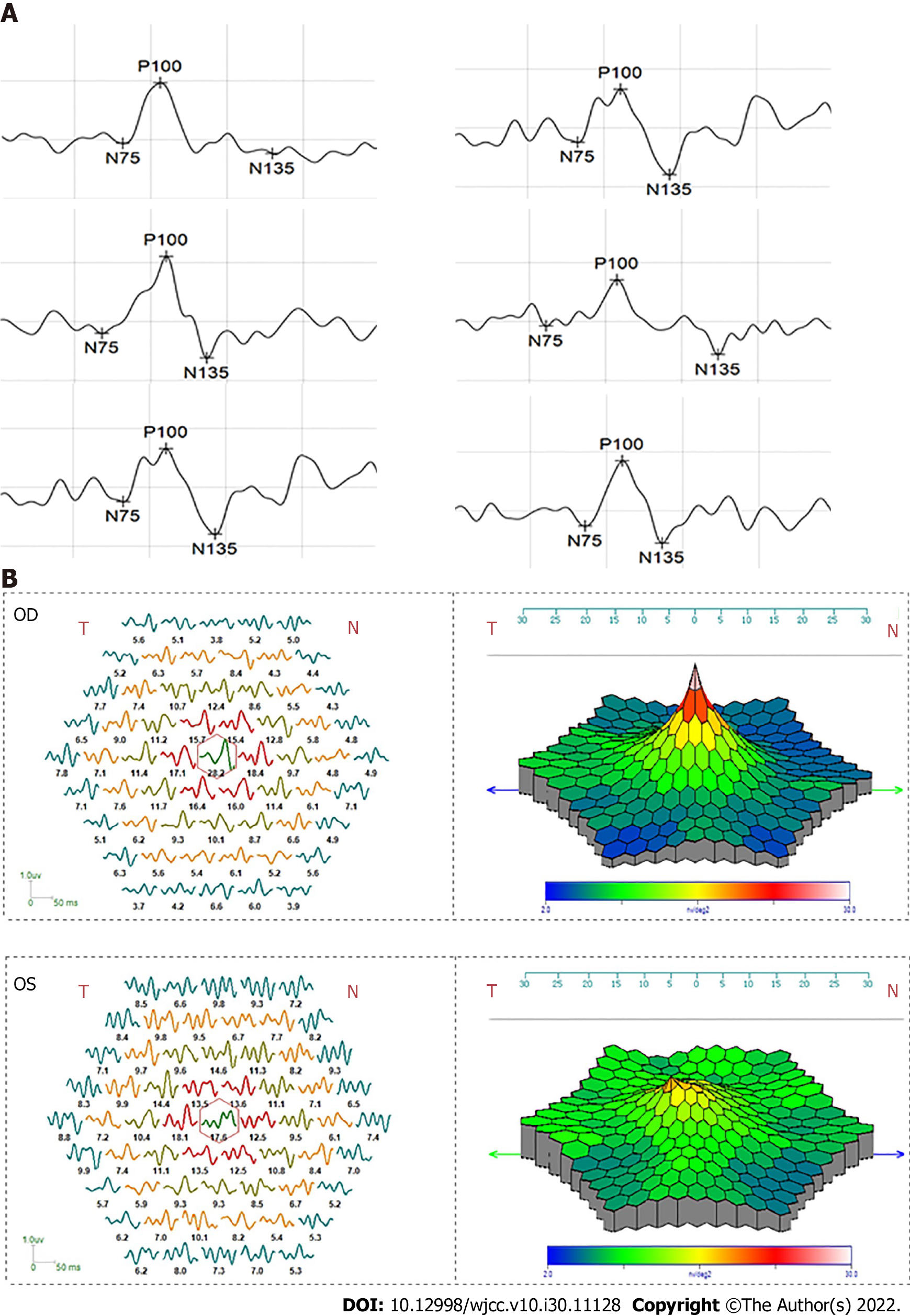
Patient 1: Angiography found a hyper-fluorescence feature and no fluorescent leakage at left eye macular (Figure 1C). Optical coherence tomography (OCT) showed that the macular had scar-like injury involving retinal pigment epithelium (Figure 1D and E). Meanwhile, the visual electrophysiological results indicated that the amplitude of P100 of pattern visual evoked potentials (PVEP) was reduced (Figure 2A), and full field electroretinogram (ffERG) was normal, and the amplitude density of multi-fucus electroretinograms (mfERG) macular center decreased (Figure 2B).
Patient 2: Funduscopic and auto-fluorescence examination of right eye revealed a black shape punctuation abnormality surrounded with a ringlike margin lesion (Figure 3A-D). Angiography (FFA + ICGA) found a macular hyper-fluorescence leakage around a black shape punctation at right eye (Figure 3E and F). OCT showed that the macular cystoid edema was significant, retinal pigment epithelium (RPE) layer of centra macular site was broken and choroidal neovascularization (CNV) was found in the right eye (Figure 3G and H). Meanwhile, the electrophysiological results showed that the amplitude of P100 of PVEP in right eye declined while the peak time was delayed (Figure 4A). FVEP and ffERG were normal, and the amplitude density of mfERG macular center was decreased (Figure 4B).
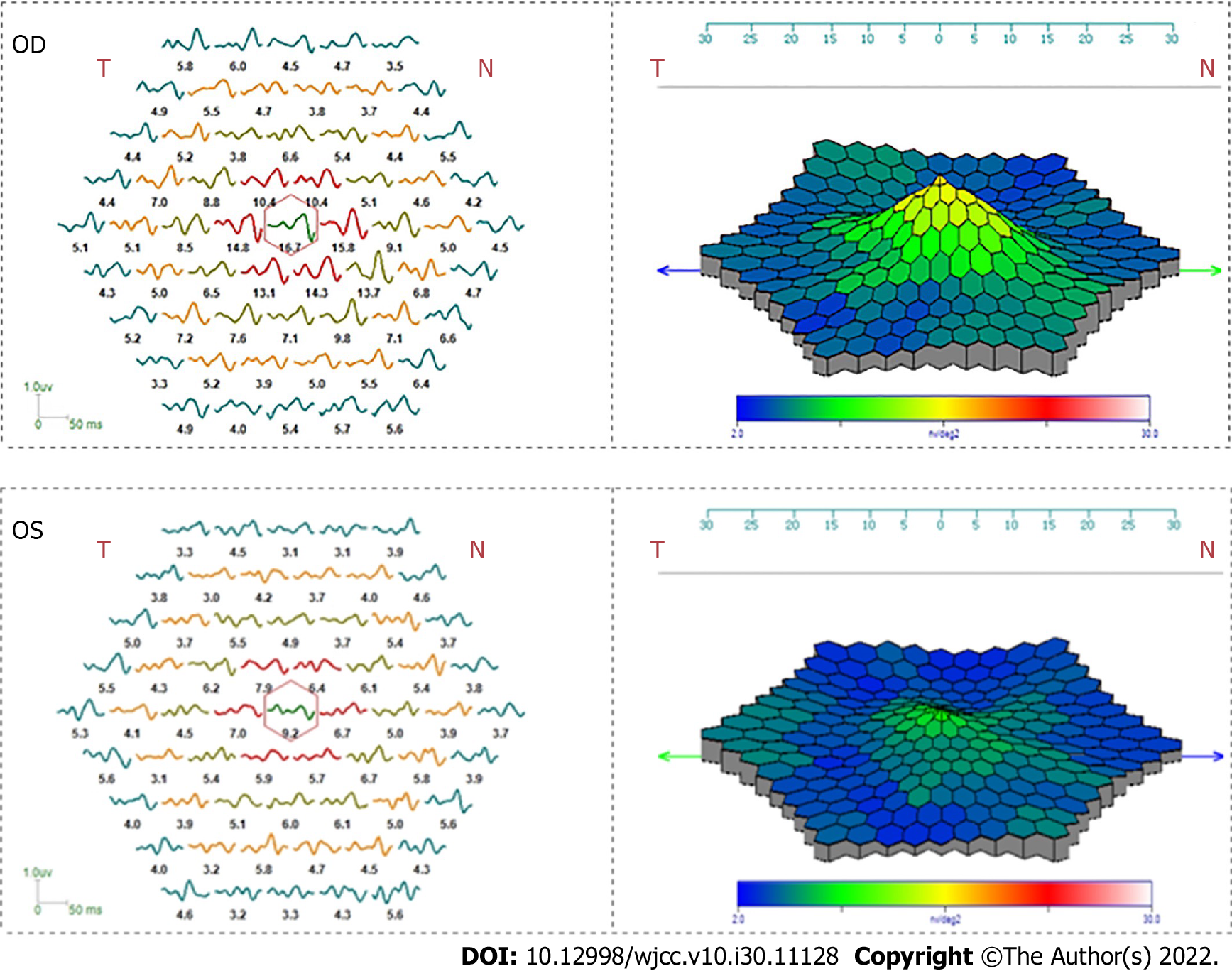
Patient 3: Funduscopic and auto-fluorescence examination of left eye revealed a blurred margin macular abnormality (Figure 5A and B). OCT discovered that the macular of left eye became more thinner, and the retinal pigment epithelium did not change significantly compared with right eye (Figure 5C). The visual electrophysiology indicated that the P100 amplitude of PVEP reduced in the left eye, while the function of ffERG cone cell system and the amplitude density of mfERG macular center decreased (Figure 6).
We made a diagnosis of old retinal injury induced by laser.
We made a diagnosis of acute retinal injury induced by strong-energy light irradiation.
We made a diagnosis of chronic retinal injury induced by sustaining light irradiation.
We suggested to stop the treatment of amblyopia.
For patients with CNV, we made anti VEGF treatment, at present vision improved with right eye vision 0.5.
This patient need no further treatment and we suggest to make a safety goggles when working.
When retina is irradiated by light under normal physiological conditions, part of the photon energy is absorbed by the photoreceptor cells. Moreover, the rest of extra photons are absorbed by the retinal pigment epithelium or choroid to avoid heat accumulation[11,12]. However, due to the direct effect of light energy, photoreceptor cells and RPE are also the most vulnerable tissues when the light irradiates abnormally[13]. Moreover, animal study found müller glia cell activation paticipated in a laser-induced retinal degeneration and regeneration in zebrafish[14]. During COVID-19 pandemic, researchers found retinas damages could be related with Neuropilin-1[15]. At present, studies have indicated that various types of light stimulation, such as ultraviolet, blue light and laser could damage the retina through photochemical reaction, photothermal effect and photomechanical effect[16-18]. As its biological effects can be accumulated, retinal injury can be caused by multiple irradiations, which can display the characteristic that the boundary of the damage area is clear in the early stage and fuzzy in the later stage[19]. In the cases, we observed three typical patients suffering from light-induced retinopathy.
In the first case, this young female patient received amblyopia treatment for one year and didn’t improve vision acuity. When retina related morphological and functional examinations were applied, we realized that this could be old laser-induced retina damage. Then the patients bring to mind that she was exposed to laser pen irradiation when played with classmates. Her left eye was found obvious pigmented scar in the macular region, which may be related to the proliferation and repair of peripheral RPE[20]. Angiography revealed that there were obvious round fluorescent defects at the corresponding lesion area of retina, which may be due to laser induced occlusion of retinal and choroidal vessels in macula, and then fluorescence perfusion defect. OCT showed that the outer nuclear layer of macular area was destroyed, resulting in the corresponding retinal layer continuity was disrupted. Consistent with the morphological results, electrophysiological results showed that the function of macula was significantly impaired, and the peripheral retina was not significantly abnormal.
In the second case, the soldier’s right eye vision acuity decreased after being exposed to instantaneous strong LED light. Because the high-energy visible light in the LED lamp is mainly blue light, fundus color and AF showed there was disorder of pigment in RPE of macular. The electrophysiological results indicated that there was no obvious abnormality in the peripheral retina of right eye, but the retinal function in the macular area was significantly damaged and the conduction function of optic nerve may be also affected to some extent.
In the third case, the patient is a middle-aged man who has been engaged in optical fiber work for a long time, mainly exposed to ultraviolet and blue light. Due to improper daily protective measures, visual acuity was obviously injured. Fundus examination showed that the patient’s macular in retina became thinner, which may be caused by the shortening of outer segment of photoreceptor or the detachment and disappearance of photoreceptor under long-term light stimulation resulting in thinning of the outer nuclear layer. In addition, RPE also showed atrophy and thinning after light injury. Similar to the previous two patients, this patient’s electrophysiological examination indicated that there is significant impairment of macular function.
Through the three cases, it can be found that the above three patients have a clear history of light damage. No matter what kind of light source equipment they experience, the macular of patients presents different forms of pathological lesion, especially in the outer nuclear layer where photoreceptor and RPE are located. In our cases, we found that retinopathy caused by light damage has similar morphological and functional characteristics. Specifically, the morphological changes were mainly pathological changes related to retinal pigment epithelium and photoreceptor, and the physiological function changes were largely associated with the decline of macular function. In terms of electrophysiological function, visual electrophysiology could easily assess majority light-induced macular injuries, including old cumulative asymptomatic damages, acute symptomatic damages and chronic occupational exposure.
We identified children, military personnel and optical fiber communicators are likely to suffer from retinal damage caused by light. Commonly, children are often misdiagnosed as amblyopia. The degree of lesions is related to the energy and duration of light irradiation, and is often manifested as macular thinning, interruption of RPE continuity, CNV and other manifestations. The amplitude changes of PVEP are common in acute high-energy injuries, and ffERG usually is normal. For long-term low energy sustained injury, PVEP amplitude is decreased and ffERG cone system is decreased, too. No matter what kind of light damage, the amplitude density of mfERG in macular center is decreased.
We thank each author who contributed to this paper.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Arabey AA, Egypt; Kotelevets SM, Russia S-Editor: Chen YL L-Editor: A P-Editor: Zhang XD
| 1. | Hunter JJ, Morgan JI, Merigan WH, Sliney DH, Sparrow JR, Williams DR. The susceptibility of the retina to photochemical damage from visible light. Prog Retin Eye Res. 2012;31:28-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 238] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 2. | Chen Y, Perusek L, Maeda A. Autophagy in light-induced retinal damage. Exp Eye Res. 2016;144:64-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Rossi F, Pini R, Menabuoni L, Mencucci R, Menchini U, Ambrosini S, Vannelli G. Experimental study on the healing process following laser welding of the cornea. J Biomed Opt. 2005;10:024004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Ivanov IV, Mappes T, Schaupp P, Lappe C, Wahl S. Ultraviolet radiation oxidative stress affects eye health. J Biophotonics. 2018;11:e201700377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 5. | Löfgren S. Solar ultraviolet radiation cataract. Exp Eye Res. 2017;156:112-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Moon J, Yun J, Yoon YD, Park SI, Seo YJ, Park WS, Chu HY, Park KH, Lee MY, Lee CW, Oh SJ, Kwak YS, Jang YP, Kang JS. Blue light effect on retinal pigment epithelial cells by display devices. Integr Biol (Camb). 2017;9:436-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | van Norren D, Vos JJ. Light damage to the retina: an historical approach. Eye (Lond). 2016;30:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Algvere PV, Marshall J, Seregard S. Age-related maculopathy and the impact of blue light hazard. Acta Ophthalmol Scand. 2006;84:4-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 219] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 9. | Turaka K, Bryan JS, Gordon AJ, Reddy R, Kwong HM Jr, Sell CH. Laser pointer induced macular damage: case report and mini review. Int Ophthalmol. 2012;32:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Petrou P, Kanakis M, Koutsandrea C, Georgalas I, Banerjee PJ. Full-Thickness Macular Hole Secondary to High-Power Handheld Blue Laser: Natural History and Management Outcomes. Am J Ophthalmol. 2015;160:1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Schweitzer D, Guenther S, Scibor M, Hammer M. Spectrometric investigations in ocular hypertension and early stages of primary open angle glaucoma and of low tension glaucoma--multisubstance analysis. Int Ophthalmol. 1992;16:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Palczewski K, Kiser PD. Shedding new light on the generation of the visual chromophore. Proc Natl Acad Sci U S A. 2020;117:19629-19638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 13. | Bai S, Sheline CR, Zhou Y, Sheline CT. A reduced zinc diet or zinc transporter 3 knockout attenuate light induced zinc accumulation and retinal degeneration. Exp Eye Res. 2013;108:59-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Conedera FM, Arendt P, Trepp C, Tschopp M, Enzmann V. Müller Glia Cell Activation in a Laser-induced Retinal Degeneration and Regeneration Model in Zebrafish. J Vis Exp. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | El-Arabey AA, Abdalla M. Neuropilin-1 may be responsible for retinal findings in patients with COVID-19. Hum Cell. 2021;34:1280-1281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Yu ZL, Qiu S, Chen XC, Dai ZH, Huang YC, Li YN, Cai RH, Lei HT, Gu HY. Neuroglobin - a potential biological marker of retinal damage induced by LED light. Neuroscience. 2014;270:158-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Yanagi Y. [Retinal phototoxicity from endoilluminators for vitrectomy]. Nippon Ganka Gakkai Zasshi. 2008;112:975-983. [PubMed] |
| 18. | Lavinsky D, Sramek C, Wang J, Huie P, Dalal R, Mandel Y, Palanker D. Subvisible retinal laser therapy: titration algorithm and tissue response. Retina. 2014;34:87-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Besharse JC, McMahon DG. The Retina and Other Light-sensitive Ocular Clocks. J Biol Rhythms. 2016;31:223-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Schuele G, Rumohr M, Huettmann G, Brinkmann R. RPE damage thresholds and mechanisms for laser exposure in the microsecond-to-millisecond time regimen. Invest Ophthalmol Vis Sci. 2005;46:714-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |