Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10695
Peer-review started: May 6, 2022
First decision: June 8, 2022
Revised: June 28, 2022
Accepted: September 1, 2022
Article in press: September 1, 2022
Published online: October 16, 2022
Processing time: 146 Days and 5.2 Hours
Here we report a rare case of submucosal esophageal abscess evolving into intr
An 80-year-old woman was admitted to our emergency department with a chief complaint of dysphagia and fever. Laboratory tests showed mild leukocytosis and elevated C-reactive protein level. Computed tomography showed thickening of the esophageal wall. Upper endoscopy showed a laceration of the esophageal mucosa and a submucosal mass. Spontaneous drainage occurred, and we could see purulent exudate from the crevasse. We closed the laceration with endoscopic clips. The patient did not remember swallowing a foreign body; however, she ate crabs before the symptoms occurred. We prescribed the patient with antibiotic, and the symptoms were gradually relieved. Two months later, upper endoscopy showed that the laceration was healed, and the submucosal abscess disappeared. However, intramural esophageal dissection was formed. We performed endo
In conclusion, we are the first to report the case of esophageal submucosal abscess evolving into intramural esophageal dissection. The significance of this case lies in clear presentation of the evolution process between two disorders. In addition, we recommend that endoscopic incision be considered as one of the routine therapeutic modalities of intramural esophageal dissection.
Core Tip: We are the first to report the case of esophageal submucosal abscess developing into intramural dissection. The significance of this case lies in clear presentation of the evolution process between two disorders, and we demonstrated that esophageal submucosal abscess is one of the etiologies of intramural esophageal dissection, which is a rare entity.
- Citation: Jiao Y, Sikong YH, Zhang AJ, Zuo XL, Gao PY, Ren QG, Li RY. Submucosal esophageal abscess evolving into intramural submucosal dissection: A case report. World J Clin Cases 2022; 10(29): 10695-10700
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10695.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10695
Esophageal submucosal abscess is an extremely rare disease caused by mucosal injury to the esophagus but without transmural perforation. It has been rarely reported[1-5]. Intramural esophageal dissection (IED) is also a rare disorder characterized by extensive laceration between the mucosal and submucosal layers of the esophageal wall. Herein, we report a rare case of submucosal esophageal abscess evolving into intramural submucosal dissection.
An 80-year-old woman was admitted to our emergency department with a chief complaint of dysphagia and fever for 14 d.
She also had a sore throat.
She had hypertension and type 2 diabetes.
No special notes.
On examination, the patient was febrile and tachycardiac.
Laboratory tests showed mild leukocytosis and an elevated C-reactive protein level.
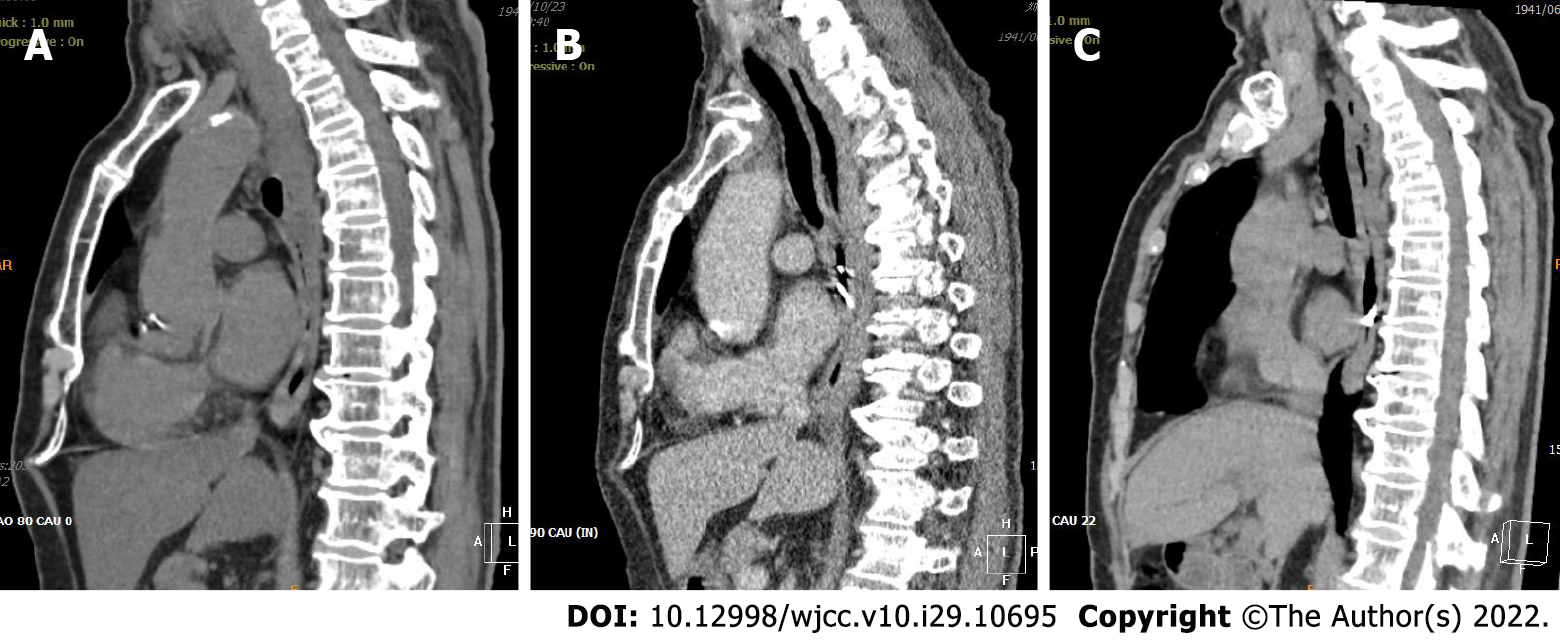
Chest computed tomography showed eccentric thickening of the esophageal wall.
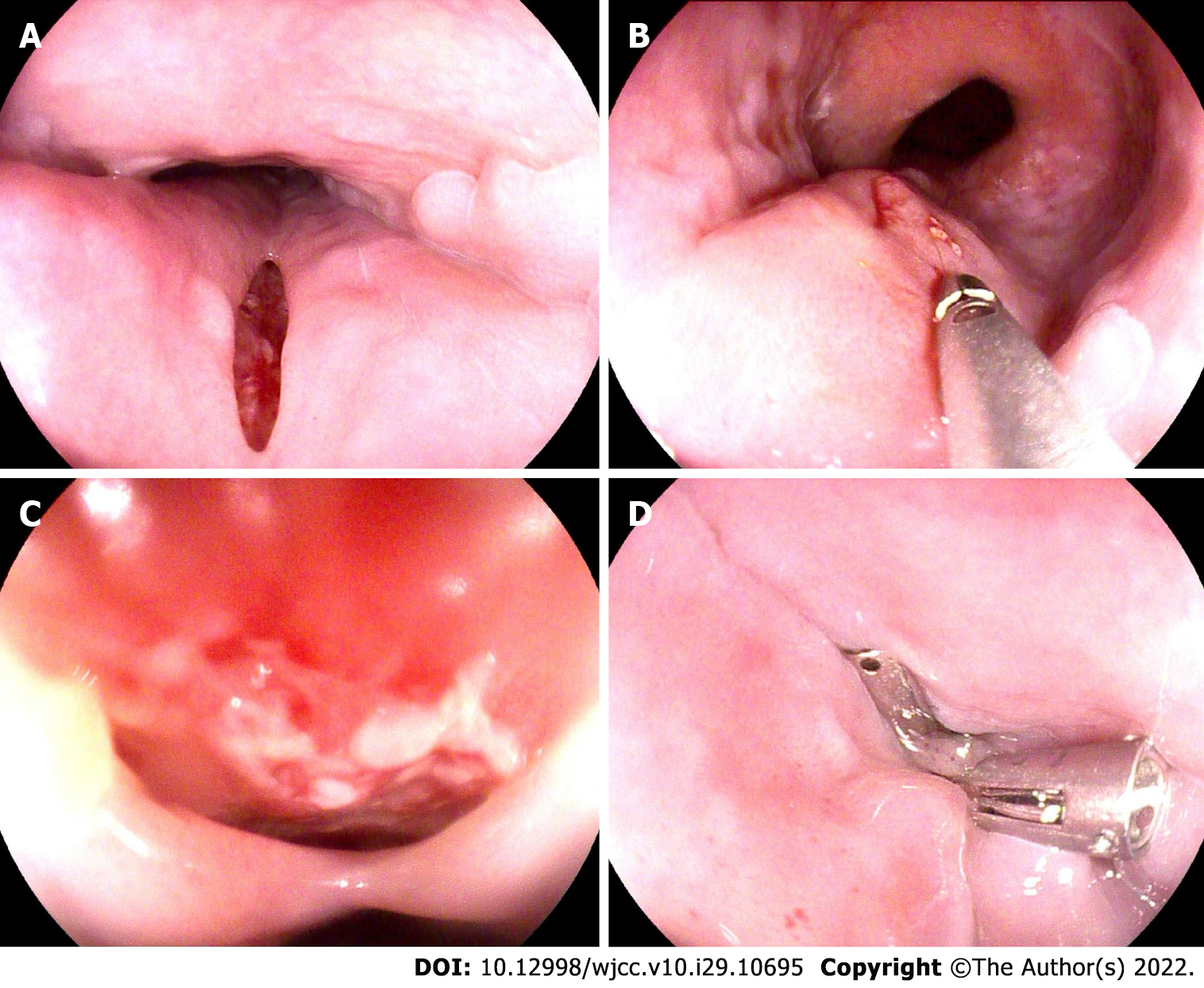
Esophageal carcinoma was our first consideration. To confirm this diagnosis, we performed upper endoscopy, which showed a laceration of the esophageal mucosa 30 cm distal to the incisors and a submucosal mass right above the esophagogastric junction. Spontaneous drainage of the submucosal mass occurred, and we could see purulent exudate from the crevasse. Therefore, the diagnosis of esophageal submucosal abscess was made.
We closed the laceration above the mass with metal endoscopic clips (Figure 1). The patient did not remember swallowing any foreign bodies, but she had eaten crabs before the symptoms occurred. Therefore, we presumed that she might have unintentionally swallowed some crab shell, which caused the laceration of the esophagus. We performed contrast-enhanced chest computed tomography after the endoscopy and found that the thickening of the esophageal wall was worse than before. We prescribed the patient a broad-spectrum antibiotic (sulperazone), and the dysphagia and fever were gradually relieved.
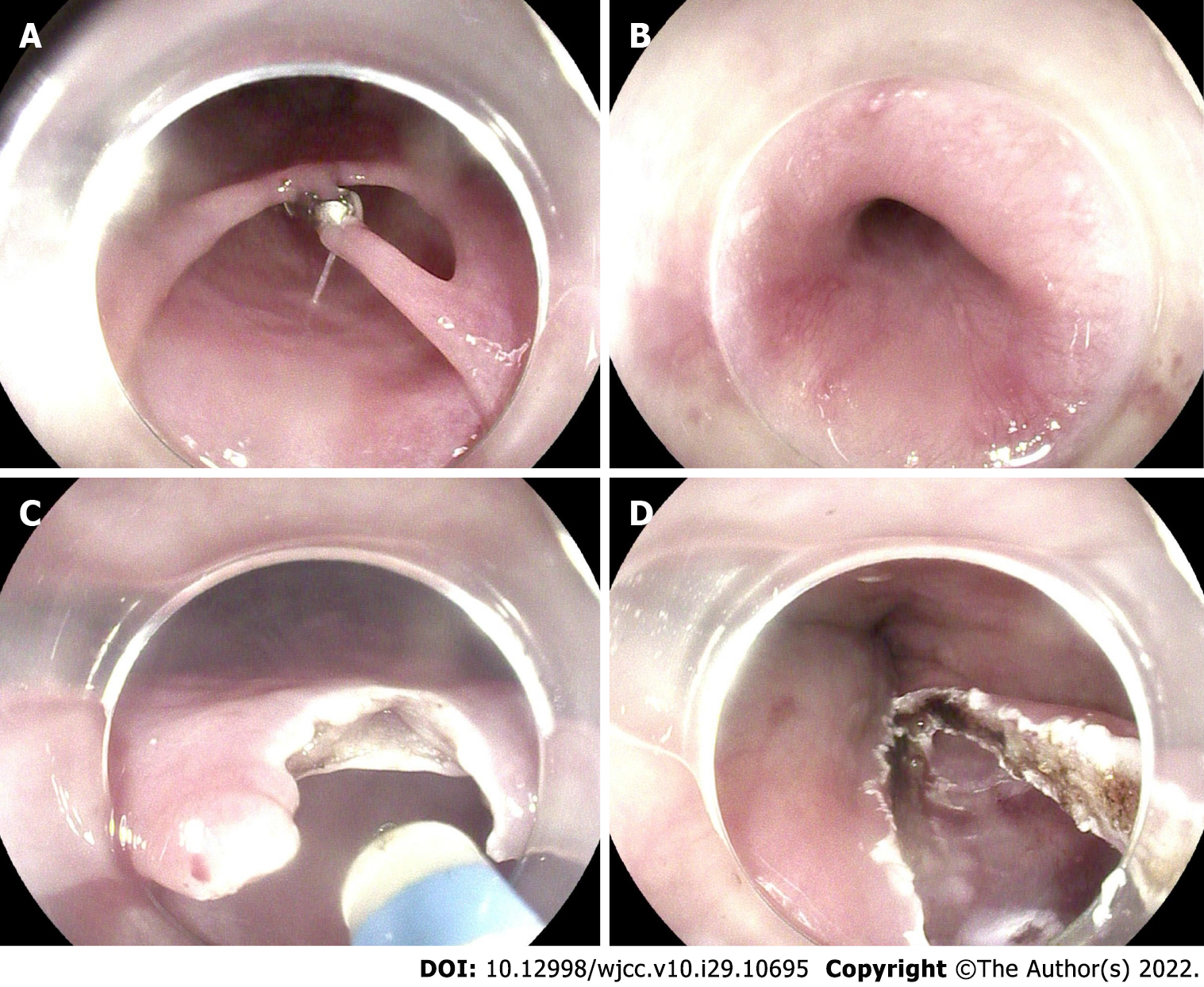
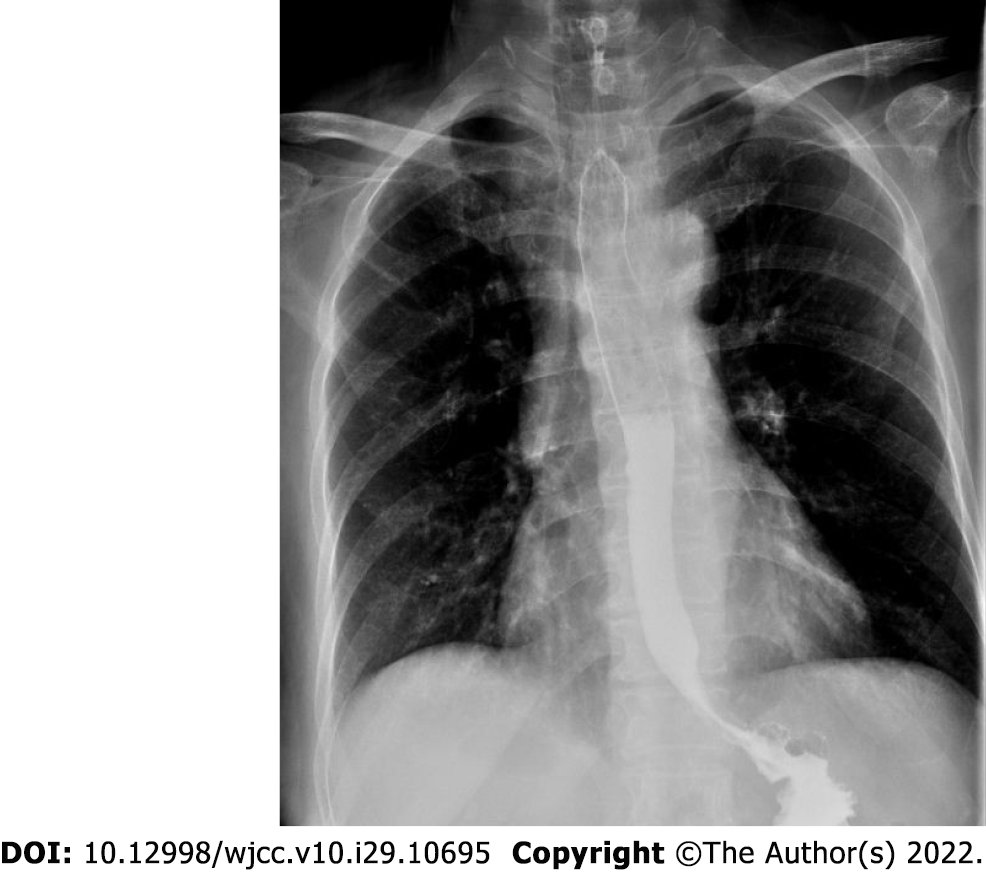
Two months later, we performed chest computed tomography and upper endoscopy again. Computed tomography showed a double-barreled esophagus without thickening of the esophageal wall (Figure 2). Upper endoscopy showed that the laceration had healed, and the submucosal abscess had disappeared. However, an IED formed. Endoscopic incision of the septum between two lumens was performed using a dual-knife process (Olympus, Tokyo, KD650L) with diathermy (Figure 3). An esophagogram taken 3 d after endoscopic incision showed that the barium could pass smoothly through the esophagus, and the dissection had disappeared (Figure 4).
Esophageal submucosal abscess is an extremely rare disease caused by mucosal injury to the esophagus but without transmural perforation, which has been reported in very few cases[1-5]. They are often caused by tuberculosis, fish bones, piriform sinus fistulae, and peritonsillar abscesses. In our case, the patient had unintentionally swallowed a foreign body that injured the esophageal mucosa and caused subsequent submucosal abscess.
In the present patient, the diagnoses of esophageal submucosal abscess and IED were both made by endoscopy and computed tomography. This case is quite unique in that spontaneous rupture of the abscess occurred, which allowed sufficient drainage. Although the submucosal abscess was cured with broad-spectrum antibiotics, an intramural dissection formed after 2 mo. This case is the first to allow any research team to witness the entire development of the condition as it transitioned from esophageal submucosal abscess to IED. This rare type of IED was confirmed to be the result of a submucosal abscess, establishing that esophageal submucosal abscess is one of the etiologies of IED.
IED is a rare disorder characterized by extensive laceration between the mucosal and submucosal layers of the esophageal wall. It was first reported by Marks and Keet in 1968[6]. The pathogenesis of IED remains unclear, however two theories have been proposed. The first theory postulates that intramural dissection from submucosal bleeding secondarily tears the mucosa, decompressing the hematoma into the esophageal lumen[7]. The second presumes that the mucosa tears first, with secondary dissection of the submucosa[8]. In rare cases[9], IED is considered to be the result of an intramural abscess caused by a foreign body, as in our patient.
Most teams choose to treat IED with conservative management because of its good prognosis. It is recommended that the patient’s regimen should include parenteral nutrition and fasting[10], and reports state that symptoms usually resolve after several days. Surgical treatment is rarely necessary[9]. In our case, the patient was senile and had diabetes mellitus, which rendered her susceptible to various infections. Thus, to avoid food retention and secondary infection, we performed endoscopic incision of the septum with a needle-knife. This endoscopic procedure has been proven to be simple and effective in several cases[11-13]. In rare cases, IED has been treated with self-expandable metal stents and endoscopic dilation[14,15]. Given its safety and effectiveness, we highly recommend endoscopic incision as a routine therapeutic modality for IED.
In conclusion, we are the first to report a case of esophageal submucosal abscess developing into intramural dissection. The significance of this case lies in clear presentation of the evolutionary transition between two disorders. We found endoscopic incision of the septum to be a viable therapeutic option for IED.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kohno S, Japan; Zhang X, United States S-Editor: Liu JH L-Editor: Filipodia P-Editor: Liu JH
| 1. | Inoue M, Okamoto K, Nagao H, Toyoda K. A Case of Esophageal Submucosal Abscess Originating from a Peritonsillar Abscess. Nihon Jibiinkoka Gakkai Kaiho. 2016;119:962-966. [PubMed] |
| 2. | Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, Yilmaz O, Gürsan N. Esophageal tuberculosis abscess: an unusual cause of dysphagia. Dis Esophagus. 2002;15:93-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Lee KH, Kim HJ, Kim KH, Kim HG. Esophageal tuberculosis manifesting as submucosal abscess. AJR Am J Roentgenol. 2003;180:1482-1483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Takeno S, Moroga T, Ono K, Kawahara K, Hirano T, Moriyama M, Suzuki M, Maki K, Yamana I, Hashimoto T, Shibata R, Naito M, Shiwaku H, Sasaki T, Yoshida Y, Yamashita Y. Endoscopic mucosal incision for successful treatment of submucosal abscess extending the full length of the esophagus due to fish bone: report of a case. Esophagus 2015; 12: 199–202. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Koyama S, Fujiwara K, Morisaki T, Fukuhara T, Kawamoto K, Kitano H, Takeuchi H. Submucosal Abscess of the Esophagus Caused by Piriform Sinus Fistula Treated with Transoral Video Laryngoscopic Surgery. ORL J Otorhinolaryngol Relat Spec. 2016;78:252-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Marks IN, Keet AD. Intramural rupture of the oesophagus. Br Med J. 1968;3:536-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Shay SS, Berendson RA, Johnson LF. Esophageal hematoma. Four new cases, a review, and proposed etiology. Dig Dis Sci. 1981;26:1019-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 49] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Phan GQ, Heitmiller RF. Intramural esophageal dissection. Ann Thorac Surg. 1997;63:1785-1786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Hanson JM, Neilson D, Pettit SH. Intramural oesophageal dissection. Thorax. 1991;46:524-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Barone JE, Robilotti JG, Comer JV. Conservative treatment of spontaneous intramural perforation (or intramural hematoma) of the esophagus. Am J Gastroenterol. 1980;74:165-167. [PubMed] |
| 11. | Ooi M, Norton I. Spontaneous intramural esophageal dissection successfully treated by endoscopic needle-knife incision. Gastrointest Endosc. 2016;84:195-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Cho CM, Ha SS, Tak WY, Kweon YO, Kim SK, Choi YH, Chung JM. Endoscopic incision of a septum in a case of spontaneous intramural dissection of the esophagus. J Clin Gastroenterol. 2002;35:387-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Murata N, Kuroda T, Fujino S, Murata M, Takagi S, Seki M. Submucosal dissection of the esophagus: a case report. Endoscopy. 1991;23:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Fischer A, Höppner J, Richter-Schrag HJ. First successful treatment of a circumferential intramural esophageal dissection with perforation in a patient with eosinophilic esophagitis using a partially covered self-expandable metal stent. J Laparoendosc Adv Surg Tech A. 2015;25:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Gluck M, Jiranek GC, Low DE, Kozarek RA. Spontaneous intramural rupture of the esophagus: clinical presentation and endoscopic findings. Gastrointest Endosc. 2002;56:134-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |