Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10713
Peer-review started: May 10, 2022
First decision: July 13, 2022
Revised: July 19, 2022
Accepted: September 8, 2022
Article in press: September 8, 2022
Published online: October 16, 2022
Processing time: 140 Days and 5.2 Hours
Large abdominal wall defect (LAWD) caused by shotgun wound is rarely reported.
Herein, we describe a case of LAWD caused by a gunshot wound in which the abdominal wall was reconstructed in stages, including debridement, tension-reduced closure (TRC), and reconstruction with mesh and a free musculocutaneous flap. During a 3-year follow-up, the patient recovered well without hernia or other problems.
TRC is a practical approach for the temporary closure of LAWD, particularly in cases when one-stage abdominal wall restoration is unfeasible due to significant comorbidities.
Core Tip: The large full-thickness abdominal defect caused by gunshot wound is often associated with infection, multiorgan injuries, and poor patient conditions. Tension-reduced closure is a useful method for the temporary closure of large abdominal wall defect, particularly in cases in which one-stage abdominal wall reconstruction is unfeasible.
- Citation: Li Y, Xing JH, Yang Z, Xu YJ, Yin XY, Chi Y, Xu YC, Han YD, Chen YB, Han Y. Tension-reduced closure of large abdominal wall defect caused by shotgun wound: A case report. World J Clin Cases 2022; 10(29): 10713-10720
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10713.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10713
Large abdominal wall defect (LAWD) is commonly caused by tumor resection, followed by infection, trauma, and radiation-induced injury[1]. LAWD caused by gunshot wound has been rarely reported in the previous literature[2]. Gunshot wounds often lead to full-thickness defects, infection, multiorgan injuries, and poor patient conditions making reconstruction of LAWD extremely challenging[3]. Conventional one-stage reconstruction with mesh reinforcement plus free flap may be unfeasible and staged reconstruction is required[4].
Tension-reduced closure (TRC) is a novel technique for the closure of large wounds by reducing the tension across the wound edges based on the theories of stress relaxation and mechanical creep for skin stretching[5]. Previous studies have shown that TRC is a simple, effective, and safe method for wound closure for a variety of reasons. However, no study to date has reported the use of TRC for LAWD caused by a gunshot wound. Here, we report a case of gunshot LAWD, who underwent staged abdominal wall reconstruction including debridement, temporary TRC, and definitive reconstruction with prosthetic mesh plus a free flap.
Abdominal wall hernia formation after abdominal gunshot wound.
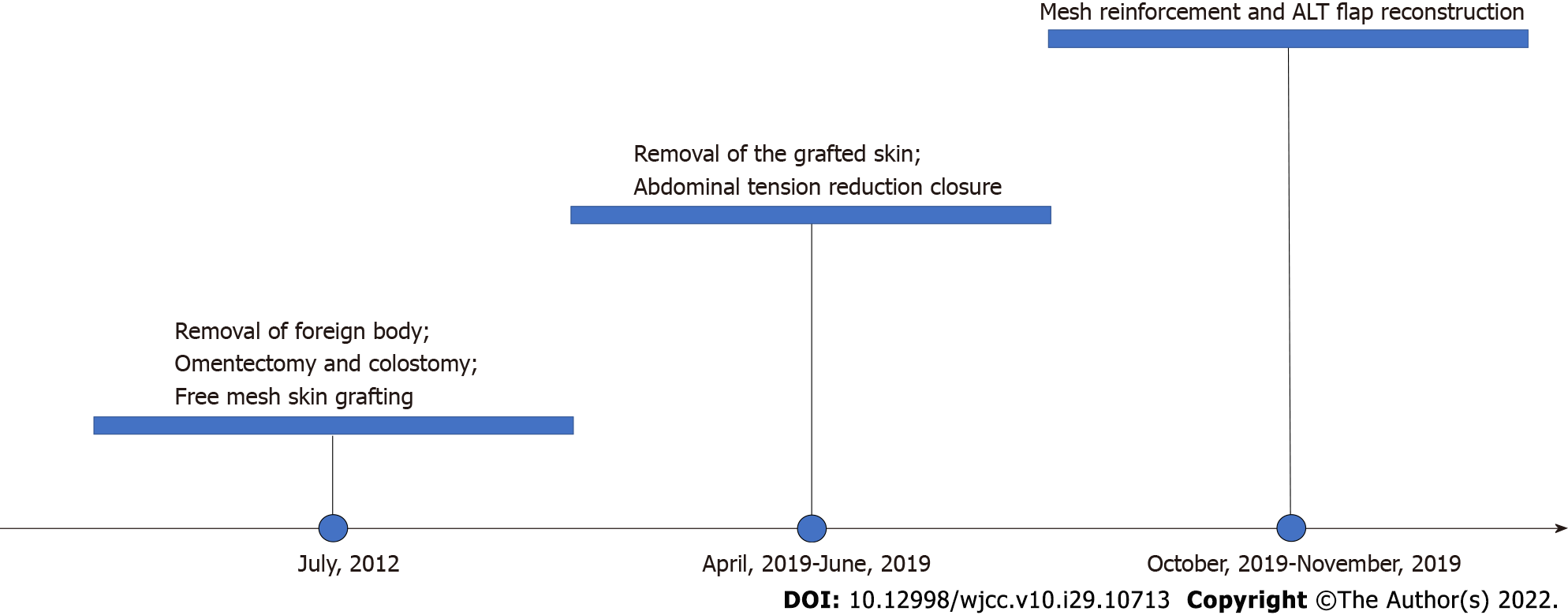
A 44-year old man presented with a large abdominal bulge. He was robbed and shot in the abdomen in South Africa 1.5 years ago, resulting in open abdomen, hemorrhagic shock, infection, intestinal exposure, and severe multiorgan injures involving the transverse colon, greater omentum, spleen, diaphragm, and left kidney. Emergency surgeries including removal of bullets and foreign body, debridement, transverse colectomy, omentectomy, nephrectomy, and colostomy were performed at a local hospital in South Africa. The large full-thickness abdominal wall defect was initially covered by split-thickness skin mesh grafting on intestines harvested from the left thigh.
The patient had hepatitis and underwent left kidney removal after a gunshot wound on July 26, 2017.
The patient denied a family history of infectious and genetic diseases.
The patient developed a large abdominal hernia and was referred to our hospital for abdominal reconstruction 1.5 years after the initial injury. A 26 cm × 28 cm full thickness abdominal defect covered with grafted skin mesh was found at the first consultation. The hernia was protruding when he was standing or lying on one side. Underlying peristalsis was observed. A colostomy stoma was located at 10 cm close to the skin grafts and connected with a colostomy bag.
Laboratory examinations showed no significant abnormalities.
Ultrasound examination results were consistent with changes in the abdominal wall defect after trauma.
The final diagnosis were postoperative abdominal wall trauma, abdominal wall defect, and abdominal wall hernia.
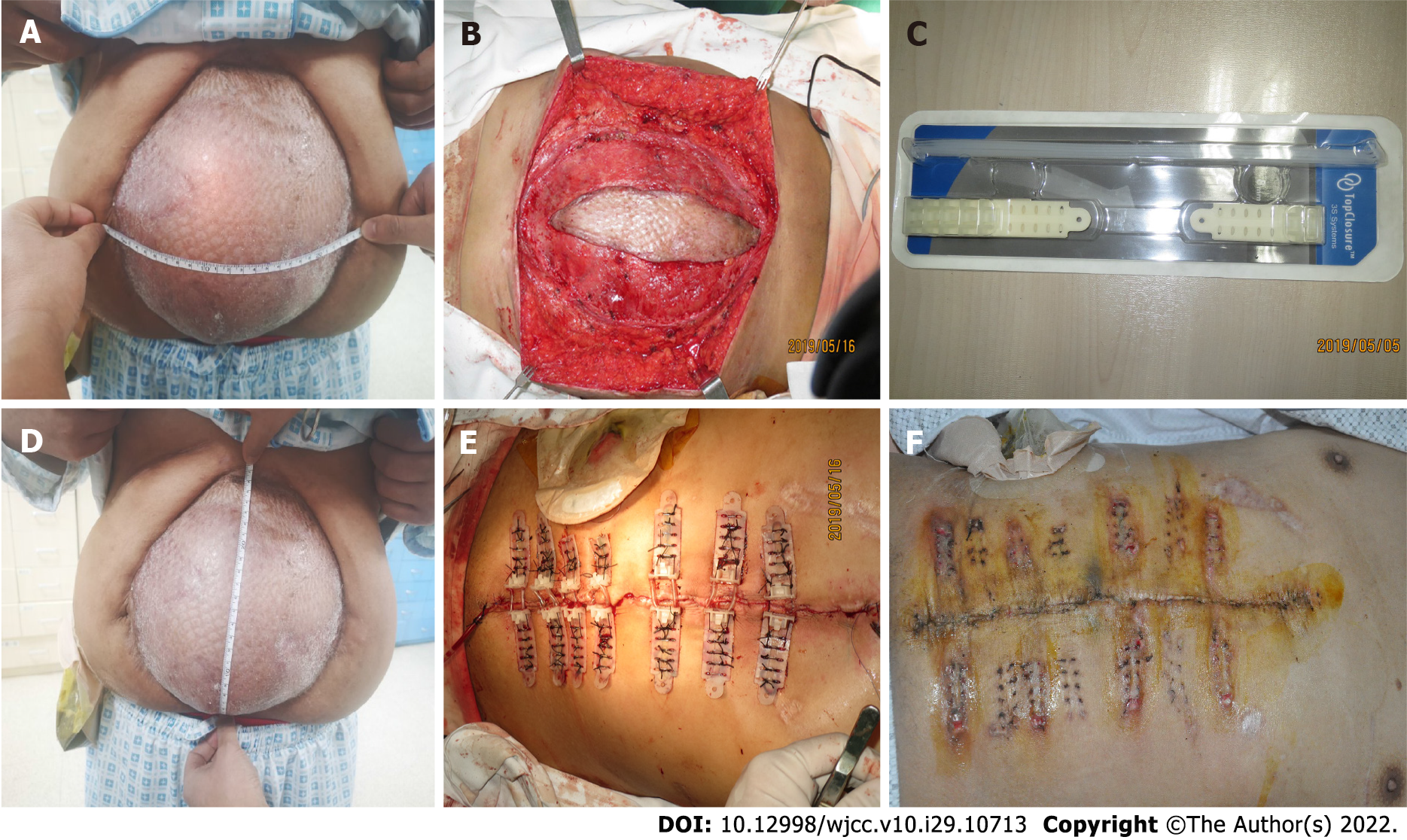
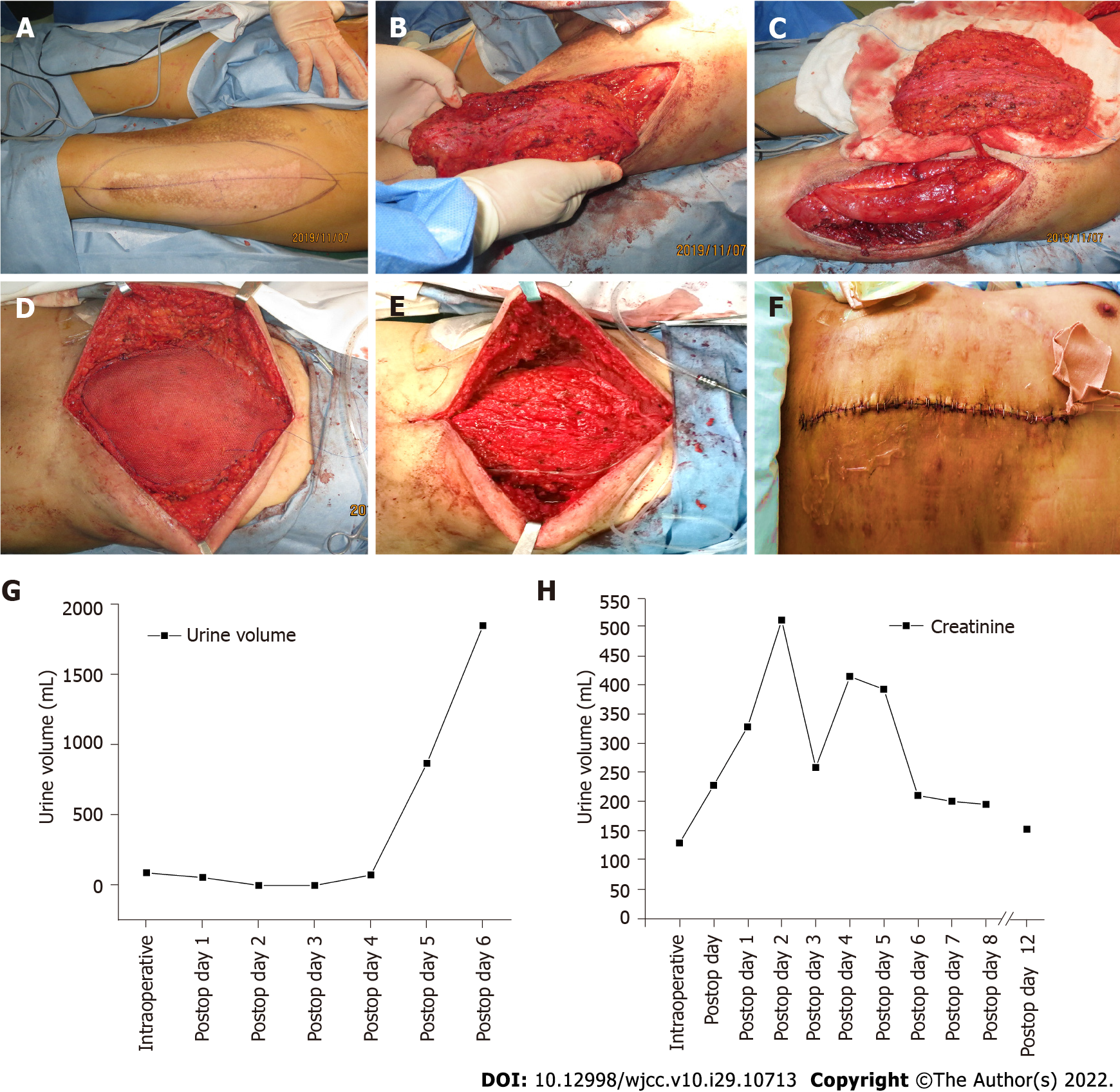
One-stage abdominal reconstruction was unfeasible due to the patient’s comorbidities and poor condition. The colostomy stoma may increase the risk of infection. Therefore, we carefully removed the grafted skin. The area of LAWD was 21 cm × 22 cm after the removal of the grafted skin. The operation duration was prolonged to 5.5 h due to the large area of severe adhesion between the grafted skin and viscera. Oliguria (urine volume < 90 mL) occurred during surgery owing to the mononephrous dysfunction, right renal pelvis stone, and ureteral obstruction diagnosed by ultrasonography. To reduce operation duration and surgical risks, a temporary TRC of the defect was performed using the Tension Relief System (TRS, Top Closure® 1S 8 mm sets, IVT Medical Limited, Israel). Briefly, seven pairs of attachment plates were placed 2 cm away from the wound edges and anchored with 3-0 silk sutures (Mersilk, Ethicon, United States) and staples (PROXIMATE, Ethicon, United States). Incremental approximation of wound edges was archived by pulling the bridging approximation straps through a lock/release ratchet mechanism (Figure 1). The patient developed hydronephrosis with a maximum blood creatinine level up to 511.3 μmol/L. He underwent hemofiltration dialysis and renal pelvis catheterization for 2 wk. The change in urine volume and creatinine is shown in Figure 2. The abdominal wound healed well without dehiscence or necrosis and TRS was removed 3 wk after installation.
Five months later, the patient underwent abdominal wall reconstruction with mesh reinforcement and a free anterolateral thigh (ALT) musculofascial flap to definitively repair his hernia (Figure 2). The original incision was reopened. Component separation was performed. The 15 cm × 20 cm peritoneal defect was repaired with a 20 cm × 20 cm hydrophilic mesh (Covidien, United States). The coverage ranged from the xiphoid and 2 cm inferior to the costal arch to 10 cm superior to the pubic symphysis vertically, and bilateral aponeurosis of external obliques horizontally. The mesh was secured with lock-stitch PDS II suturing. A 15 cm × 20 cm ATL musculofascial flap was elevated. The pedicle of descending branch of the lateral circumflex femoral artery was 14 cm. The microvascular anastomosis was performed on a branch of the superficial epigastric artery (Figure 2). The ALT flap was covered on the prosthetic mesh to repair the soft tissue defect (Figure 3).
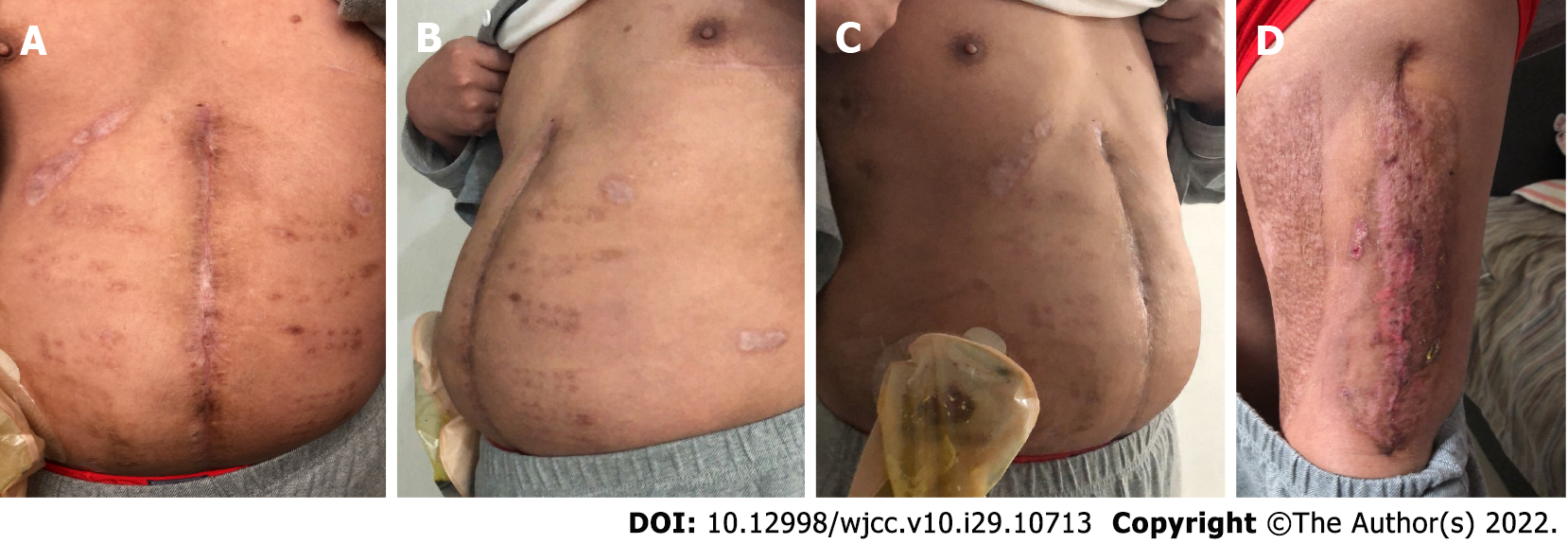
The patient was followed for 3 years. He recovered well and reported significant improvement in quality of life without signs of hernial recurrence (Figure 4).
Shotgun wounds, a high-energy firearm injury, often result in trauma contamination, extensive tissue contusions, and open injuries that make treatment difficult[6-8]. Current treatment principles regarding shotgun wounds include initial debridement followed by wound closure to prevent damage to deep tissue. However, closure of the wound should be delayed until 15 d in patients with more severe contamination[9]. Further treatment is feasible after the patient’s vital signs have stabilized. The case that we report had a temporary local trauma closure due to multiple shotgun wounds throughout the body, resulting in a LAWD, multiple organ damage, and poor general condition. For the further resolution of the abdominal wall hernia, he came to our department for treatment.
Many techniques for reconstruction of LAWD have been reported, but this is to date the first case of staged reconstruction with temporary TRC and definitive reconstruction with mesh and a flap. Gu et al[10] summarized the methods for abdominal wall reconstruction, including suture[11], prosthetic material[12], component separation technique[13], autologous tissue reconstruction[14], and abdominal wall expansion[15]. However, none of these methods could be used during the first reconstructive surgery owing to the patient’s poor conditions. Therefore, we used a commercial TRS for temporary abdominal closure[16].
The TRS was a novel method for large wound closure. Topaz et al[5] first introduced the use of TRS in 20 patients for preoperative skin stretching or intraoperative wound closure. Their study presented many cases who underwent TRS for larger defect closure after malignancy resection[17,18]. Dan et al[19] reported two cases of using TRS for wound closure of high-tension flap donor site following the harvest of deep inferior epigastric perforator flap and ALT flap. Choke et al[20] described their successful experience of using TSR and vacuum-assisted closure techniques for the treatment of extensive soft tissue defects in four patients. Similarly, Li et al[21] used a combined treatment with vacuum sealing drainage, TRS, and Ilizarov technique for traumatic hemipelvectomy in one case. The patient was able to ambulate and perform activities of daily life at the follow-up visit. Zhu et al[22] reported a 61-year-old man with bladder exstrophy who received primary closure of a large abdominal defect using TRS. In addition, a simulation study using finite element modeling by Katzengold et al[23] showed that the tensile stress generated by the TRS was only 4% of that generated by conventional sutures, suggesting that TRS significantly reduced local tissue deformations and stress concentrations during large wound closure. These studies have demonstrated that TRS reduced operative time, length of hospital stay, and costs, improved wound aesthetics, and minimized complications and obviated donor site morbidity caused by conventional skin grafting or flap reconstruction (Table 1).
| Ref. | Case no. | Age (yr) | Gender (male/female) | Cause of defect | Region of defect | Size of defect | Application time (prior to, during, and/or after surgery) | Closure (immediate/delayed closure) | Time to closure (min/d) |
| Topaz et al[5], 2012 | 1 | 62 | Male | SCC | Left distal leg | 3 cm × 2 cm | Prior to surgery | Delayed | 16 d |
| 2 | 52 | Female | Scar | Lower abdominal | 7 cm × 8 cm | Prior to surgery | Delayed | 11 d | |
| 3 | 26 | Male | High-voltage electric burn | Left lower limb | NA | During surgery | Immediate | NA | |
| 4 | 12 | Female | Congenital nevus | Right thigh | Φ = 2 cm | Prior to surgery | Delayed | 14 d | |
| 5 | 29 | Female | Infected surgical wound | Abdominal | NA | NA | Delayed | NA | |
| 6 | 88 | Female | SCC | Left distal leg | Φ = 2.5 cm | Prior to surgery | Delayed | 12 d | |
| Topaz et al[17], 2014 | 7 | 64 | Male | BCC | Parietal scalp | Φ = 3.5 cm | After surgery | Delayed | 5 d |
| 8 | 64 | Male | BCC | Parietal scalp | Φ = 3 cm | After surgery | Delayed | 1 d | |
| 9 | 74 | NA | SCC | Frontal scalp | Φ = 3 cm | During surgery | Immediate | NA | |
| 10 | 78 | NA | Ulcerated BCC | Occipital scalp | Φ = 3.2 cm | After surgery | Delayed | 5 d | |
| 11 | 17 | NA | Scar tissue neoplasia | Parietal scalp | Φ = 2.5 cm | After surgery | Delayed | 2 d | |
| 12 | 95 | Male | SCC | Occipital scalp | Φ = 4.5 cm | After surgery | Delayed | 17 d | |
| 13 | 82 | NA | SCC | Parietal scalp | Φ = 3.5 cm | After surgery | Delayed | 21 d | |
| 14 | 82 | NA | SCC | Occipital scalp | Φ = 3 cm | After surgery | Delayed | 2 d | |
| 15 | 65 | NA | SCC | Occipital scalp | Φ = 4 cm | After surgery | Delayed | 5 d | |
| Topaz et al[18], 2014 | 16 | 60 | Male | Basal cell carcinoma | Flank | 15 cm × 25 cm | During surgery | Immediate | 26 min |
| 17 | 35 | Male | Malignant melanoma | Scapular | 7 cm × 11.5 cm | During surgery | Immediate | 60 min | |
| 18 | 41 | Male | Spindle cell sarcoma | Supraclavicular | 26 cm × 25 cm | During surgery | Immediate | 135 min | |
| Dan et al[19], 2015 | 19 | 20 | Female | Tumor | Left groin | 10 cm × 8 cm | After surgery | Delayed | 28 d |
| 20 | 53 | Male | Traffic accident | Foot and ankle | 10 cm × 9 cm | After surgery | Delayed | 15 d | |
| Zhu et al[22], 2020 | 21 | 3 | Female | Infantile hemangiomas | Scalp | 6.5 cm × 5.2 cm | During surgery | Immediate | 20 min |
| Choke et al[20], 2017 | 22 | 42 | Male | Bacterial infection | Limb | 91 cm × 17 cm | After surgery | Delayed | 60 d |
| 23 | 55 | Male | Sternal osteomyelitis | Chest | 28 cm × 8 cm | After surgery | Delayed | 42 d | |
| 24 | 29 | Male | Hernia | Abdomen | 9 cm × 10 cm | After surgery | Delayed | 28 d | |
| Li et al[21], 2019 | 25 | 4 | Female | Traffic accident trauma | Pubic symphysis | 14 cm × 9 cm | After surgery | Delayed | NA |
There are several advantages of using TRS. First, TRS narrowed the width of the abdominal wall defect, thus reducing the flap area in the final abdominal reconstruction from 26 cm × 28 cm to 15 cm × 25 cm. Second, the operation time and associated risks were significantly reduced. The abdomen was successfully closed within 40 min using TRC, compared to hours of operation time for conventional reconstruction[24]. At the last follow-up, the patient reported satisfaction with his treatment owing to significant improvement in quality of life without signs of hernial recurrence.
The large full-thickness abdominal defect caused by a gunshot wound is often associated with infection, multiorgan injuries, and poor patient conditions. TRC is a useful method for the temporary closure of LAWD, particularly in cases in which one-stage abdominal wall reconstruction is unfeasible.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Musoni L, Morocco; Zharikov YO, Russia S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Muysoms F, Campanelli G, Champault GG, DeBeaux AC, Dietz UA, Jeekel J, Klinge U, Köckerling F, Mandala V, Montgomery A, Morales Conde S, Puppe F, Simmermacher RK, Śmietański M, Miserez M. EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia. 2012;16:239-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 206] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 2. | Alhan D, Şahin İ, Güzey S, Aykan A, Zor F, Öztürk S, Nışancı M, Özerhan İH. Staged repair of severe open abdomens due to high-energy gunshot injuries with early vacuum pack and delayed tissue expansion and dual-sided meshes. Ulus Travma Acil Cerrahi Derg. 2015;21:457-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Bulic K, Dzepina I, Mijatovic D, Unusic J. Prosthetic mesh for infected abdominal wall defects? J Plast Reconstr Aesthet Surg. 2008;61:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Wechselberger G, Schoeller T, Rainer C, Papp C. Temporary closure of full-thickness abdominal-wall defects with mesh grafts. Langenbecks Arch Surg. 1999;384:88-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Topaz M, Carmel NN, Silberman A, Li MS, Li YZ. The TopClosure® 3S System, for skin stretching and a secure wound closure. Eur J Plast Surg. 2012;35:533-543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Ordog GJ, Wasserberger J, Balasubramaniam S. Shotgun wound ballistics. J Trauma. 1988;28:624-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Bender JS, Hoekstra SM, Levison MA. Improving outcome from extremity shotgun injury. Am Surg. 1993;59:359-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Asensi V, Perciaccante A, Lippi D, Charlier P, Appenzeller O, Bianucci R, Donell S. Tudor military surgery and the management of Sir Martin Frobisher's gunshot wound: Comparison with current treatment. Injury. 2020;51:597-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Silva FE, Sorrentino BC. Selective conservative treatment for anterior abdominal gunshot: a literature narrative review. Rev Col Bras Cir. 2020;47:e20202523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Gu Y, Wang P, Li H, Tian W, Tang J. Chinese expert consensus on adult ventral abdominal wall defect repair and reconstruction. Am J Surg. 2021;222:86-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Kaufmann R, Halm JA, Eker HH, Klitsie PJ, Nieuwenhuizen J, van Geldere D, Simons MP, van der Harst E, van 't Riet M, van der Holt B, Kleinrensink GJ, Jeekel J, Lange JF. Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. Lancet. 2018;391:860-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 109] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 12. | Mathes T, Walgenbach M, Siegel R. Suture Versus Mesh Repair in Primary and Incisional Ventral Hernias: A Systematic Review and Meta-Analysis. World J Surg. 2016;40:826-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 13. | Tandon A, Pathak S, Lyons NJ, Nunes QM, Daniels IR, Smart NJ. Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. Br J Surg. 2016;103:1598-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 120] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 14. | Roubaud MS, Baumann DP. Flap Reconstruction of the Abdominal Wall. Semin Plast Surg. 2018;32:133-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Wooten KE, Ozturk CN, Ozturk C, Laub P, Aronoff N, Gurunluoglu R. Role of tissue expansion in abdominal wall reconstruction: A systematic evidence-based review. J Plast Reconstr Aesthet Surg. 2017;70:741-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Ribeiro Junior MA, Barros EA, de Carvalho SM, Nascimento VP, Cruvinel Neto J, Fonseca AZ. Open abdomen in gastrointestinal surgery: Which technique is the best for temporary closure during damage control? World J Gastrointest Surg. 2016;8:590-597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Topaz M, Carmel NN, Topaz G, Zilinsky I. A substitute for skin grafts, flaps, or internal tissue expanders in scalp defects following tumor ablative surgery. J Drugs Dermatol. 2014;13:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Topaz M, Carmel NN, Topaz G, Li M, Li YZ. Stress-relaxation and tension relief system for immediate primary closure of large and huge soft tissue defects: an old-new concept: new concept for direct closure of large defects. Medicine (Baltimore). 2014;93:e234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Dan X, Hongfei J, Huahui Z, Chunmao H, Hang H. A Skin-stretching Wound Closure System to Prevent and Manage Dehiscence of High-tension Flap Donor Sites: A Report of 2 Cases. Ostomy Wound Manage. 2015;61:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Choke A, Goh TL, Kang GC, Tan BK. Delayed primary closure of extensive wounds using the TopClosure system and topical negative pressure therapy. J Plast Reconstr Aesthet Surg. 2017;70:968-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Li J, Shi JB, Hong P, Wang YS, Ze HR, Lee RJ, Tang X. Combined treatment with vacuum sealing drainage, TopClosure device, and Ilizarov technique for traumatic hemipelvectomy: A rare case report of successful repairing of large-size soft tissue defects. Medicine (Baltimore). 2019;98:e14205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Zhu Z, Tong Y, Wu T, Zhao Y, Yu M, Topaz M. TopClosure® tension-relief system for immediate primary abdominal defect repair in an adult patient with bladder exstrophy. J Int Med Res. 2020;48:300060519891266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Katzengold R, Topaz M, Gefen A. Tissue loads applied by a novel medical device for closing large wounds. J Tissue Viability. 2016;25:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Patel NG, Ratanshi I, Buchel EW. The Best of Abdominal Wall Reconstruction. Plast Reconstr Surg. 2018;141:113e-136e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |