Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11122
Peer-review started: June 9, 2022
First decision: June 27, 2022
Revised: July 7, 2022
Accepted: September 16, 2022
Article in press: September 16, 2022
Published online: October 26, 2022
Processing time: 133 Days and 22.6 Hours
It is necessary for clinicians to be aware of a rare but possible acute respiratory distress syndrome (ARDS) complication caused by multiple wasp stings. Severe ARDS has a high mortality rate but no specific pharmacotherapies have been identified to date. This case study presents the first case of severe ARDS caused by multiple wasp stings, treated successfully with extracorporeal membrane oxy
A 24-year-old woman was admitted to the emergency department after being stung by more than 10 wasps within a 30-min period, with clinical symptoms of multiple rashes, dizziness, chest tightness, nausea, and vomiting. On the 2nd day of admission, the patient developed progressive dyspnea. The patient was diagnosed with ARDS based on clinical manifestations and lung computed tomography (CT) scan. Because of the progressive dyspnea, the intensive care unit physician performed endotracheal intubation and continued to provide ventilator support, but the patient’s respiratory distress worsened, as indicated by the ratio of arterial partial pressure of oxygen to fraction of inspired oxygen. Veno-venous ECMO was initiated for 6 d. On day 7 of admission, ECMO was stopped. On the 11th day of admission, CT scan of the lungs revealed significant reduction of ground-glass opacities and consolidations. After about 2 wk, the patient recovered completely from ARDS and was discharged to home. At the 2-mo follow-up, the patient was in good health with no recurrence of dyspnea nor chest tightness.
ARDS complication caused by multiple wasp stings may be fatal when mechanical ventilation becomes dangerous due to persistent hypoxemia and despite optimization of ARDS management. We propose that the early implementation of ECMO is a relatively effective treatment, although the evidence is relatively limited.
Core Tip: It is necessary for clinicians to be aware of a rare but possible acute respiratory distress syndrome (ARDS) complication caused by multiple wasp stings. To date, there is no evidence of the extracorporeal membrane oxygenation (ECMO) treatment for ARDS or respiratory failure caused by wasp stings. For the first time, we report a case of severe ARDS caused by multiple wasp stings, successfully treated with ECMO.
- Citation: Cai ZY, Xu BP, Zhang WH, Peng HW, Xu Q, Yu HB, Chu QG, Zhou SS. Acute respiratory distress syndrome following multiple wasp stings treated with extracorporeal membrane oxygenation: A case report. World J Clin Cases 2022; 10(30): 11122-11127
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11122.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11122
Although involvement of the respiratory system is a common clinical manifestation of multiple wasp stings, rapid progression to severe acute respiratory distress syndrome (ARDS) is rare. Severe ARDS has a high mortality rate; however, to date, no specific pharmacotherapies have been identified and treatment is focused on lung-protective ventilation[1]. Extracorporeal membrane oxygenation (ECMO) is a treatment in which blood is circulated outside the body to be oxygenated on a gas-permeable membrane. It has been shown to improve survival rates and outcomes in patients with severe ARDS in critical care settings[2,3], particularly in patients who have severe ARDS within the 1st week of mechanical ventilation and do not have multiple organ failure[4,5]. However, ECMO is also an invasive, costly and high-risk treatment, with complications such as thrombocytopenia and bleeding[6].
There is no evidence in the literature of the ECMO treatment of ARDS nor respiratory failure caused by wasp stings. This case study presents the first case of severe ARDS caused by multiple wasp stings, treated successfully with ECMO. It also emphasizes the effectiveness of early ECMO treatment of severe ARDS with persistent hypoxemia.
A 24-year-old woman was admitted to the emergency department (ED) after being stung by more than 10 wasps within a 30-min period.
After being stung, the patient had clinical symptoms of multiple rashes, dizziness, chest tightness, nausea, and vomiting. She was conscious and no other abnormalities were found.
The patient had no known or documented allergies.
The patient’s personal and family history was unremarkable.
On clinical examination, the patient had a pulse of 120 beats/min, blood pressure of 84/56 mmHg (1 mmHg = 0.133 kPa), respiratory rate of 25 breaths/min, and pulse oximetry of 98% in room air. She had no cardiac murmurs or wet rales. Other than rash and erythema on her neck, chest and upper extremities, no other abnormalities were found on systemic examination.
The patient's biological tests (including blood routine, markers of coagulation, liver and kidney functions, myocardial enzyme spectrum, and electrolytes) were normal.
The electrocardiogram revealed sinus tachycardia, without any signs of ischemia. Computed tomography (CT) scan of the lung revealed no abnormalities.
Anaphylactic shock caused by severe bee stings.
The stingers were removed first, and the treatment then begun with adrenaline [0.5 mg intramuscular (IM)], methylprednisolone [80 mg intravenous (IV)], promethazine (25 mg IM), and omeprazole (40 mg IV). Three hours after admission, the patient's condition began to deteriorate and the chest tightness and pain worsened. Arterial blood gas analysis showed pH 7.36, partial pressure of oxygen (PaO2) 50 mmHg (on 40% fraction inspired oxygen), partial pressure of carbon dixoide (PaCO2) 40.2 mmHg, and bicarbonate 22.7 mmol/L. She was admitted to the intensive care unit (ICU), and noninvasive mechanical ventilation was started. IV adrenaline [0.5 mg/every 4 h (q4h)], promethazine (25 mg/d), and dexamethasone (10 mg/q12h) were administered, and continuous hydration infusions and other symptomatic treatment were also given.
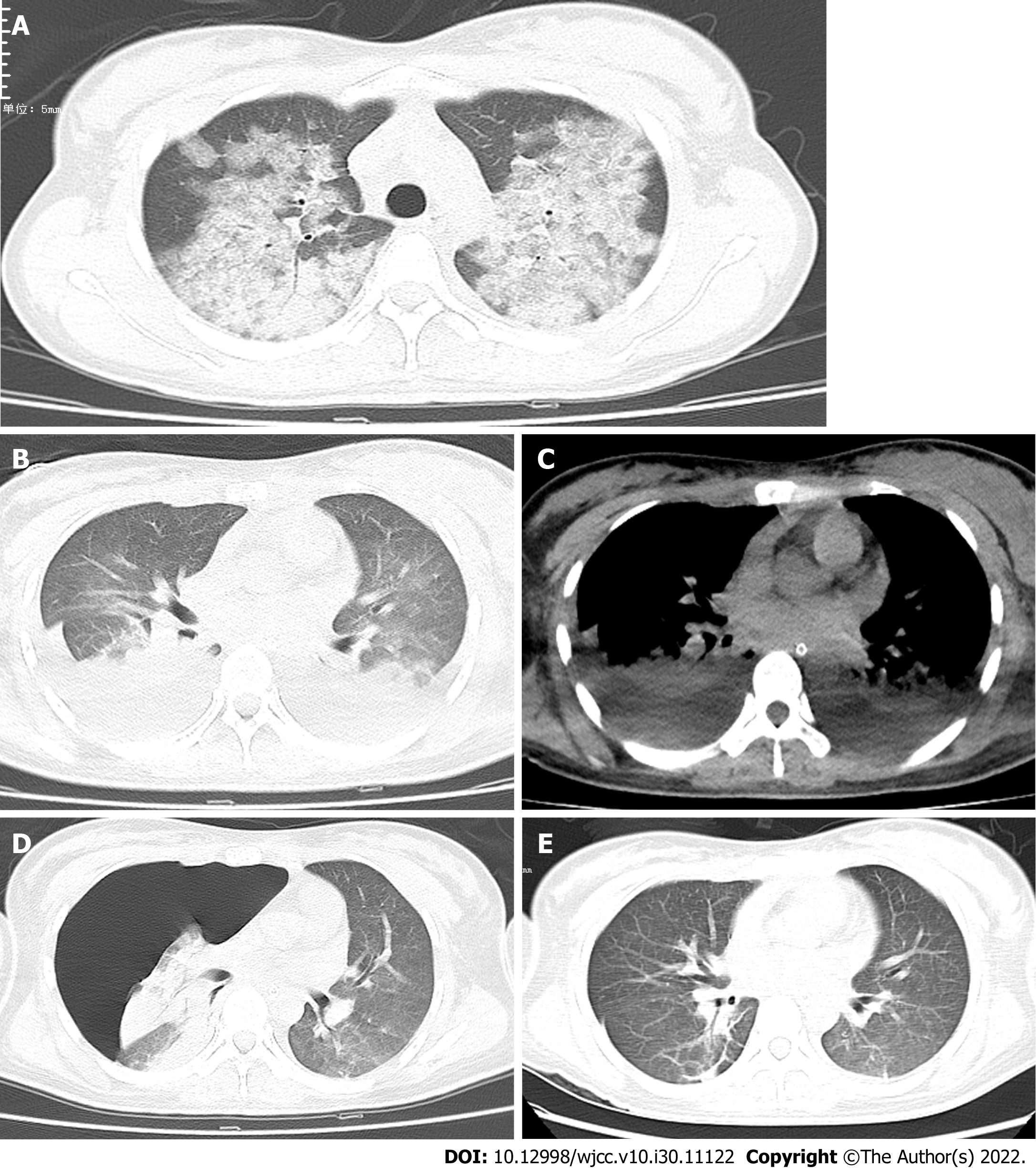
On the second day of admission, the patient developed progressive dyspnea. CT scan of the lung (Figure 1A) revealed a small pleural effusion and bilateral lung multifocal ground-glass opacity. The ICU physician performed endotracheal intubation and continued to provide ventilator support. Subsequently, fiberoptic bronchoscopy examination revealed tracheal mucosal edema and congestion with foamy sputum in the main bronchial lumens but no obvious bleeding. Six hours after tracheal intubation, the patient’s respiratory distress worsened, with PaO2/FiO2 ratio of 39. Physicians decided to place the patient on veno-venous ECMO for 6 d. ECMO support was initiated with a blood flow of 3.0 L/min and a purge gas flow rate of 3 L/min. Ventilatory settings were adjusted to volume-controlled ventilation of 6 mL/kg ideal body weight, positive end-expiratory pressure of 8 cmH2O, peak inspiratory pressure of 40 cmH2O, respiratory rate of 20, and fraction of inspired oxygen of 100%. With minimal mechanical ventilation, the patient achieved stability, with a pulse rate of 84 beats per min and pulse blood oxygen saturation of 98%.
On the 7th day, ECMO was stopped, and the patient felt well and was clinically stable. CT scan of the lungs (Figure 1B and C) revealed large multiple patchy ground-glass opacities with consolidation, and a possible large pleural effusion in both lungs. As a result, the patient underwent closed thoracic drainage of hydrothorax. On the 11th day, CT scan of the lungs (Figure 1D) revealed significant reduction of ground-glass opacities and consolidations. However, the patient developed right pneumothorax with lung compression greater than 50%, necessitating treatment of the right lung with closed thoracic pneumothorax drainage.
On the 14th day, chest CT (Figure 1E) revealed that the pneumothorax had disappeared, and the patient was discharged to home. At the 2-mo follow-up visit, the patient was in good health, with no recurrence of dyspnea nor chest tightness.
In China’s vast hilly areas, wasp stings are one of the most common emergencies in the emergency departments of hospitals. They are also one of the environmental accidents that seriously threaten human health. Some patients with wasp stings present with local hypersensitivity; however, a small number of patients develop multisystem involvement due to multiple stings[7]. The clinical manifestations of wasp stings differ, depending on the victim’s sensitivity to the venom and the number of stings received[8]. Symptoms associated with wasp sting range from simple papular urticaria and subcutaneous angioedema to skin necrosis, throat edema, severe anaphylaxis shock, and multiple organ dysfunction involving the kidney, heart, central nervous system, liver, respiratory system, and coagulopathy, all of which can be fatal[7,9]. It is critical to completely assess the patient’s condition, including the number of wasp stings, severity of the allergic reaction, any associated multiple system damage, and the need for cardiopulmonary resuscitation. Epinephrine is the medication of choice for the initial treatment of anaphylaxis following multiple wasp stings, and if administered promptly, can be lifesaving.
The pathogenesis of ARDS after wasp stings is poorly understood. Wasp venom is a well-known natural complex toxic mixture of polypeptides, enzymes, histamine, hyaluronic acid, and phospholipase A2[10]. Melittin, the main lethal component of wasp venom, affects membrane integrity[11]. In conjunction with melittin, the higher molecular weight enzyme phospholipase A2 acts as a cytolytic agent, causing tissue damage such as intravascular hemolysis, rhabdomyolysis, and acute lung injury[10]. Wasp venom can initiate a series of immune responses and even severe envenomation syndrome in the human body, resulting in the massive release of various cytokines and acute inflammatory storm[10]. These inflammatory factors can cause tissue and organ damage, including the respiratory system[12], leading to ARDS in severe cases[13]. Wasp venom is a complex neuromuscular blocking agent, and its active substance can affect acetylcholine synthesis and release. It has a direct toxic effect on the membrane voltage of the striated muscle sodium ion channel, which can cause respiratory muscle paralysis and respiratory failure[11,13].
Despite some improvements, mortality from ARDS, particularly severe ARDS, remains a severe threat[1]. To date, no specific pharmacotherapies have been identified, and treatment is focused on lung-protective ventilation[1]. Physicians should strongly consider ventilation in a prone position when persistent hypoxemia cannot be relieved in ARDS patients with a PaO2/FiO2 ratio of < 150. It is also effective in patients with acute hypoxic respiratory failure without intubation[6]. Despite optimized standard therapies such as neuromuscular blockade with deep sedation and prone positioning for the previous 24 h, some patients continue to deteriorate clinically. ECMO is a treatment in which blood is circulated outside the body to be oxygenated on a gas-permeable membrane. It has been shown to improve survival rates and outcomes in patients with severe ARDS in critical care settings[2,3], particularly in patients who have severe ARDS within the 1st week of mechanical ventilation and do not have multiple organ failure[4,5].
There is no evidence in the literature of treatment of ARDS nor respiratory failure caused by wasp stings with ECMO. In the present case, despite receiving mechanical ventilation and other optimized standard therapies at an early stage, the patient’s respiratory status continued to rapidly deteriorate. ECMO treatment was started after she passed a comprehensive health assessment, and rapid improvement in the patient’s condition was observed. Thus, when mechanical ventilation becomes dangerous for patients with ARDS following multiple wasp stings due to persistent hypoxemia and despite optimization of ARDS management, we propose that the early implementation of ECMO is a relatively effective treatment, although the evidence is relatively limited[14,15].
Patients with multiple wasp stings need early assessment and treatment by emergency care physicians to reduce subsequent organ dysfunction, in order to shorten the disease course and improve the prognosis. Rapid progression to severe ARDS after wasp stings is rare, and severe ARDS has a high mortality rate. When mechanical ventilation becomes dangerous in patients with ARDS following multiple wasp stings due to persistent hypoxemia and despite optimization of ARDS management for the previous 24 h, we propose that the early implementation of ECMO is a relatively effective treatment, although the evidence is relatively limited.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Oliveira I, Brazil; Sunder T, India S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Paolone S. Extracorporeal Membrane Oxygenation (ECMO) for Lung Injury in Severe Acute Respiratory Distress Syndrome (ARDS): Review of the Literature. Clin Nurs Res. 2017;26:747-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, Dechartres A, Elbourne D. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048-2057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 244] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 4. | Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Brodie D, Mercat A; EOLIA Trial Group, REVA, and ECMONet. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2018;378:1965-1975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1417] [Cited by in RCA: 1485] [Article Influence: 212.1] [Reference Citation Analysis (0)] |
| 5. | Combes A, Brodie D, Bartlett R, Brochard L, Brower R, Conrad S, De Backer D, Fan E, Ferguson N, Fortenberry J, Fraser J, Gattinoni L, Lynch W, MacLaren G, Mercat A, Mueller T, Ogino M, Peek G, Pellegrino V, Pesenti A, Ranieri M, Slutsky A, Vuylsteke A; International ECMO Network (ECMONet). Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. 2014;190:488-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 348] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 6. | Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, Forel JM, Guérin C, Jaber S, Mekontso-Dessap A, Mercat A, Richard JC, Roux D, Vieillard-Baron A, Faure H. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 292] [Cited by in RCA: 466] [Article Influence: 77.7] [Reference Citation Analysis (0)] |
| 7. | Singh H, Chaudhary D, Dhibar DP. Rhabdomyolysis and acute kidney injury following multiple wasp stings. QJM. 2021;114:53-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Vikrant S, Parashar A. Two Cases of Acute Kidney Injury Due to Multiple Wasp Stings. Wilderness Environ Med. 2017;28:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Radhakrishnan H. Acute kidney injury and rhabdomyolysis due to multiple wasp stings. Indian J Crit Care Med. 2014;18:470-472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Ferreira RS Jr, Almeida RA, Barraviera SR, Barraviera B. Historical perspective and human consequences of Africanized bee stings in the Americas. J Toxicol Environ Health B Crit Rev. 2012;15:97-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Silva GBD Junior, Vasconcelos AG Junior, Rocha AMT, Vasconcelos VR, Barros J Neto, Fujishima JS, Ferreira NB, Barros EJG, Daher EF. Acute kidney injury complicating bee stings - a review. Rev Inst Med Trop Sao Paulo. 2017;59:e25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Mendonça-da-Silva I, Monteiro WM, Sachett JAG, Barbosa ES, Cordeiro-Dos-Santos M, Lacerda MVG, Melo GC, Costa AG, Val FFA. Bee sting envenomation severe cases in Manaus, Brazilian Amazon: clinical characteristics and immune markers of case reports. Rev Soc Bras Med Trop. 2020;54:e20200319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Walker T, Tidwell AS, Rozanski EA, DeLaforcade A, Hoffman AM. Imaging diagnosis: acute lung injury following massive bee envenomation in a dog. Vet Radiol Ultrasound. 2005;46:300-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome. Lancet. 2021;398:622-637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 529] [Cited by in RCA: 678] [Article Influence: 169.5] [Reference Citation Analysis (0)] |
| 15. | Laffey JG, Misak C, Kavanagh BP. Acute respiratory distress syndrome. BMJ. 2017;359:j5055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |