Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10803
Peer-review started: July 14, 2022
First decision: August 1, 2022
Revised: August 11, 2022
Accepted: September 1, 2022
Article in press: September 1, 2022
Published online: October 16, 2022
Processing time: 77 Days and 0.6 Hours
Scrotal lipoma is exceedingly rare, so its origin is still unknown. Injury is sug
A 66-years elderly male with giant scrotal mass. B-ultrasound, computed tomography and magnetic resonance imaging examinations are typical lipoma-like changes, which were confirmed by postoperative pathological analysis. Abnormal somatic fat distribution was confirmed by images. no recurrence after follow-up for 2 years. Previously published English-language literature was reviewed, and a history of inguinal or pelvic surgery was reported in 6 studies (total 21 cases). To our knowledge, this is the heaviest bilateral scrotal lipoma in the English-language literature, and it has the longest postoperative follow-up time. More importantly, the origin of these tumours is reviewed and discussed.
Giant bilateral scrotal lipoma in elderly may as part of the symptoms of abnormal somatic fat distribution.
Core Tip: A case of giant bilateral scrotal lipoma was reported, and the literature was reviewed. A 66-year-old male with a giant scrotal mass was evaluated. Surgical treatment was performed, and scrotal lipoma were confirmed by postoperative pathological analysis. This is the heaviest bilateral scrotal lipoma in the English-language literature, and it has the longest postoperative follow-up time. More importantly, the origin of these tumours is reviewed and discussed.
- Citation: Chen Y, Li XN, Yi XL, Tang Y. Giant bilateral scrotal lipoma with abnormal somatic fat distribution: A case report. World J Clin Cases 2022; 10(29): 10803-10810
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10803.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10803
In 1780, Pelletan described a fatty tumour of the cord[1]. In 1883, Roswell Park reported a case of intrascrotal lipoma and concurrently reviewed three reported cases[1,2]. Cecil[1] reported a case of intrascrotal lipoma in 1927.
Scrotal lipoma is exceedingly rare, so its origin is still unknown[2,3]. Injury is suggested as a potential factor, but the cause remains unclear. It is difficult to determine the origin of these tumours. Previous studies have suggested that these tumours may be congenital[4] or that they originate from small fatty particles around the cord. Other studies have suggested that these tumours originate from testicles or the tunica[2].
These tumours are very large. A 75-cm lipoma from the scrotum to the knee was reported by Kocher[1]. Regarding weight, Brossard reported a tumour that weighed 9 pounds, and Bonney reported a 20-pound fibrolipoma in 1930[2]. However, no pure lipoma was observed[1]. A study published in 1930 reported a giant scrotal lipoma weighing 480-1100 g[2,5]. Seidu et al[5] reported a large unilateral scrotal mass that weighed 1100 g in 2020.
Herein, a large bilateral scrotal lipoma with abnormal accumulation of body surface fat was reported. To our knowledge, this is the heaviest bilateral scrotal lipoma in the English-language literature, and it has the longest postoperative follow-up time. More importantly, the origin of these tumours is reviewed and discussed.
Progressive enlargement of bilateral scrotum for more than one year.
At first, the bilateral scrotal tumours were small (approximately the size of peanuts); then, they became larger. The patients reported slight itching, but no pain or other discomfort. Both sides of his scrotum were obviously enlarged, approximately 13 cm in diameter, and the skin of the scrotum was tight, with no redness or varicose veins.
The patient had undergone electroresection of the prostate and bladder lithotripsy for benign prostatic hyperplasia three years ago in our clinic.
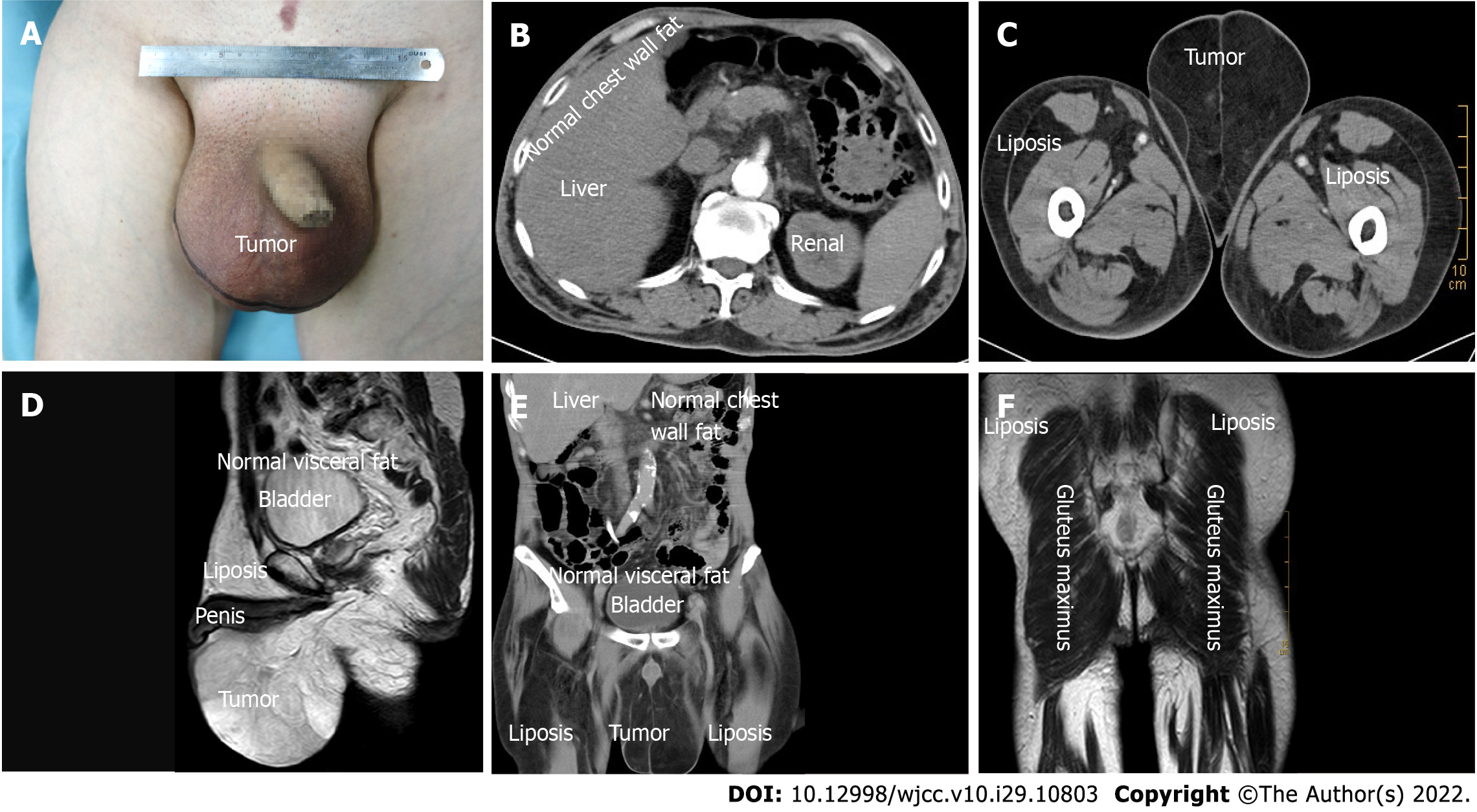
It was failure to touch spermatic cord and testes with negative light transmission test (Figure 1A).
Serum beta-human chorionic gonadotropin, alpha-fetoprotein and lactate dehydrogenase levels were normal. Abnormally decreased platelets were shown from the first operation (Table 1). A bone marrow test was performed, and immune thrombocytopenia was diagnosed.
| Test | First operation (3 yr ago) | Current operation | Normal reference range |
| CRP | < 5 | < 5 | 0-10 mg/L |
| hs-CRP | 2.74 | 3.56 | 0-3 mg/L |
| Hemoglobin | 136 | 130 | 131-172 g/L |
| Red blood cell count | 3.95 | 3.62 | 4-5.5 × 109/L |
| White blood cell count | 3.38 | 2.7 | 4-10 × 109/L |
| Platelets | 93 | 58 | 100-300 × 109/L |
| Cholinesterase | 3223 | 2587 | 5320-12920 |
| Glutamyltransferase | 233 | 256 | 8-73 |
| LDH | 360 | 366 | 120-250 g/L |
| Myoglobin | 29.3 | 22.4 | 25-58 |
| Glutamate dehydrogenase | 41 | 25 | 0-5 |
| Triglyceride | N/A | 1.38 | 0.48-1.7 |
| Apolipoprotein-A1 | N/A | 1.97 | 1-1.6 |
| Thyroid stimulating hormone | 13.52 | 8.39 | 0.27-4.2 |
| Ferritin | N/A | 942 | 30-400 μg/L |
Scrotal ultrasonography showed a slightly higher echogenic mass. The computed tomography (CT) scan showed diffuse fat accumulation in the scrotum, and its density was not uniform. The CT value range was approximately -66 to -94 Hu. The testicles on both sides were normal in size and compressed by the scrotal wall (Figure 1B-D). A magnetic resonance imaging (MRI) scan showed bilateral patchy abnormal signals on both scrotum, high signals on T1 weighted imaging and T2 weighted imaging (T2WI) scans, a low signal on a T2WI lipid-pressing sequence, no obvious diffusion-restricted signal changes on diffusion weighted imaging and apparent diffusion coefficient, and no obvious abnormal enhancement on an enhanced scan (Figure 1E and F).
Giant bilateral scrotal lipoma with abnormal somatic fat distribution.
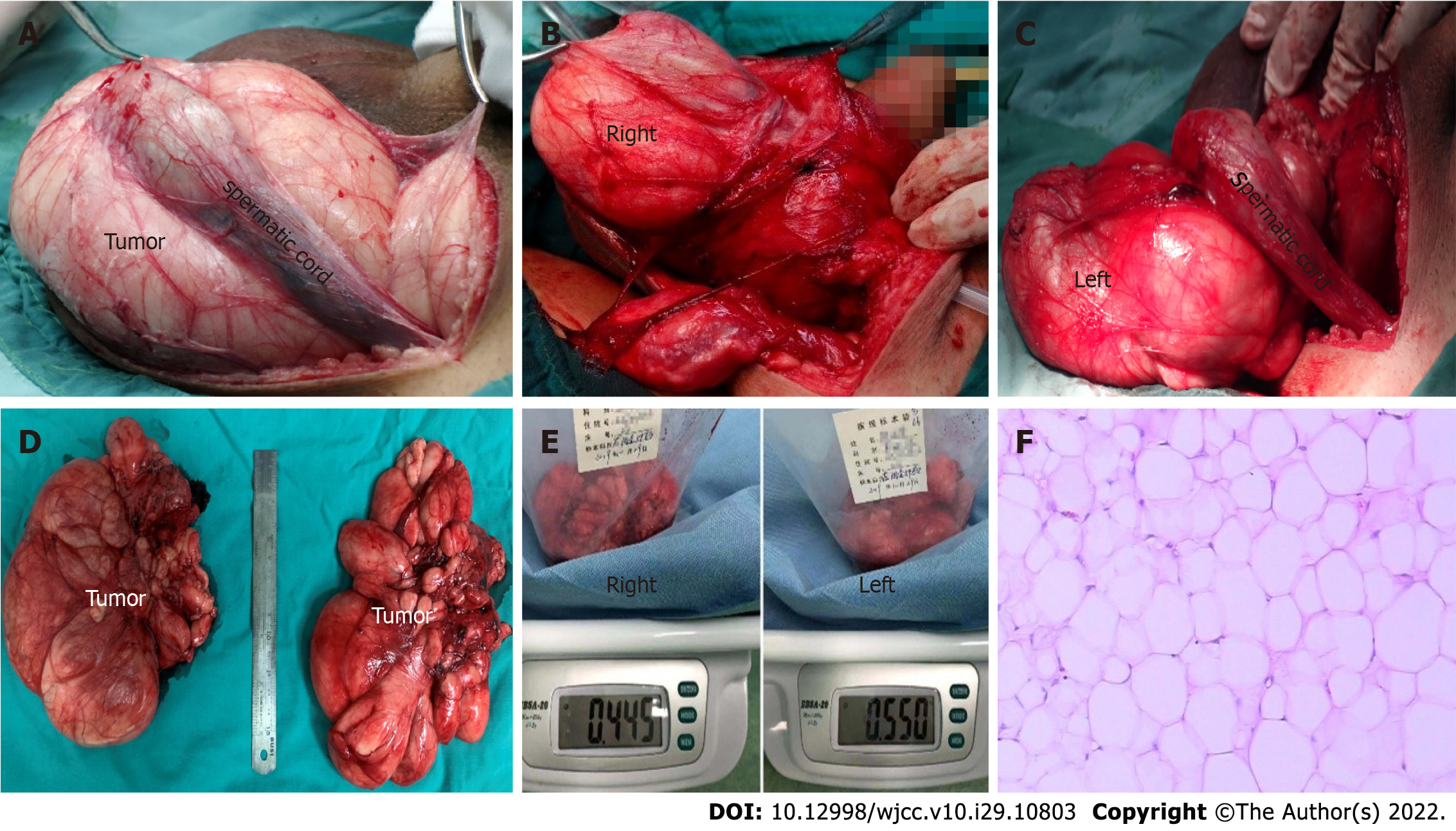
Surgical treatment was performed. The tumour squeezed the bilateral testis, epididymis and spermatic cord tightly against the inner wall of the scrotum, and the boundary between the tumour and the tumour was obvious. The capsules of both tumours were intact, lobulated, light yellow, and soft (Figure 2A-D). The cut surface was off-white and slightly tough. The total weight of bilateral scrotal tumours reached 995 g (Figure 2E). Bilateral scrotal lipomas were confirmed by postoperative pathology (Figure 2F). follow-up only postoperative, no radiotherapy and chemotherapy.
The patient was followed up for two years and no recurrence was found.
Scrotal lipoma is very rare, and only approximately 20 cases have been reported[3,6]. In most cases, the aetiology and origination are still unknown. Some patients are young[7], and the cause is suggested to be congenital[4]. However, some patients were older than 60 years, as shown in Table 2. An elderly patient with abnormal fat somatic distribution was reported herein, and its origin was discussed in this study.
| Ref. | Age (yr) | Place (side) | Size (cm) | Weight (g) | Symptom | Presumably origination | Midical history (yr) | Operation history | Follow-up (mo) | Outcome/prognosis |
| Cecil[1] | 44 | Left | 10. 5 × 9 × 7.5 | N/A | Hard lumb | Spermatic cord | 8 yr | Fractured rib | N/A | N/A |
| Livermor[2] | 75 | Left | 16.5 × 8.89 | 225 | Weight and pressure | Spermatic cord | 1 yr | Prostate surgery | N/A | N/A |
| Mccullough[20] | 49 | Left | Two 2.0 × 1.5 × 1.5 | N/A | Pressure | Spermatic cord | 5 yr | Inguinal surgery | N/A | N/A |
| Florante et al[8] | 20 | Right | 5 × 3.5 × 2 | N/A | Symptomless mass | Perineum | N/A | Contralateral inguinal surgery | N/A | No recurrence |
| Florante et al[8] | 76 | Right | 3 × 2 | N/A | Symptomless mass | Perineum | 2 mo | Prostate surgery | N/A | N/A |
| Fujimura and Kurokawa[4] | 19 | Right | 6.5 × 6 × 5 | 41 | Symptomless mass | Scrotum (tunica dartos) | 2 yr | N/A | N/A | No recurrence |
| Kryvenko et al[19] | 37 | Left | 26 × 14 (scrotum) | N/A | N/a | Scrotal wall | 18 mo | N/A | N/A | N/A |
| Kryvenko et al[19] | N/A | N/A | N/A | N/A | Inguinal and scrotal swelling | Inguinal canal | N/A | N/A | N/A | N/A |
| Szmigielski et al[16] | 67 | Both | 17 × 16 × 11 | N/A | Symptomless mass | Scrotal wall | 2 yr | Pulmonary embolism | N/A | N/A |
| Edelstein[15] | 48 | N/A | 7 × 6 | N/A | Scrotal swelling | Spermatic cord | 8 yr | Inguinal surgery | N/A | N/A |
| Kim et al[21] | 1 mo | Midline | 3 × 1.5 | N/A | N/A | Scrotal wall | Congenital | N/A | N/A | N/A |
| Sakorafas and Polychronopoulos[22] | 67 | N/A | N/A | N/A | Mild discomfort | Scrotal wall | 6 yr | N/A | N/A | No recurrence |
| Kaplanoglu et al[12] | 64 | Left | 10 × 9 × 5 | 550 | Painless swelling | Intrascrotal lipoma | 10 yr | N/A | 6 | No recurrence |
| Fabiani et al[9] | 22 | Left | 3 × 2 | N/A | Painful nodule | Intrascrotal lipoma | 3 mo | N/A | N/A | N/A |
| Creta et al[11] | 54 | Midline | 8 × 10 × 12 | 600 | Swelling | Scrotal wall | N/A | N/A | N/A | N/A |
| Srivastava et al[7] | 29 | Left | 15 × 10 | N/A | Increasing lump | Scrotum (tunica dartos) | N/A | N/A | N/A | No recurrence |
| Yamamichi et al[13] | 58 | Left | 14 × 6 | 250 | Swelling and discomfort | Scrotal wall | 46 yr | N/A | 6 | No recurrence |
| Vignot et al[23] | 47 | Left | 17 × 11 × 6 | 460 | Large left scrotal mass | Scrotal wall | 10 yr | N/A | N/A | No recurrence |
| Zheng et al[3] | 47 | Both | Right 9.9 × 4.5, left 10.8 × 5.6 | N/A | Progressively enlarging lumps | Scrotal wall | 8 mo | N/A | 5 | No recurrence |
| Seidu et al[5] | 28 | Right | 21 × 7 × 9 | 1100 | Inguinoscrotal swelling | Inguinal canal | 3 yr | N/A | N/A | N/A |
| Current case | 66 | Both | 13 × 11 × 10 | 995 | Swelling | Inguinal canal | 3 yr | Thrombocytopenia; cystolithotomy | 24 | No recurrence |
Florante et al[8] used the term "extratesticular" to describe scrotal tumours that do not directly affect the testes themselves. While 95% of testicular tumours are malignant, most paratesticular tumours, including scrotal lipoma, are benign[9].
Large scrotal lipomas often present with scrotal enlargement and discomfort[10-12]. A large right scrotal mass that weighed 1100 g was reported[5]. Yamamichi et al[13] reported a case of scrotal lipoma with a maximum diameter of 14 cm combined with liposarcoma (weight 250 g). The lesion described in the current report is the heaviest bilateral scrotal lipoma in the English-language literature[10-12], which was 995 g in weight (Figure 1D).
Scrotal lipomas can be divided into three types[14]: (1) Originating from the posterior spermatic cord and spreading into the scrotum; (2) Originating from the inside or outside of the spermatic cord, and (3) originating from fat lobules of the scrotal dartos tunica. The latter lipomas are called primary scrotal lipomas, and they usually occur in young individuals[4].
However, abnormal somatic fat distribution may be an important influencing factor in the current case. The CT and MRI results of this patient showed liposis of the lower abdomen, perineum and thigh but no liposis in the chest wall or pelvic cavity (Figure 1B-F). Excess fat around the penis was shown on MRI (Figure 1D). A fat test was performed, and only apolipoprotein-A1 was slightly increased (Table 1). Multiple metabolic enzyme abnormalities were also shown, which lasted for three years in this case (Table 1). These results showed that bilateral scrotal lipoma in elderly individuals may be a symptom of abnormal somatic fat distribution caused by metabolic diseases. Because the scrotal tissue is loose and extensible, which is more suitable for fat accumulation, bilateral scrotal lipoma developed. Recently, a giant bilateral scrotal lipoma along with multiple lipomas was also reported[3]. Indirect evidence can also be provided by many patients with obesity[15].
The aetiology of scrotal lipoma is still unclear. In addition to congenital factors[4], local pluripotent cells develop into adipocyte lines[15]. Moreover, injury may be a factor when the lesion originates from the spermatic cord or inguinal canal in elderly individuals[2]. We reviewed the English-language literature, and a history of inguinal or pelvic surgery was reported in 6 patients, including the current patient (21 patients total, Table 2). However, a small mass similar to a peanut was observed before this patient’s first operation three years ago. There was one case of contralateral inguinal surgery in the literature[8]. However, these results suggest that inguinal or pelvic surgery is an accelerating factor, if not an initiating factor.
Blood diseases may also play a role in the tumorigenesis of scrotal lipoma. This current case was diagnosed as primary thrombocytopenia due to decreased platelets for more than 3 years. Szmigielski et al[16] reported a case of a large scrotal lipoma that arose after venous thrombosis and pulmonary embolism. The scrotal mass in the 67-year-old patient was approximately 9 cm × 11 cm after taking oral anticoagulants for 3 mo.
Ultrasonography and MRI play an important role in the evaluation of scrotal lipoma[11]. Ultrasound is the first choice for an investigation tool. MRI is the most sensitive method to distinguish a benign lesion from a malignant lesion. High T1 signal strength is a characteristic of fat-containing tumours. Nevertheless, it is difficult to distinguish low-grade liposarcoma from benign lipoma based on MRI findings alone[17]. Complete removal of a tumour by surgery and pathological examination can confirm lipoma[11]. Lipoma is homogenous, and its CT values are between -50 and -150 Hounsfield units; this information can help in the identification of liposarcoma[16].
If lipomas are excluded, more than 50% of spermatic cord tumours are malignant[18]. If the tumour grows rapidly beyond 10 cm, liposarcoma should be considered in the differential diagnosis[19]. To our knowledge, this is the longest reported postoperative follow-up time. Yamamichi et al[13] reported a case and follow-up for six months[13]. Kaplanoglu et al[12] reported a case of intrascrotal lipoma (weight 550 g) with a diameter of 10 cm[12]. No tumour recurrence was observed after six months of follow-up. The main limitation of this study is that it is a case report, and there are no genomic data.
To our knowledge, this is the heaviest bilateral scrotal lipoma and the longest postoperative follow-up time in English-language literature. Bilateral scrotal lipoma in elderly maybe as part of the symptoms of abnormal somatic fat distribution, which caused by metabolic diseases. Inguinal or pelvic surgery is an accelerating factor, if not an initiating factor. Blood system diseases may also play a role in the tumorigenesis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Carannante F, Italy; Wang P, China S-Editor: Wang DM L-Editor: A P-Editor: Wang DM
| 1. | Cecil AB. Intrascrotal lipomata. J Urol. 1927;17:557-568. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | LIVERMORE GR. Lipoma of the scrotum; case report. J Urol. 1948;60:153-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Zheng W, Shi M, Li T, Xu H, Chen Z, Wang X, Bai S, Le W, Yang L, Wei Q. Giant bilateral primary scrotal lipoma along with lipomas in multiple sites of the body: a case report and literature review. Transl Androl Urol. 2021;10:983-990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Fujimura N, Kurokawa K. Primary lipoma of the scrotum. Eur Urol. 1979;5:182-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Seidu AS, Yorke J, Akpaloo J, Danso P, Sukenibe SS, Fiifi-Yankson PK, Adae-Aboagye K, Amoah G, Yamoah FA, Afful-Yorke D, Agyeman-Gyebi SNP, Brenu SG, Adjei E. Giant primary scrotal lipoma in a low-resource setting: challenges with diagnosis and review of literature. J Surg Case Rep. 2021;2021:rjab398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Galosi AB, Scarpelli M, Mazzucchelli R, Lopez-Beltran A, Giustini L, Cheng L, Montironi R. Adult primary paratesticular mesenchymal tumors with emphasis on a case presentation and discussion of spermatic cord leiomyosarcoma. Diagn Pathol. 2014;9:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Srivastava KN, Agarwal A, Siddharth Vikram SS, Gupta M. Huge scrotal lipoma posing a diagnostic dilemma: A case report and review of literature. Urol Case Rep. 2017;15:39-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Florante J, Leyson J, Doroshow LW, Robbins MA. Extratesticular lipoma: report of 2 cases and a new classification. J Urol. 1976;116:324-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Fabiani A, Principi E, Filosa A, Pieramici T, Fioretti F, Maurelli V, Servi L, Mammana G. An unusual case of primary intrascrotal lipoma. Arch Ital Urol Androl. 2016;88:345-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Masciovecchio S, Saldutto P, Del Rosso A, Galatioto GP, Vicentini C. [An unusual case of massive funicular lipoma]. Urologia. 2014;81:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Creta M, De Stefano G, Buonopane R, Barba C, Di Meo S, Imperatore V, Imbimbo C, Mirone V. Giant primary scrotal lipoma: A case report. Arch Ital Urol Androl. 2017;89:243-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kaplanoglu V, Kaplanoglu H, Parlak IS, Tatar IG. Giant intrascrotal lipoma. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Yamamichi G, Nakata W, Yamamoto A, Tsujimura G, Tsujimoto Y, Nin M, Tsujihata M. Liposarcoma of the spermatic cord associated with scrotum lipoma: A case report and review of the literature. Urol Case Rep. 2018;17:114-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Mostofi FK, Price EB. Tumors of the male genital system. Ar For Instit of Pathol. 1973;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 15. | Edelstein RA. Giant spermatic cord lipoma. ScientificWorldJournal. 2009;9:1194-1196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 16. | Szmigielski W, Khairat M, Haider A, Ejeckam GC. Huge scrotal lipoma masquerading as haematoma. Clin Radiol. 2000;55:479-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Muglia V, Tucci S Jr, Elias J Jr, Trad CS, Bilbey J, Cooperberg PL. Magnetic resonance imaging of scrotal diseases: when it makes the difference. Urology. 2002;59:419-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Patel NG, Rajagopalan A, Shrotri NS. Scrotal liposarcoma - a rare extratesticular tumour. JRSM Short Rep. 2011;2:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Kryvenko ON, Rosenberg AE, Jorda M, Epstein JI. Dedifferentiated liposarcoma of the spermatic cord: a series of 42 cases. Am J Surg Pathol. 2015;39:1219-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | McCULLOUGH CP. Unusual scrotal lipoma associated with sigmoid diverticulum. Calif Med. 1953;79:449-450. [PubMed] |
| 21. | Kim SO, Im CM, Joo JS, Oh KJ, Jung SI, Park K, Choi C, Kang TW, Kwon D, Ryu SB. Scrotal primary lipoma with unusual clinical appearance in newborn. Urology. 2009;73:1024-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Sakorafas GH, Polychronopoulos D. Giant scrotal lipoma. Eur J Cancer Care (Engl). 2010;19:e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Vignot L, Saad E, Peyromaure M, Barry Delongchamps N. Giant Primary Scrotal Lipoma: A Rare Entity with Diagnostic Pitfalls. Case Rep Urol. 2020;2020: 8815845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |