Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11116
Peer-review started: June 17, 2022
First decision: August 1, 2022
Revised: August 17, 2022
Accepted: September 7, 2022
Article in press: September 7, 2022
Published online: October 26, 2022
Processing time: 125 Days and 21.7 Hours
There has been an increasing number of elderly patients with intraductal papillary mucinous neoplasm (IPMN), who are surgically intolerant and require less invasive treatment options, which are limited. In the present study, we report a case of IPMN presenting with acute recurrent pancreatitis (ARP), in which radiation therapy effectively prevented further attacks of ARP and reduced tumor volume.
An 83-year-old man was referred to our hospital with an asymptomatic incidental pancreatic cyst. Endoscopic ultrasound imaging and magnetic resonance cholangiopancreatography revealed a multiloculated tumor in the head of the pancreas, with dilated pancreatic ducts and mural nodules. The patient was diagnosed with mixed-type IPMN, and five years later, he developed ARP. Several endoscopic pancreatic ductal balloon dilatations failed to prevent further ARP attacks. Surgery was considered clinically inappropriate because of his old age and comorbidities. He was referred to our department for radiation therapy targeted at those lesions causing intraductal hypertension and radiation was administered at a dose of 50 Gy. An magnetic resonance imaging scan taken ten weeks after treatment revealed a decrease in tumor size and improvement of pancreatic duct dilatation. Fourteen months later, he remains symptom-free from ARP.
This case highlights the important role of radiation therapy in mitigating the signs and symptoms of ARP in patients with inoperable IPMN.
Core Tip: For intraductal papillary mucinous neoplasm (IPMN) patients with symptoms of acute recurrent pancreatitis (ARP), the only therapeutic option recommended by current guidelines is surgical intervention. However, a growing number of IPMN patients require minimally invasive treatment options because of old age, systemic conditions, or personal preference. Herein, we present a case of IPMN presenting with ARP, in which radiation therapy effectively prevented further attacks of ARP and reduced tumor volume. This case highlights the important role of radiation therapy in preventing further episodes of ARP in patients with IPMN who cannot undergo surgery.
- Citation: Harigai A, Kume K, Takahashi N, Omata S, Umezawa R, Jingu K, Masamune A. Favorable response after radiation therapy for intraductal papillary mucinous neoplasms manifesting as acute recurrent pancreatitis: A case report. World J Clin Cases 2022; 10(30): 11116-11121
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11116.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11116
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is a cystic lesion in which mucin-producing neoplastic epithelia proliferate abnormally. IPMN is benign, but is known to have malignant potential and requires regular surveillance; surgical resection is recommended for lesions at a high risk of malignancy. High-resolution imaging technology is being increasingly used to diagnose IPMN before it manifests any signs or symptoms[1]. Most patients with IPMN are asymptomatic until malignant transformation and are eventually diagnosed with intraductal papillary mucinous cancer, which has a poor prognosis. Therefore, current efforts are focused on identifying and treating IPMNs that are at a high risk of malignancy.
Recent studies have reported that some IPMNs present with acute pancreatitis (AP) or acute recurrent pancreatitis (ARP) associated with intraductal hypertension[2]. The prevention of repetitive attacks of ARP is preferred because ARP reduces the patients’ quality of life and may lead to irreversible chronic pancreatitis[3]. The latest guidelines state that patients with IPMN and accompanying AP may undergo surgical resection for symptomatic relief[4]. However, there has been inadequate discussion regarding other treatment options when surgery is not clinically appropriate. Here, we report a case of IPMN with ARP in which radiation therapy successfully prevented further attacks of ARP and reduced the tumor volume.
An 83-year-old man diagnosed with IPMN was referred to our radiation oncology department because of repetitive episodes of ARP resistant to endoscopic treatment.
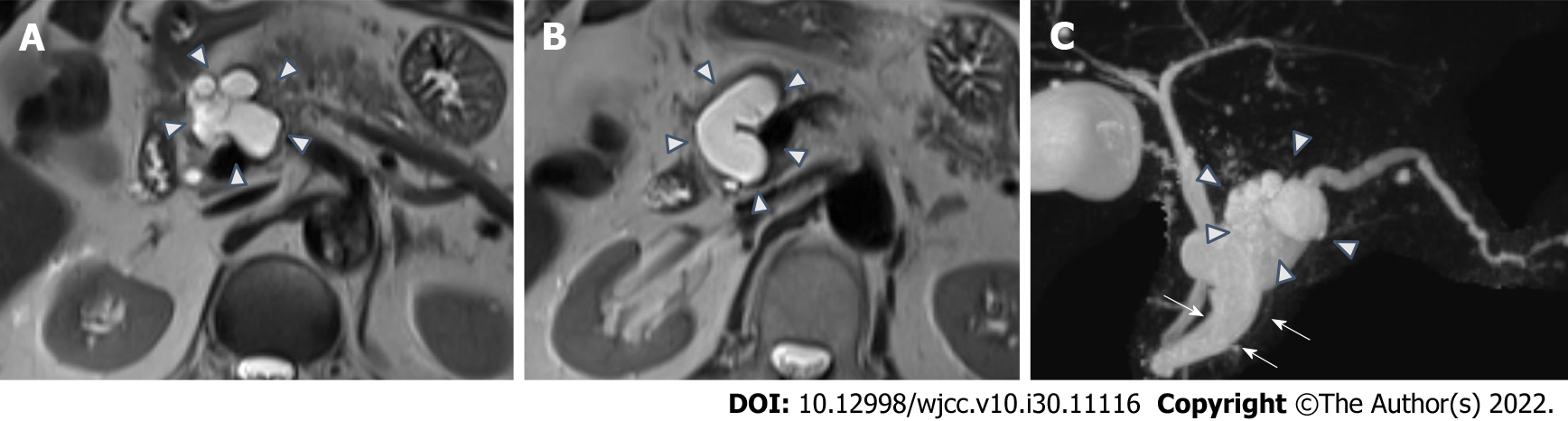
The patient visited a physician to investigate an incidentally detected asymptomatic pancreatic cyst, and was subsequently referred to our hospital for suspected IPMN. Endoscopic ultrasound (EUS) imaging and magnetic resonance cholangiopancreatography (MRCP) revealed a 30 mm multiloculated tumor, located in the head of the pancreas; the main duct had a diameter of 10 mm and the mural nodules were 8 mm in height. The patient was diagnosed with mixed-type IPMN (Figure 1).
The patient was regularly monitored for four years using imaging for signs of malignancy. During regular outpatient surveillance, gradual dilation of the main pancreatic duct to 13 mm was observed, which met the “high-risk stigmata” criteria for surgical resection, as per IPMN management guidelines[4-6]. The patient’s old age and personal preference were indicative of conservative management with follow-up and not surgical intervention. Five years after the initial diagnosis, he developed mild AP twice, but recovered with supportive measures. However, the following year, he developed ARP once a month for three consecutive months. Several attempts at endoscopic pancreatic ductal balloon dilatation failed to prevent the recurrence of AP, and pancreatic juice samples obtained by these endoscopic procedures did not show cytological malignancy. Although international IPMN guidelines suggest surgery for symptomatic relief in pancreatitis[4], the surgeons who consulted with this patient concluded that pancreaticoduodenectomy would not be clinically appropriate because of his old age and comorbidities. Because the episodes of ARP in this case were mainly attributed to intraductal hypertension caused by viscous mucin-rich pancreatic juice secreted from IPMN, the patient was referred to our department for radiation therapy to reduce mucin secretion and prevent further episodes of AP.
The patient had a medical history of right lacunar infarction with residual hemiparesis, prostate cancer, colorectal polyps, nephrotic syndrome, chronic pulmonary obstructive disease, and hemorrhoids.
He had smoked 60 cigarettes per day for 55 years, from 22 to 77 years of age.
On presentation to our outpatient clinic, the patient had no abnormal pathological signs or symptoms, including jaundice.
At our radiation oncology department, laboratory tests indicated that complete blood count, C-reactive protein, liver enzymes, and pancreatic enzymes, were within the normal range.
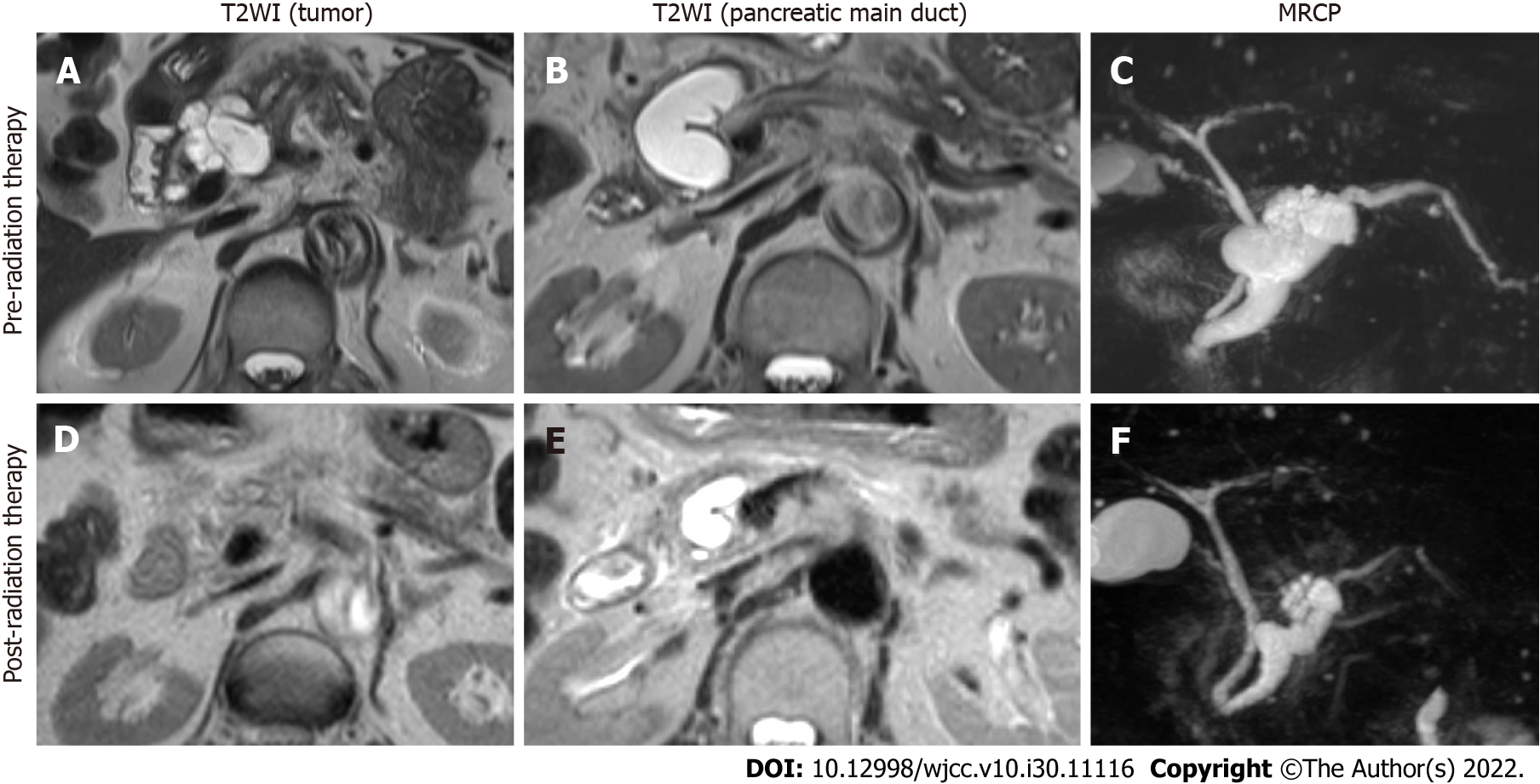
One month before initiating radiation therapy, MRCP revealed a 36.5 mm multiloculated tumor in the head of the pancreas and significant pancreatic main duct dilatation (17 mm in diameter). The common bile duct was not dilated (Figure 2).
The final diagnosis in the current case was IPMN leading to episodes of ARP, which was not indicated for surgery due to the patient’s age and comorbidities.
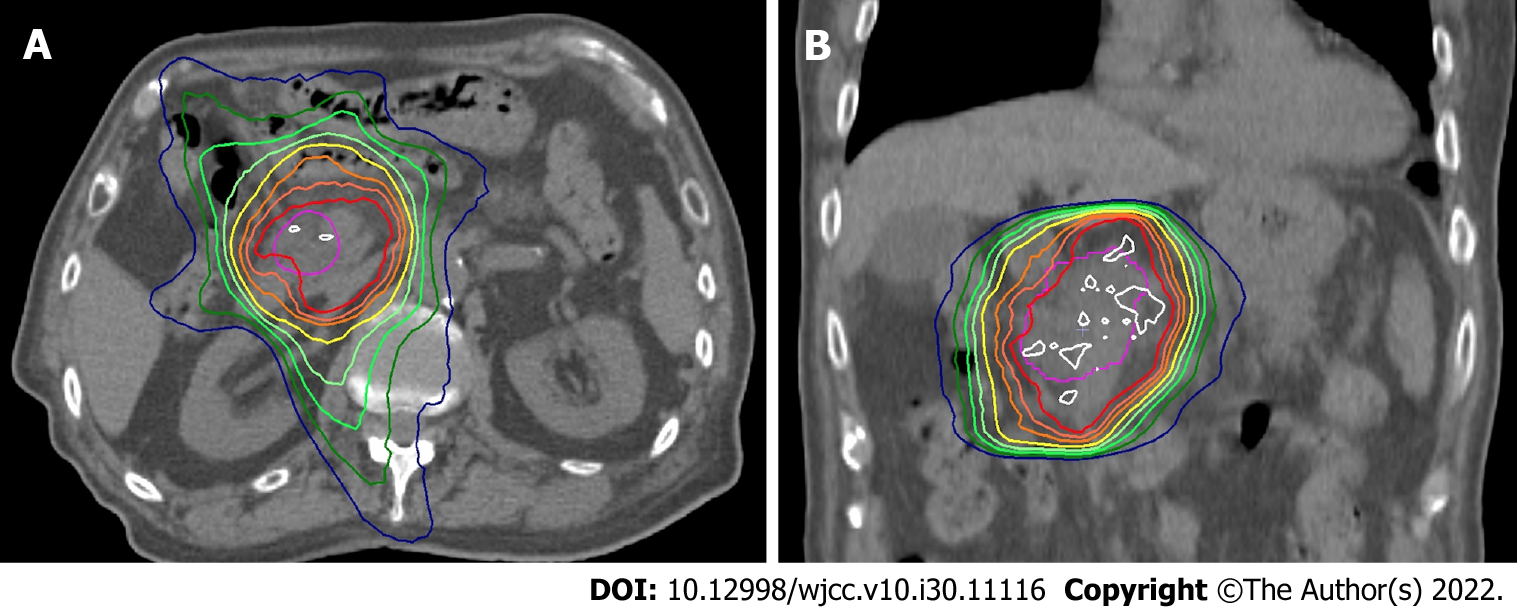
The patient was treated with radiation therapy at a total dose of 50 Gy in 25 fractions for 5 wk. Radiation therapy was delivered using 10 MV photon beams from a linear accelerator equipped with a multileaf collimator. Volumetric modulated arc therapy was performed to reduce acute gastrointestinal toxicity (Figure 3). The gross target volume (GTV) was defined as the IPMN lesion, and the clinical target volume (CTV) was defined as equal to the GTV. The internal target volume for GTV was contoured with reference to the respiratory movement, using four-dimensional computed tomography. The planning target volume (PTV) was defined as the CTV plus a 5 mm margin. The prescribed dose was calculated to cover 95% of the PTV.
During radiation therapy, the patient reported symptoms of acute radiation toxicity such as fatigue, nausea, radiation dermatitis, and diarrhea, all of which corresponded to grades 1 and 2 of the Common Terminology Criteria for Adverse Events[7]. The patient recovered completely within six weeks after radiation therapy. Magnetic resonance imaging performed ten weeks after the initiation of radiation therapy revealed a decrease in tumor size from 36 mm to 28 mm and an improvement in pancreatic duct dilatation (Figure 2). The patient had not experienced any symptoms indicating a recurrence of AP until his last follow-up, 14 mo after the administration of radiation therapy.
To the best of our knowledge, this report presents the first case in which radiation therapy was successfully administered to a patient with repetitive episodes of ARP caused by IPMN. The patient did not report any abdominal symptoms indicative of pancreatitis for at least one year after the completion of radiation therapy. Although chemoradiotherapy has recently been recognized as an adjuvant therapy, performed after surgical resection in patients with IPMN[8], little is known about the role of radiation therapy in unresected IPMN. Kameyama et al[9] reported the case of a patient with unresectable IPMNs with suspected involvement of the superior mesenteric artery, in which chemoradiotherapy successfully shrunk the tumor prior to conversion surgery. However, there have been no reports of patients with IPMN receiving radiation therapy for symptomatic relief of ARP. Jang et al[2] reported that among 488 patients with IPMN, 34 (7%) developed AP or ARP attributable solely to IPMN. Thus, considering our aging society, our patient is a representative case of ARP caused by IPMN, for which minimally invasive therapeutic measures are preferred. We expect that the number of similar cases will increase in the near future.
Therapeutic measures for ARP attributable to IPMN have not yet been established. Only a short explanatory note on symptomatic IPMN is found at the bottom of the IPMN management algorithm in the international guidelines of IPMN, stating, “pancreatitis may be an indication for surgery for relief of symptoms”[5]. However, regardless of the type of procedure, pancreatic surgery can lead to severe complications including postoperative pancreatic fistula (POPF). POPF, which causes leakage of pancreatic juice, intraperitoneal abscesses, and lethal hemorrhage from pseudoaneurysms, has an incidence of > 10%. Patients who develop ARP due to IPMN can also be treated endoscopically, which unfortunately failed in the present case. Another previously reported treatment option for pancreatic cysts is the injection of ethanol and paclitaxel into the cystic lesion[10]. This EUS-guided technique is undoubtedly less invasive than surgery but could potentially lead to severe complications in patients with IPMN. Because IPMN cysts directly communicate with the main pancreatic duct, post-procedural AP may occur more frequently in IPMN than in other pancreatic cystic lesions[11].
Immediately after the patient was referred to our radiation oncology department, we developed this treatment strategy by hypothesizing that an appropriate dose of radiation therapy could have an effect on abnormal mucin secretion from IPMN. Although chemoradiotherapy might have a better tumor control[9], it was not selected considering the negative cytological malignancy of the pancreatic juice, age, and comorbidities of the patient. Research on adverse late effects of radiation therapy on the pancreas has shown that pancreatic exocrine insufficiency, which could result in malabsorption, occurs at 45 Gy[12]. Recently, there was a case report describing the application of chemoradiotherapy (50.4 Gy irradiation and gemcitabine) for invasive pancreatic IPMN[13]. We set the radiation dose for this patient based on previously reported experiences. We believe that this case will help establish radiation therapy as a novel nonsurgical treatment for patients with ARP caused by IPMN. Therefore, more such cases are essential to investigate the necessary and adequate radiation dose and to establish this treatment strategy.
This case showed the important role of radiation therapy in recurrent episodes of ARP in patients with IPMN, who cannot undergo surgical resection.
The authors thank the staff of the Department of Radiation Oncology at Tohoku University Hospital for their support in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beji H, Tunisia; Khalil MTASH, Egypt S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Klibansky DA, Reid-Lombardo KM, Gordon SR, Gardner TB. The clinical relevance of the increasing incidence of intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol. 2012;10:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 126] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Jang JW, Kim MH, Jeong SU, Kim J, Park DH, Lee SS, Seo DW, Lee SK, Kim JH. Clinical characteristics of intraductal papillary mucinous neoplasm manifesting as acute pancreatitis or acute recurrent pancreatitis. J Gastroenterol Hepatol. 2013;28:731-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Braganza JM, Lee SH, McCloy RF, McMahon MJ. Chronic pancreatitis. Lancet. 2011;377:1184-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 343] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 4. | Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 1147] [Article Influence: 143.4] [Reference Citation Analysis (1)] |
| 5. | Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K; International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1714] [Cited by in RCA: 1613] [Article Influence: 124.1] [Reference Citation Analysis (0)] |
| 6. | Tanaka M. International consensus on the management of intraductal papillary mucinous neoplasm of the pancreas. Ann Transl Med. 2015;3:286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 7. | U.S. Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. [cited 10 May 2022]. Available from: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. |
| 8. | McMillan MT, Lewis RS, Drebin JA, Teitelbaum UR, Lee MK, Roses RE, Fraker DL, Vollmer CM. The efficacy of adjuvant therapy for pancreatic invasive intraductal papillary mucinous neoplasm (IPMN). Cancer. 2016;122:521-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Kameyama S, Motonari H, Ishimine T, Isa T. Successful treatment with conversion surgery following chemoradiotherapy for unresectable invasive intraductal papillary mucinous neoplasm. Clin J Gastroenterol. 2020;13:579-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Seo DW. EUS-Guided Antitumor Therapy for Pancreatic Tumors. Gut Liver. 2010;4 Suppl 1:S76-S81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Choi JH, Lee SH, Choi YH, You MS, Shin BS, Paik WH, Ryu JK, Kim YT. Safety of endoscopic ultrasound-guided ethanol ablation for pancreatic cystic lesions: A single-center experience of 214 patients. Hepatobiliary Pancreat Dis Int. 2019;18:562-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Russo S, Ove R, Fajardo L, Tepper J. Adverse Late Effects of Radiation Treatment in the Pancreas. In: Rubin P, Constine L, Marks L. ALERT • Adverse Late Effects of Cancer Treatment. Medical Radiology. Heidelberg: Springer, 2014. |
| 13. | Ochiai T, Igari K, Furuyama T, Ito H, Mitsunori Y, Aihara A, Kumagai Y, Iida M, Odajima H, Tanaka S, Arii S, Yamazaki S. Favorable response after gemcitabine-radiotherapy for invasive pancreatic intraductal papillary mucinous neoplasm: a case report. Int Surg. 2013;98:340-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |