Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9904
Peer-review started: May 12, 2022
First decision: June 16, 2022
Revised: June 22, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: September 26, 2022
Processing time: 126 Days and 22.2 Hours
Dental extraction is a common operation in oral surgery and is usually accompanied by pain, swelling, and local infection. The application of high-speed air turbines increases the comfort of alveolar surgery and makes it more minimally-invasive. However, high-speed gas can enter the subcutaneous tissue of the face and neck or even the chest and mediastinum, which is a serious iatrogenic complication.
We describe two cases of severe subcutaneous and mediastinal emphysema caused by high-speed turbine splitting during dental extraction. The first case involved a 34-year-old man who complained of swelling of the face, mild chest tightness, and chest pain after dental extraction. Computed tomography (CT) scan showed a large amount of gas in the neck, chest wall, and mediastinum. The second case involved a 54-year-old woman who complained of swelling and pain of the neck after dental extraction. CT showed a large amount of gas collected in the neck and mediastinum. Both of them used high-speed turbine splitting during dental extraction.
High-speed turbine splitting during dental extraction may lead to severe subcutaneous and mediastinal emphysema. Dentists should carefully operate to avoid emphysema. If emphysema occurs, CT can be used to improve the diagnosis. The patient should be informed, and the complications dealt with carefully.
Core Tip: Facial and neck emphysema, especially with mediastinal emphysema, is rare complication in dental treatment. Iatrogenic subcutaneous emphysema is associated with the use of high-speed turbines. Here, we reported two cases of pneumomediastinum and subcutaneous emphysema secondary to dental extraction. We want to caution the dentists to be carefully to avoid the emphysema in the dental operate.
- Citation: Ye LY, Wang LF, Gao JX. Pneumomediastinum and subcutaneous emphysema secondary to dental extraction: Two case reports. World J Clin Cases 2022; 10(27): 9904-9910
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9904.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9904
Subcutaneous and mediastinal emphysema are common complications associated with surgeries, trauma, or infection in the head and neck region[1]. But it is a rare clinical entity in dental treatment. Although emphysema is common in clinical practice with the application of high-speed turbines in dental treatment, it is rarely reported in the mediastinum[2-4]. The number of cases reported pneumomediastinum after dental procedure is extremely low in the literature since 1968[5-7]. Most of them occurred after dental extraction. The use of a high-speed dental drill may introduce air into the soft tissue and lead to subcutaneous emphysema and pneumomediastinum. This type of emphysema involves the interstitial space of the face and neck, and enters the mediastinum through the anterior cervical muscle space, which is more serious than subcutaneous emphysema, and must be properly treated to prevent infection[8,9]. Physicians in the emergency department may misdiagnose the symptoms as an allergic reaction. We reported the two cases for waring physicians and dentists to be aware of the potential life-threatening complications of subcutaneous and mediastinal emphysema during dental extraction and deal with it carefully.
Case 1: A 34-year-old man was admitted for swelling and pain in the right lower jaw after extraction of the left mandibular third molar by a high-speed turbine.
Case 2: A 54-year-old woman presented at the ED owing to swelling of the suffered swelling and pain of the neck, mild chest tightness, and chest pain of six hours’ duration.
Case 1: The patient went to the department for extraction of the left mandibular third molar. Physical examination showed that the right mandibular third molar was a horizontally impacted tooth with some crown exposed. The patient was given local anesthesia with 5 mL lidocaine, and an air-turbine dental drill was used for resection of his tooth before extraction by a high-speed turbine. About 30 s into the operation, the patient complained of swelling of the face, tightness in the chest and a feeling of “bubble wrap” under the skin of the neck. Then, the patient was admitted to the emergency department.
Case 2: The patient was admitted because of swelling and pain of the neck. Six hours prior to the admission, the patient had undergone extraction of the left mandibular third molar by a high-speed turbine in a dental clinic and suffered swelling and pain of the neck. Neither the dentist nor her assistant had seen a similar case previously, and they recommended the patient go to the emergency department (ED) for treatment.
