Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10728
Peer-review started: May 31, 2022
First decision: August 4, 2022
Revised: August 18, 2022
Accepted: September 7, 2022
Article in press: September 7, 2022
Published online: October 16, 2022
Processing time: 120 Days and 23.5 Hours
Tumors originating from the posterior bladder wall can be challenging to dia
A 29-year-old woman with a uterine fibroid incidentally found at a regular checkup was referred to our hospital. Based on magnetic resonance imaging, either urinary bladder leiomyoma or protrusion of pedunculated uterine cervical fibroid into the bladder was suspected. This leiomyoma in the trigone of the bladder was completely excised by laparotomy, and the patient was discharged without complication. Follow-up outpatient ultrasonography identified tumor recurrence after four years. As focal atypia was identified previously, laparotomy was performed to confirm the pathology. A round solid mass was resected from the posterior bladder wall without injuring either ureteric orifice. This tumor was pathologically diagnosed as a leiomyoma without atypia. Three-year follow-up ultrasonography has revealed no recurrence.
Atypical leiomyoma in bladder trigone is rare and could be easily mistaken for fibroid in the uterine cervix. To confirm histopathology, surgical excision is mandatory and regular follow-up is necessary to detect recurrence.
Core Tip: Diagnosis of a tumor originating from the bladder trigone is challenging because it may mimic a mass from the uterine cervix. Magnetic resonance imaging is considered superior to computed tomography or ultrasonography for assessing bladder leiomyoma. Leiomyoma in bladder trigone requires caution during surgery because it can cause damage to the adjacent ureter. Surgical removal is mandatory for histopathological confirmation since it can be atypical fibroids or sarcomas. Regular follow-up is essential to detect recurrence.
- Citation: Song J, Song H, Kim YW. Recurrent atypical leiomyoma in bladder trigone, confused with uterine fibroids: A case report. World J Clin Cases 2022; 10(29): 10728-10734
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10728.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10728
Mesenchymal tumors represent 5% of all urinary bladder tumors[1]. Leiomyomas of the urinary bladder are very rare neoplasms, with an incidence of 0.43% of all bladder tumors[2]. Leiomyomas can be submucosal, intramural, or extravesical. Submucosal (i.e., endovesical) leiomyomas are the most common, corresponding to 63%-86% of all cases, while intramural and extravesical leiomyomas represent 3%-7% and 11%-30% of cases, respectively[3,4]. Women make up 76% of the total patient population for leiomyomas[4]. Patients present most commonly with obstructive urinary symptoms (49%), irritative symptoms (38%), hematuria (11%), or flank pain (13%), but nearly 19% of patients are asymptomatic[4].
Imaging studies such as ultrasonography or magnetic resonance imaging (MRI) are effective methods to predict histopathology. In ultrasonography, atypical leiomyoma demonstrated irregular cauliflower shape and homogenous enhancement[5]. In the MRI view, atypical myoma is similar to bladder malignancy rather than bladder leiomyoma, showing an isointense signal on T1- and T2-weighted images and an uneven surface with a cauliflower-like appearance[5]. However, there is no definitive imaging finding that could diagnose atypical bladder leiomyoma.
We report the case of a 29-year-old woman with surgically resected recurrent atypical bladder leiomyoma and recurred bladder leiomyoma. In this case, we reviewed the diagnosis, treatment, and precautions for the treatment of atypical bladder leiomyoma with the relevant literature.
The patient was incidentally diagnosed with a uterine fibroid at a clinic. Following diagnosis, the patient was referred to our center, a tertiary care hospital, for treatment.
A 29-year-old woman was diagnosed with a uterine fibroid on ultrasonography at a regular checkup and was referred to our hospital for surgical treatment. She denied any specific symptoms.
The patient’s clinical history was insignificant, and she had no other diseases.
The patient’s personal and family history was insignificant, and she had no other diseases.
Laboratory findings were non-specific except for micro-hematuria (red blood cell: 5–9/high power field (HPF) in urine sediment examination), and no abnormalities were found on physical examination.
The laboratory findings were as follows: Hemoglobin (14.3 g/dL), white blood cell count (8810/mm3), platelet count (311000/mm3), sodium (139 mmol/L), potassium (3.8 mmol/L), fasting blood glucose (97 mg/dL), creatinine (0.6 mg/dL), aspartate aminotransferase (28 U/L), and alanine aminotransferase (37 U/L).
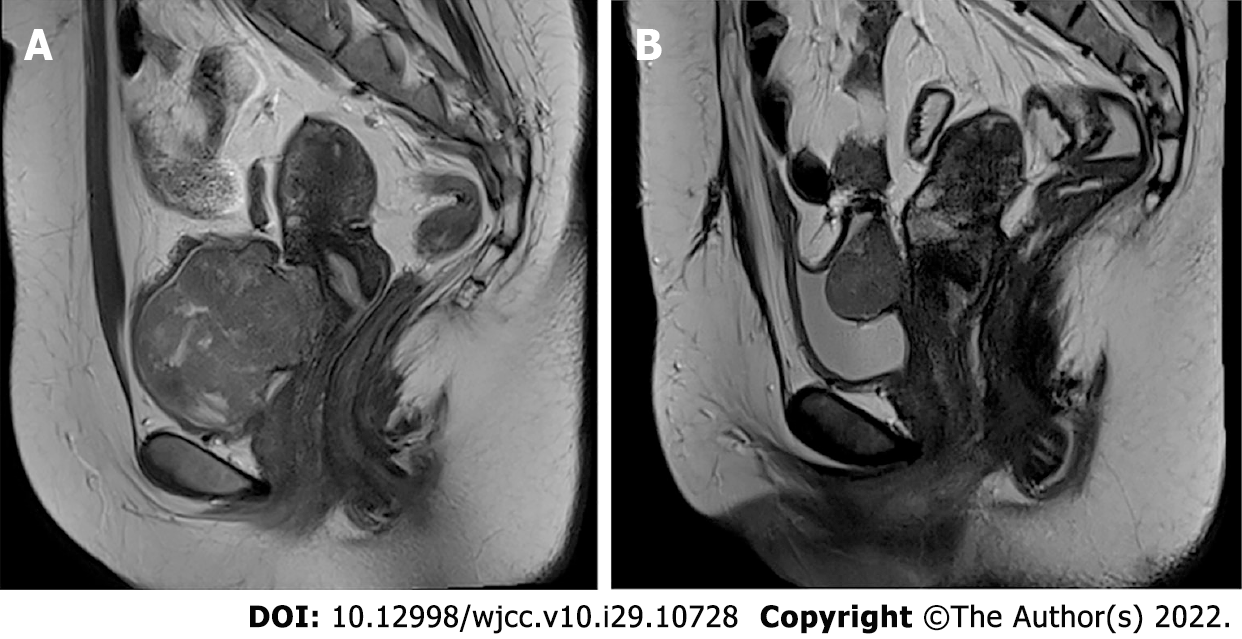
Ultrasonography revealed a 6 cm × 4.6 cm solid mass between the uterine wall and bladder. We considered the tumor a uterine fibroid, and a pelvis MRI was performed to determine the exact anatomical location. Based on MRI findings, the mass was suspected leiomyoma (6 cm × 4.6 cm) between the cervix and urinary bladder. The mass protruded into the urinary bladder with relatively increased signal intensity on T2-weighted image suggesting high cellularity and ruling in either bladder leiomyoma or pedunculated cervical fibroid (Figure 1A).
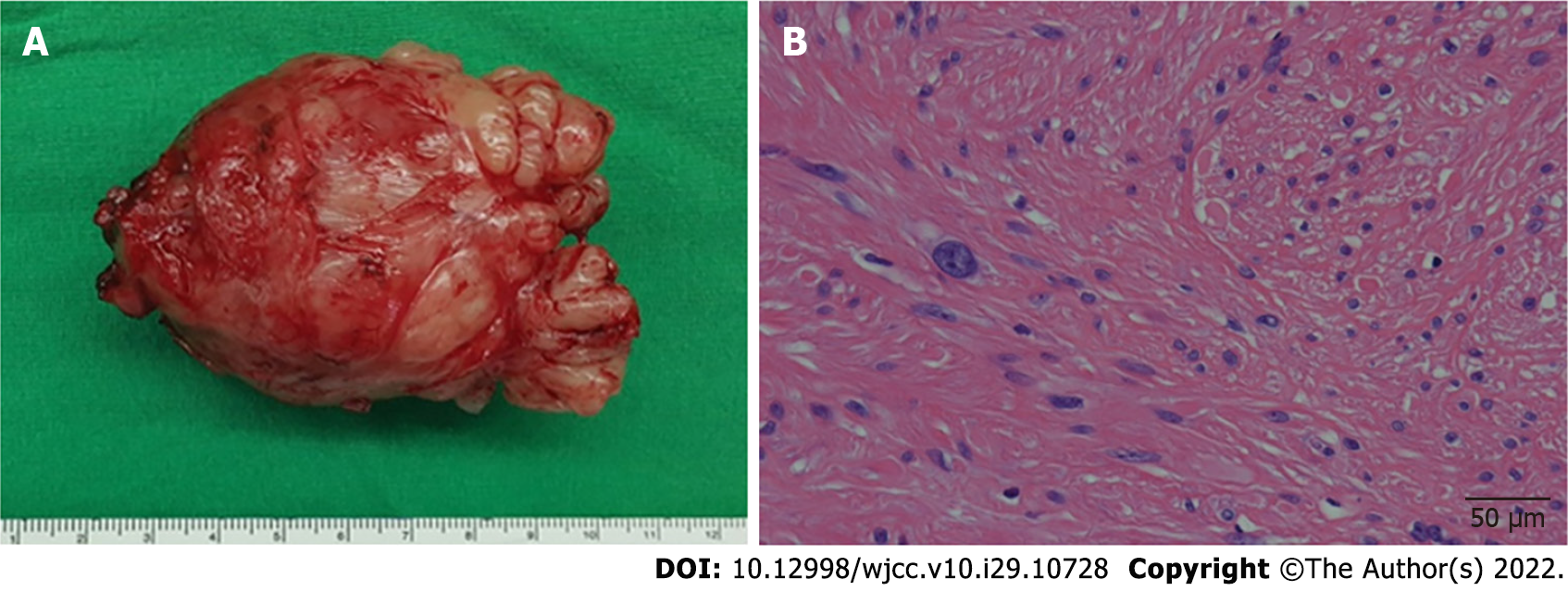
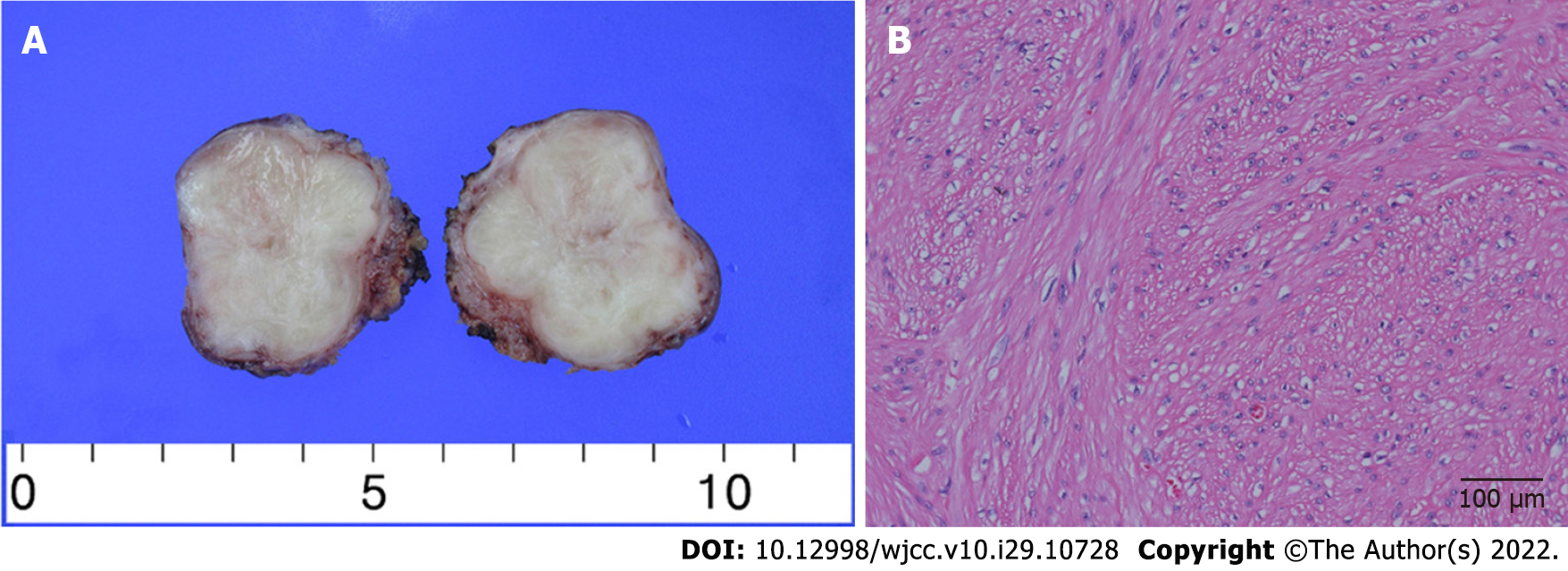
The final diagnosis of the initial case was bladder leiomyoma with focal atypia (mitotic count: 1/10 HPF). In the recurrent case, bladder leiomyoma without atypia was diagnosed.
Magnetic resonance imaging was performed before surgery, but considering the incidence, we focused on pedunculated uterine fibroid rather than bladder leiomyoma. Therefore, instead of cystoscopy, laparotomy was performed. No mass was found in the pelvic cavity when the abdominal wall was incised. Therefore, we made an incision on the bladder and found a submucosal tumor. The tumor was resected by visually complete excision. Both ureteral orifices were deviated due to mass effect. To avoid damage to the ureteral orifices, we performed bilateral Double J-stent placement before tumor resection. It was a well-demarcated single tumor (Figure 2A), and histopathological examination revealed a focally atypical leiomyoma with mitotic count of 1/10 HPF (Figure 2B). Necrotic features were absent. The patient was discharged without any complications. The bilateral Double-J catheters were removed two weeks after surgery.
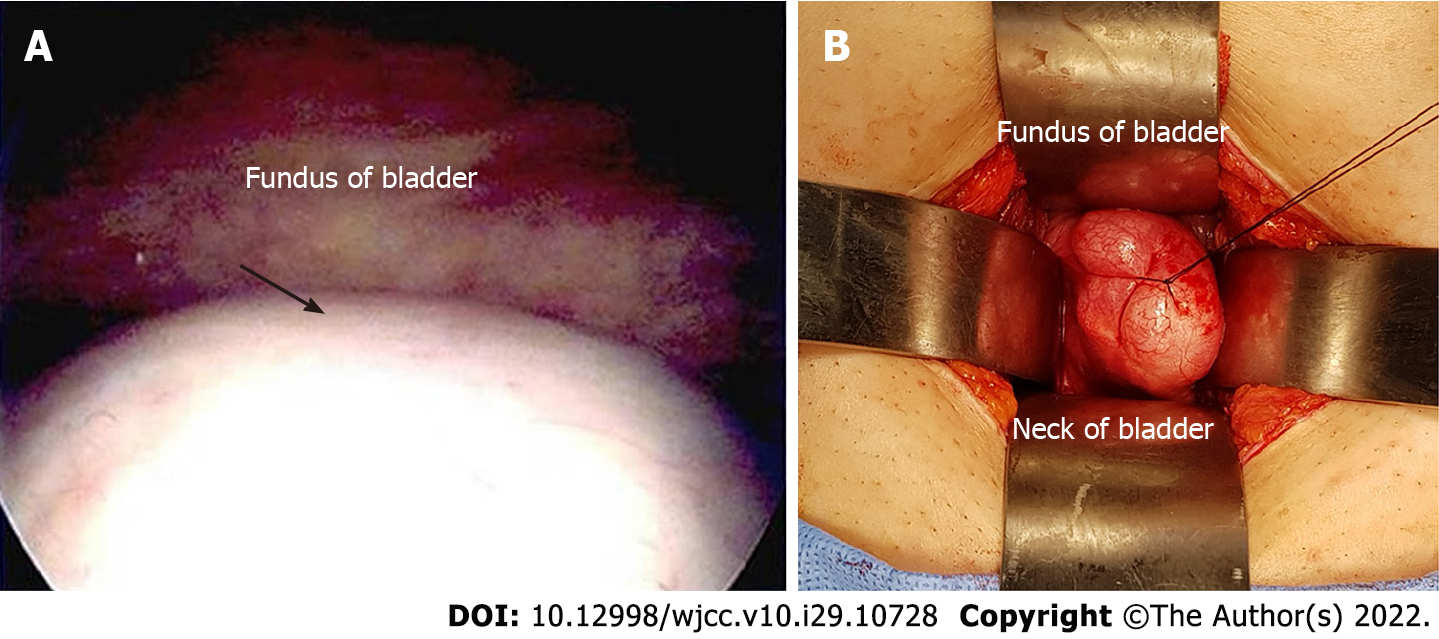
At both six months and one year after surgery, no recurrence was found on ultrasonography. However, tumor recurrence was detected by ultrasonography without specific symptoms when the patient visited our hospital for a third checkup, four years after surgery. Cystoscopy revealed a protruding mass in the posterior bladder wall (Figure 3A). For further evaluation, a preoperative MRI revealed a 3.8 cm × 3 cm-sized homogeneous mass on the posterior wall of the bladder (Figure 1B). Transvesical laparotomy was performed considering recurrence of the previous pathology, atypical leiomyoma. A round solid mass was found in the bladder trigone during surgery (Figures 3B and 4A), and it was resected without injuring either ureteric orifice. This well-encapsulated tumor was found to be leiomyoma without atypia on permanent pathology (Figure 4B).
There were no complications after surgery, and there has been no recurrence for more than three years, as observed on follow-up ultrasonography.
Leiomyoma is a benign disease that can develop from fibroblasts found in any part of the body, including the genitourinary tract. However, bladder leiomyoma is a rare condition, accounting for only 0.43% of all bladder tumors[2,6]. Leiomyoma can be endovesical, intramural, and extravesical. Endovesical origin is also known as submucosal origin, which is the most frequent site and more symptomatic than other origins. Leiomyoma affects individuals with a wide age range (22-78 years)[7] and is more predominant in women, especially in recently published case series[8,9].
Our case was asymptomatic except for microhematuria. However, since various symptoms, such as urinary retention, hematuria, and dyspareunia, are possible[4,7-12], a thorough history is necessary. In a review by Goluboff et al[4], 49% of the 37 patients presented with obstructive symptoms, 38% showed irritative symptoms, 11% had hematuria, and 19% were asymptomatic. In a case report by Xin et al[10], a 44-year-old female with dyspareunia was diagnosed with bladder leiomyoma coexisting with uterine leiomyoma on histological examination. Saidi et al[11] reported leiomyoma of the urinary bladder presenting with hematuria, and Ameli et al[12] reported atypical leiomyoma of the bladder presenting as flank pain.
Magnetic resonance imaging is considered to be superior to computed tomography (CT) or ultrasonography for assessing bladder leiomyoma[1,8,13]. Leiomyoma shows intermediate signal intensity on T1-weighted MR images and low signal intensity on T2-weighted MR images[1,14]. In our case, atypical bladder leiomyoma showed hypercellularity on MRI. However, imaging findings could not accurately diagnose atypical bladder leiomyoma. Therefore, pathological confirmation was the best option to diagnose atypical bladder leiomyoma.
Cystoscopy is a high-value diagnostic tool that can show the leiomyoma’s morphology and anatomical location[12]. Moreover, cystoscopy can be used to confirm the histopathology of bladder mass. However, cystoscopy, an invasive procedure, is usually performed when abnormalities in the urethra or bladder are detected on imaging tests[15,16]. One of the limitations of cystoscopy is that if the mass size is too large it is difficult to determine the overall contour considering this case. Cystoscopy could be contraindicated in the presence of acute urinary tract infection or urethral stricture[16].
Before the first surgery, since bladder leiomyomas are very rare, we thought that uterine fibroids were more likely and did not perform preoperative cystoscopy. At the time of recurrence, cystoscopy was performed, but a biopsy was not performed because it was assumed that the recurrent mass would be the same atypical bladder leiomyoma as before. Unlike our expectations, the final diagnosis was leiomyoma without atypia. Although we did not perform cystoscopy and biopsy, the procedures would have been helpful in determining preoperative diagnosis. If fibroids protruding from the cervix to the bladder are found on imaging tests, though rare, there is a possibility of bladder fibroids, so a cys
There are several surgical approaches to resect bladder myoma. According to anatomical position, abdominal, transvaginal, transurethral, or laparoscopic resection may be possible. In malignancy, a huge or recurrent mass in an unfavorable location should be excised through an abdominal or laparoscopic approach for complete resection. Murota et al[17] presented a laparoscopic partial cystectomy case using both retroperitoneoscopic and transurethral procedures to treat a leiomyoma sized 2 cm on the right wall of the bladder. Once the mass was palpable through the vagina, it could be removed via a transvaginal approach[18]. If a small tumor is located within the endovesical wall of the bladder, it can be managed with transurethral resection. Zachariou et al[19] reported transurethral resection of a bladder trigone leiomyoma.
As with our case report, if protruding subserosal leiomyoma of the uterine cervix is suspected in imaging studies, a differential diagnosis for the tumor-originated bladder is required. Such masses could either be sarcoma or other malignant masses. Therefore, surgeons should be mindful of several possibilities to decide on better treatment options. In a case reported by Asano et al[20], a 32-year-old woman with hematuria and suspicious bladder myoma underwent resection for treatment. However, alveolar soft part sarcoma was reported later on final pathology[20].
Recurrent cases are very rare in atypical or benign bladder leiomyoma. Khater et al[13], who reviewed 36 reports for bladder leiomyoma, reported no recurrent cases. Conversely, 2 recurrent bladder leiomyomas in all 9 cases were reported, and no recurrent disease was noted after the complete recurrent lesion of bladder leiomyoma[14]. To avoid recurrent disease, complete resection was effective and important method[13]. In large-sized bladder leiomyoma, partial cystectomy was considered to obtain complete resection with a clear surgical margin[21]. In the first surgery of this case, the tumor was completely removed visually. However, given the recurrence of leiomyoma, it appears that the tumor has not been removed with a sufficiently wide and deep margin because there were ureteral orifices right next to the tumor and the cervix behind it.
There are only a few case reports of recurrence after leiomyoma resection, as in our case[14,21]. Although rare, recurrence is possible in some cases, and regular outpatient follow-up is necessary after surgical treatment.
Leiomyoma in bladder trigone is rare and could be easily mistaken for fibroid in the uterine cervix. Magnetic resonance imaging is an effective method of assessing the anatomical position of a leiomyoma. Surgical excision is mandatory to confirm pathology since it can be atypical fibroids or sarcomas, and regular follow-up is necessary to detect recurrence.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gadelkareem RA, Egypt; Kołat D, Poland; Tan B, China; Yadav P, India S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Wong-You-Cheong JJ, Woodward PJ, Manning MA, Sesterhenn IA. From the Archives of the AFIP: neoplasms of the urinary bladder: radiologic-pathologic correlation. Radiographics. 2006;26:553-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 154] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 2. | Blasco Casares FJ, Sacristán Sanfelipe J, Ibarz Servio L, Batalla Cadira JL, Ruiz Marcellán FJ. [Characteristics of bladder leiomyoma in our setting]. Arch Esp Urol. 1995;48:987-990. [PubMed] |
| 3. | Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol. 1986;136:906-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Goluboff ET, O'Toole K, Sawczuk IS. Leiomyoma of bladder: report of case and review of literature. Urology. 1994;43:238-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 81] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Wu S. Imaging findings of atypical leiomyoma of the urinary bladder simulating bladder cancer: a case report and literature review. Med Ultrason. 2013;15:161-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Cornella JL, Larson TR, Lee RA, Magrina JF, Kammerer-Doak D. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol. 1997;176:1278-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Martin SA, Sears DL, Sebo TJ, Lohse CM, Cheville JC. Smooth muscle neoplasms of the urinary bladder: a clinicopathologic comparison of leiomyoma and leiomyosarcoma. Am J Surg Pathol. 2002;26:292-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Matsushima M, Asakura H, Sakamoto H, Horinaga M, Nakahira Y, Yanaihara H. Leiomyoma of the bladder presenting as acute urinary retention in a female patient: urodynamic analysis of lower urinary tract symptom; a case report. BMC Urol. 2010;10:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Rey Valzacchi GM, Pavan LI, Bourguignon GA, Cortez JP, Ubertazzi EP, Saadi JM. Transvesical laparoscopy for bladder leiomyoma excision: a novel surgical technique. Int Urogynecol J. 2021;32:2543-2544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Xin J, Lai HP, Lin SK, Zhang QQ, Shao CX, Jin L, Lei WH. Bladder leiomyoma presenting as dyspareunia: Case report and literature review. Medicine (Baltimore). 2016;95:e3971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Saidi R, Lefi M, Touffahi M, Farhane S, Saad H. [Leiomyoma of the urinary bladder]. Prog Urol. 2002;12:493-496. [PubMed] |
| 12. | Ameli M, Rahmandoost M. Elderly patient with atypical leiomyoma of the bladder presenting as flank pain: A case report. Arch Ital Urol Androl. 2017;89:327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Khater N, Sakr G. Bladder leiomyoma: Presentation, evaluation and treatment. Arab J Urol. 2013;11:54-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Park JW, Jeong BC, Seo SI, Jeon SS, Kwon GY, Lee HM. Leiomyoma of the urinary bladder: a series of nine cases and review of the literature. Urology. 2010;76:1425-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | McCarthy TC. Cystoscopy and biopsy of the feline lower urinary tract. Vet Clin North Am Small Anim Pract. 1996;26:463-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Messer JS, Chew DJ, McLoughlin MA. Cystoscopy: techniques and clinical applications. Clin Tech Small Anim Pract. 2005;20:52-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Murota T, Komai Y, Danno S, Fujita I, Kawakita M, Matsuda T. Endoscopic partial cystectomy for bladder leiomyoma using retroperitoneoscopic and transurethral procedures. Int J Urol. 2002;9:190-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Yin FF, Wang N, Wang YL, Bi XN, Xu XH, Wang YK. Transvaginal Resection of a Bladder Leiomyoma Misdiagnosed with a Vaginal Mass: A Case Report and Literature Review. Case Rep Obstet Gynecol. 2015;2015:981843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Zachariou A, Filiponi M, Dimitriadis F, Kaltsas A, Sofikitis N. Transurethral resection of a bladder trigone leiomyoma: a rare case report. BMC Urol. 2020;20:152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Asano A, Nishikimi T, Morikami H, Ohashi T, Yamauchi Y, Ishida R, Yamada H, Kobayashi H, Tsuduki T. [A primary bladder alveolar soft part sarcoma: a case report]. Nihon Hinyokika Gakkai Zasshi. 2021;112:45-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Bangash M, Faruqui N, Muhammad AU, Uddin Z. Leiomyoma Urinary Bladder, Mimicking Urothelial Cancer. J Ayub Med Coll Abbottabad. 2021;33:685-689. [PubMed] |