Case 1: The patient had no history of chronic diseases, anaphylaxis, or drug use. He did not smoke, and drank alcohol only occasionally (2-3 times a week). He denied trauma or vomiting.
Case 2: The patient had no history of chronic diseases, anaphylaxis, or drug use. She did not smoke or drink and denied trauma or vomiting.
Case 1: His temperature was normal, respiration was 20 breaths/min, oxygen saturation was 98% in air, blood pressure was 135/80 mmHg, and pulse rate was 89 beats/min. Physicalexamination showed swelling in the right side of the suborbital area, posterior ear, and buccal and supraclavicular fossa. Subcutaneous emphysema with crepitation upon palpation of the right buccal, submandibular, and anterior triangle of the neck.
Case 2: The temperature of the patient was normal. And her respiration was 17 breaths/min, oxygen saturation was 99% in air, blood pressure was 129/78 mmHg, and pulse rate was 77 beats/min. Physical examination showed swelling in buccal, posterior ear, the neck area and supraclavicular fossa. The fresh wound due to the dental extraction had no obvious bleeding. The trachea was midline, and she phonated normally.
Case 1: The results of routine blood tests on admission indicates inflammation with an elevated hypersensitive C-reactive protein of 15.1 mg/L (normal range: 0-10 mg/L) and 84.5% proportion of neutrophil classification (normal range: 40%-75%). No abnormalities were found in biochemical tests.
Case 2: The results of routine blood tests on admission indicates inflammation with an elevated hypersensitive C-reactive protein of 13.1 mg/L (normal range: 0-10 mg/L) and 79.5% proportion of neutrophil classification (normal range: 40%-75%). The results of biochemical tests on admission were normal.
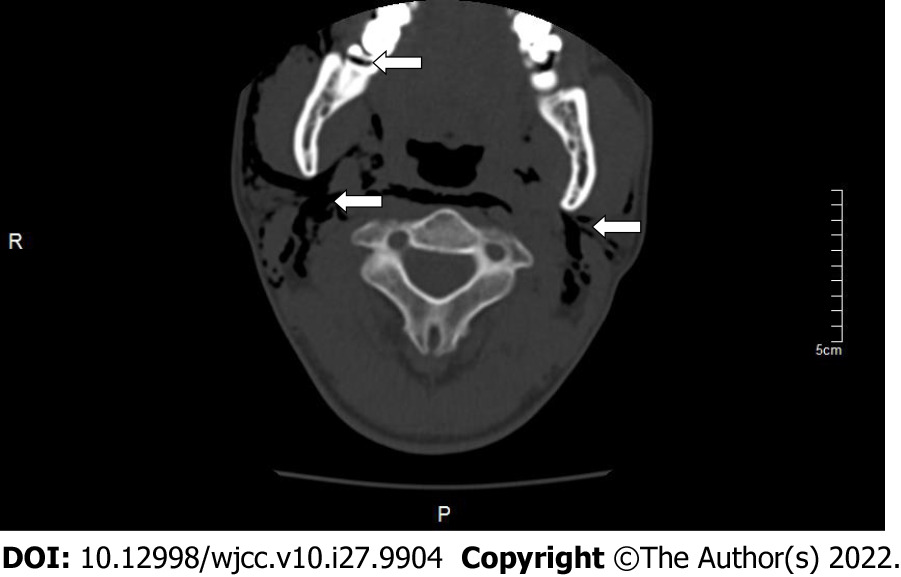
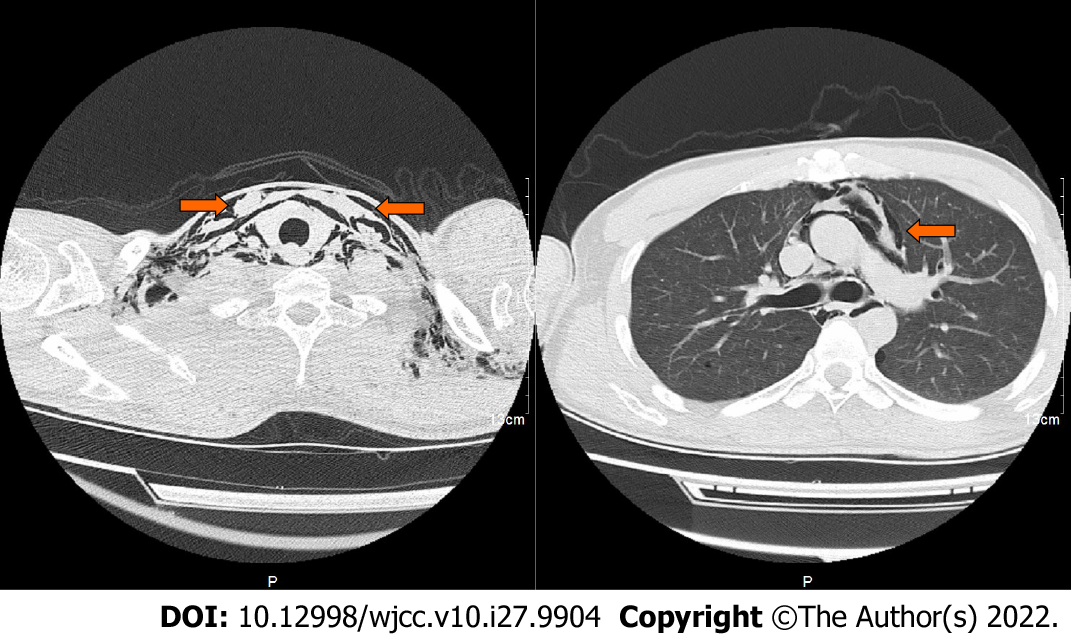
Case 1: Computed tomography (CT) showed a large amount of gas in the neck, chest wall, and mediastinum (Figures 1 and 2).
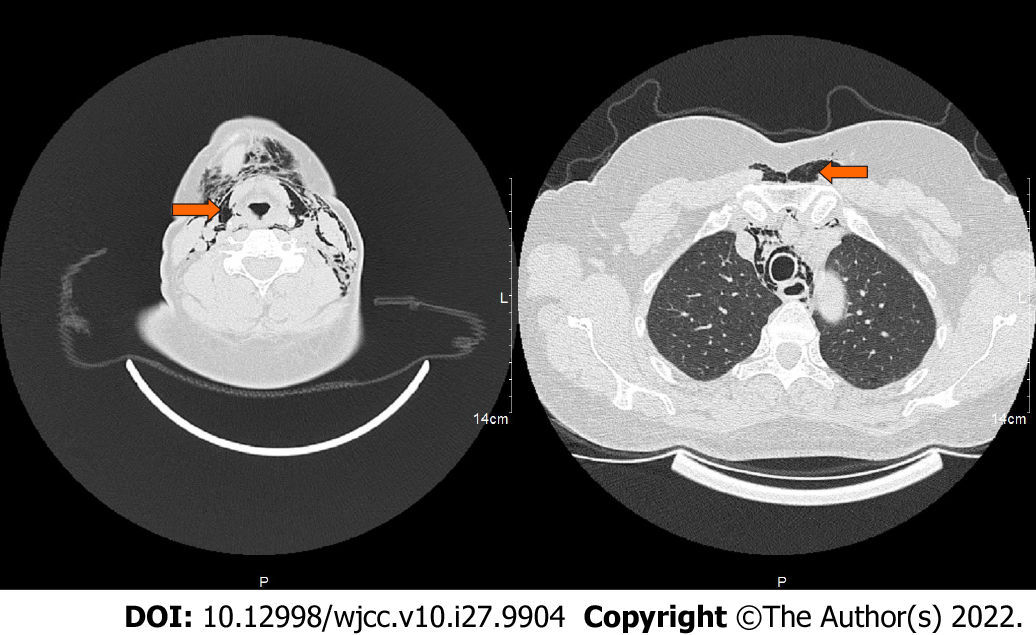
Case 2: CT showed a large amount of gas collected in the neck and mediastinum (Figures 3 and 4).
Pneumomediastinum and subcutaneous emphysema.
In order to avoid mediastinitis, piperacillin-tazobactam was initiated prophylactically to the patients with the recommendation of the department of infectious diseases. Both patients were administered with Metronidazole 200 mg and 4.5 g piperacillin-tazobactam thrice a day for three days.
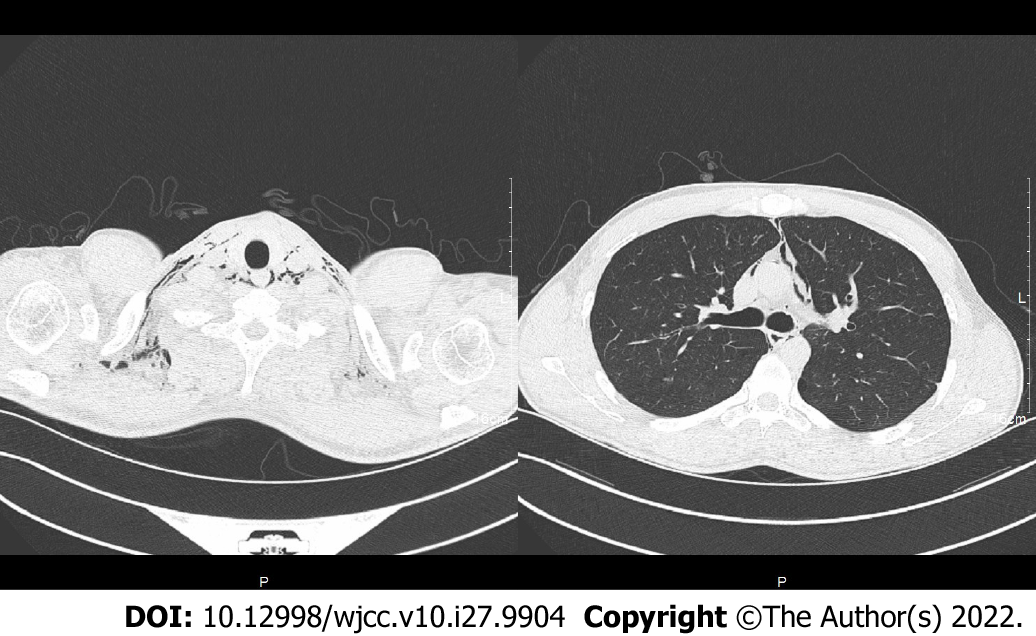
Case 1: The patient was followed radiographically with neck and thorax CT one week later. The radiologic findings were almost completely regressed (Figure 5). During the follow-up and treatment, there was no negative development in favor of mediastinitis (hypersensitive C-reactive protein was 1.9 mg/L; normal range: 0-10 mg/L) and the patient was discharged on the seventh day.
Case 2: The patient was admitted for observation and discharged after treatment with antibiotics for 3 d. The patient received a follow-up phone call one week after being discharged and reported complete resolution of symptoms.
Facial and neck emphysema, especially mediastinal emphysema, is very rare in dental treatment. The first case of subcutaneous emphysema associated with dental treatment was reported in 1900[10]. Since then, more cases related to the application of high-speed turbine in dental extraction. The first case of subcutaneous emphysema associated with dental treatment was reported in 1900[9,11,12], prosthodontics[13], root canal therapy or dental laser cooling[11], and periodontal treatment[14] with self-limited emphysema have bene reported. According to our patients’ medical histories and physical examination, it was easy to diagnose the subcutaneous emphysema associated with high-speed turbines[15]. High-speed turbines are the most commonly used tools for incising dental tissue, which is driven by compressed gas, and the high-speed airflow is a risk for subcutaneous emphysema. As reported, iatrogenic subcutaneous emphysema is associated with the use of high-speed turbines[16].
There is a space between the root of the mandibular molar and tongue, which is a common site for emphysema[17]. The compressed gas can enter the fascia of the neck through the oral barrier such as the periodontal membrane, and then spread from the submandibular and parapharyngeal space to the anterior cervical muscle space and mediastinum. If the cooling spray mixed with the tooth fragments enters into the maxillofacial space, patients may suffer from infection or even develop an abscess. In the first case, there was no flap operation and subcutaneous emphysema occurred about 30 s after the application of a high-speed turbine. In previous reports, emphysema occurred several hours after dental extraction[4,18]. The patient suffers a repeatedly infection with a narrow and deep blind pocket formed. When operated, the gas directly impacts into the soft tissue space. In the second case, buccal and lingual bone wall defects were detected, which formed a “bag” in the soft tissue. When operated, the gas entered into the “bag” and spread from the maxillofacial space to the mediastinum.
As reported, the differential diagnosis of patients with facial and neck swelling after dental extraction should include pneumothorax, hematoma, maxillofacial infection, allergic reaction, and angioedema. In some cases wherein the patient presents to the emergency room, doctors may consider esophageal perforation or allergic reactions, resulting in misdiagnosis[18,19]. For emergency doctors, examination of the vestibular groove swelling may contribute to the diagnosis of subcutaneous emphysema. Dentists should use and carry-out procedures with high-speed turbines for dental extraction very carefully. Patients should be advised of the possible complications before surgery, especially for low-position impacted teeth[20,21]. During the operation, aseptic procedures need to be strictly performed. When high-speed gas enters into a narrow surgical zone, early identification and appropriate treatment is key to preventing progression of a subcutaneous emphysema. Imaging examinations contribute to clarify the region of emphysema[22,23]. Oral microflora and fragmented tooth tissue can also enter the deep gaps; antibiotics are recommended in such cases[24,25].
As a complication of dental extraction, patients should be advised about emphysema before surgery. Dentists should carefully operate to avoid emphysema. in the event of subcutaneous emphysema, patients experience swelling to the face and neck with no obvious pain. If mediastinal emphysema occurs, patients may have difficulty breathing, hoarseness, and chest or back pain. CT contributes to better diagnosis of emphysema. In case emphysema occurs, the patient should be duly informed and the complications dealt with carefully.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chrcanovic BR, Sweden; Ghannam WM, Egypt S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Yoshimoto A, Mitamura Y, Nakamura H, Fujimura M. Acute dyspnea during dental extraction. Respiration. 2002;69:369-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | McKenzie WS, Rosenberg M. Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral Maxillofac Surg. 2009;67:1265-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 3. | Mishra L, Patnaik S, Patro S, Debnath N, Mishra S. Iatrogenic subcutaneous emphysema of endodontic origin - case report with literature review. J Clin Diagn Res. 2014;8:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Ferreira Simões A, Rodrigues JB, Úria S, Nunes da Silva G. [Subcutaneous Emphysema and Pneumomediastinum During a Tooth Extraction]. Acta Med Port. 2018;31:435-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Chen SC, Lin FY, Chang KJ. Subcutaneous emphysema and pneumomediastinum after dental extraction. Am J Emerg Med. 1999;17:678-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Erol G, Kubat E, Sicim H, Kadan M, Bolcal C. An unexpected complication of robotic cardiac surgery: Pneumomediastinum. J Saudi Heart Assoc. 2019;31:106-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Afzali N, Malek A, Attar AH. Cervicofacial emphysema and pneumomediastinum following dental extraction: case report. Iran J Pediatr. 2011;21:253-255. [PubMed] |
| 8. | Elia F, Laface B, Pagnozzi F, Boccuzzi A, Ferrari G, Perna M, Aprà F. Cervicofacial emphysema and pneumomediastinum complicating a dental procedure. J Emerg Med. 2013;45:e179-e181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Vargo RJ, Potluri A, Yeung AY, Aldojain A, Bilodeau EA. Cervicofacial subcutaneous emphysema: a clinical case and review of the literature. Gen Dent. 2016;64:68-71. [PubMed] |
| 10. | Turnbull A. A remarkable coincidence in dental surgery. Br Med J. 1900;1:1131. [RCA] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Mitsunaga S, Iwai T, Aoki N, Yamashita Y, Omura S, Matsui Y, Maegawa J, Hirota M, Mitsudo K, Tohnai I. Cervicofacial subcutaneous and mediastinal emphysema caused by air cooling spray of dental laser. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e13-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Yang SC, Chiu TH, Lin TJ, Chan HM. Subcutaneous emphysema and pneumomediastinum secondary to dental extraction: a case report and literature review. Kaohsiung J Med Sci. 2006;22:641-645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Jeong CH, Yoon S, Chung SW, Kim JY, Park KH, Huh JK. Subcutaneous emphysema related to dental procedures. J Korean Assoc Oral Maxillofac Surg. 2018;44:212-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Lee ST, Subu MG, Kwon TG. Emphysema following air-powder abrasive treatment for peri-implantitis. Maxillofac Plast Reconstr Surg. 2018;40:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Frühauf J, Weinke R, Pilger U, Kerl H, Müllegger RR. Soft tissue cervicofacial emphysema after dental treatment: report of 2 cases with emphasis on the differential diagnosis of angioedema. Arch Dermatol. 2005;141:1437-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Heyman SN, Babayof I. Emphysematous complications in dentistry, 1960-1993: an illustrative case and review of the literature. Quintessence Int. 1995;26:535-543. [PubMed] |
| 17. | Strassen U, Bas M, Knopf A. [Visit at the dentist with consequences]. HNO. 2011;59:1125-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Arai I, Aoki T, Yamazaki H, Ota Y, Kaneko A. Pneumomediastinum and subcutaneous emphysema after dental extraction detected incidentally by regular medical checkup: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e33-e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | An GK, Zats B, Kunin M. Orbital, mediastinal, and cervicofacial subcutaneous emphysema after endodontic retreatment of a mandibular premolar: a case report. J Endod. 2014;40:880-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Mozzati M, Gallesio G, Ullio L, Staiti G, Lucchina AG, Mortellaro C. Patient-based assessment of tooth extraction with ultrasonic dental surgery. J Craniofac Surg. 2014;25:2081-2083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Corrêa AP, Faverani LP, Ramalho-Ferreira G, Ferreira S, Ávila Souza F, de Oliveira Puttini I, Rangel Garcia-Júnior I. Unerupted lower third molar extractions and their risks for mandibular fracture. J Craniofac Surg. 2014;25:e228-e229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Nishimura T, Sawai T, Kadoi K, Yamada T, Yoshie N, Ueda T, Nakao A, Kotani J. Iatrogenic subcutaneous emphysema and pneumomediastinum following a high-speed air drill dental treatment procedure. Acute Med Surg. 2015;2:253-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Alonso V, García-Caballero L, Couto I, Diniz M, Diz P, Limeres J. Subcutaneous emphysema related to air-powder tooth polishing: a report of three cases. Aust Dent J. 2017;62:510-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Chen CH, Chang H, Liu HC, Hung TT, Huang WC. Pneumothorax, pneumomediastinum and pneumopericardium complications arising from a case of wisdom tooth extraction. Rev Port Pneumol. 2012;18:194-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Lococo F, Trabucco L, Leuzzi G, Salvo F, Paci M, Sgarbi G, Ferrari AM. Severe breathing and swallowing difficulties during routine restorative dentistry. Ann Ital Chir. 2015;86. [PubMed] |