Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9886
Peer-review started: May 5, 2022
First decision: June 16, 2022
Revised: June 25, 2022
Accepted: August 15, 2022
Article in press: August 15, 2022
Published online: September 26, 2022
Processing time: 134 Days and 3 Hours
An extra tooth in the normal tooth sequence in any region of the dental arch is regarded as a supernumerary tooth (SNT). Due to the large variation in location and morphology, the extraction of impacted SNTs is an extensive and complex procedure with high risks of several complications. This report presents a rare case of seven impacted SNTs in the bilateral upper and lower arch that were successfully extracted with the use of digital positioning guide plates.
In January 2022, a 21-year-old male was referred to our department with a chief complaint of pain in relation to tooth #36. Clinical examination showed a deep carious lesion with pulpal involvement in tooth #36 and lingual swelling of the bilateral mandibular posterior area. Radiographic examination revealed seven deeply impacted SNTs in the bilateral posterior area and bilateral impacted mandibular third molars. Based on these findings, the patient was diagnosed with bilateral, multiple impacted SNTs and tooth #36 chronic pulpitis. A root canal treatment and an all-ceramic crown restoration for tooth #36 were performed. An individualized digital positioning guide plate was designed by computer-aided design/computer-aided manufacturing technology and cone-beam computed tomography for extraction of the impacted SNTs. During the operation, the digital positioning guide plate allowed rapid positioning and exposure of the SNTs while avoiding adjacent important anatomical structures. At 3-month follow-up, regeneration of bone and soft tissues was visible.
The application of digital positioning guide plates is useful for the individualized and minimalized extraction of impacted supernumerary teeth.
Core Tip: We present a rare case of seven impacted supernumerary teeth (SNTs) in the bilateral maxilla and mandible extracted with the aid of digital positioning guide plates manufactured by computer-aided design/computer-aided manufacturing technology. The use of these convenient and practical digital positioning guide plates for SNT extraction can provide accurate positioning, reduce the surgical complexity, decrease the operation time and minimize the invasiveness of the procedure. The surgery can be performed under local anesthesia, broadening the application prospects of digital positioning guide plates in other outpatient programs.
- Citation: Wang Z, Zhao SY, He WS, Yu F, Shi SJ, Xia XL, Luo XX, Xiao YH. Application of digital positioning guide plates for the surgical extraction of multiple impacted supernumerary teeth: A case report and review of literature. World J Clin Cases 2022; 10(27): 9886-9896
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9886.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9886
Supernumerary teeth (SNTs) are one of the most frequently encountered developmental abnormalities in clinical practice. The prevalence of SNTs varies between 0.1% and 3.8%; they can occur in both the permanent and primary dentition, but mostly in the former[1]. In general, males are more likely to be affected than females, at a ratio of 2.3:1[1,2-4]. They can appear as single or multiple teeth that are erupted or impacted and located in either the maxilla or mandible[4]. Rare occurrences of SNTs in extraoral sites, such as the nasal cavity, have also been reported, while in the dental arch, there is a preference for the maxilla[5]. The most common SNTs are mesiodens[6] that form between the maxillary central incisors, followed by the maxillary and mandibular fourth molars, premolars, canines, and lateral incisors[1]. A single SNT is present in 76%-86% of patients, two are present in 12%-23%, and three or more are found in less than 1%[7,8]. However, it has been reported that multiple SNTs (more than five) often form in the mandibular premolar region[7]. Depending on the morphology of the SNTs, they can be classified as conical, tuberculate, supplemental, and odontoma[9]. The presence of SNTs may affect the spatial position of the normal teeth and often causes a series of complications, including the displacement of adjacent teeth, blocking eruption, root resorption, and odontogenic cysts[10]. Therefore, the identification and diagnosis of SNTs at an early stage are important to avoid these complications.
Because the impacted SNTs are close to the normal teeth and important anatomical structures, the adjacent tissues may be damaged during the surgical extraction procedure. Cone-beam computed tomography (CBCT) provides detailed spatial location information for impacted SNTs, thus allowing the surgeon to make an appropriate treatment plan, but the role of this visual information in the extraction procedure is limited[11-13]. Even though the surgeon can clarify the position of the impacted SNTs in relation to the adjacent teeth by CBCT, the extraction procedure is normally conducted by empirical manipulation, and problems such as the inability to accurately control surgical trauma, operative time, and postoperative complications often arise. In recent years, the applications of 3D-printing technology[14,15] and navigation systems[16-18] have facilitated minimally invasive alveolar surgery. Preoperative digital positioning guide plates based on the patient's CBCT and oral scan data can simplify the surgical operations and transfer preoperative planning more precisely to the intraoperative period, which may improve the precision of the operation thus reduce the deviation between the actual position and preoperative design[18]. The use of digital positioning guide plates during the tooth extraction procedure may increase the predictability of the surgery effect and reduce postoperative discomfort and complications for the patients[19]. However, few studies have reported the use of personalized guide plates for the extraction of complex SNTs[20].
Herein, we present a rare case of seven impacted SNTs in the bilateral upper and lower arch that were successfully extracted with the use of individualized digital positioning guide plates.
A 21-year-old male was referred to our department with a chief complaint of pain in relation to tooth #36.
The patient experienced slight pain, discomfort, and lingual swelling of the bilateral mandibular premolar and molar area 4 mo prior. The patient took an anti-inflammatory drug and felt that the pain had decreased but could not recall the type and dose of the drug. During the prior month, the pain recurred.
The patient had no significant dental history.
Not mentioned.
Clinical examination revealed a deep carious lesion with pulpal involvement in tooth #36 and lingual swelling of the bilateral mandibular premolar and molar area. The facial appearance was normal and presented with no skeletal or other abnormalities suggestive of any syndrome.
There were no laboratory examinations.
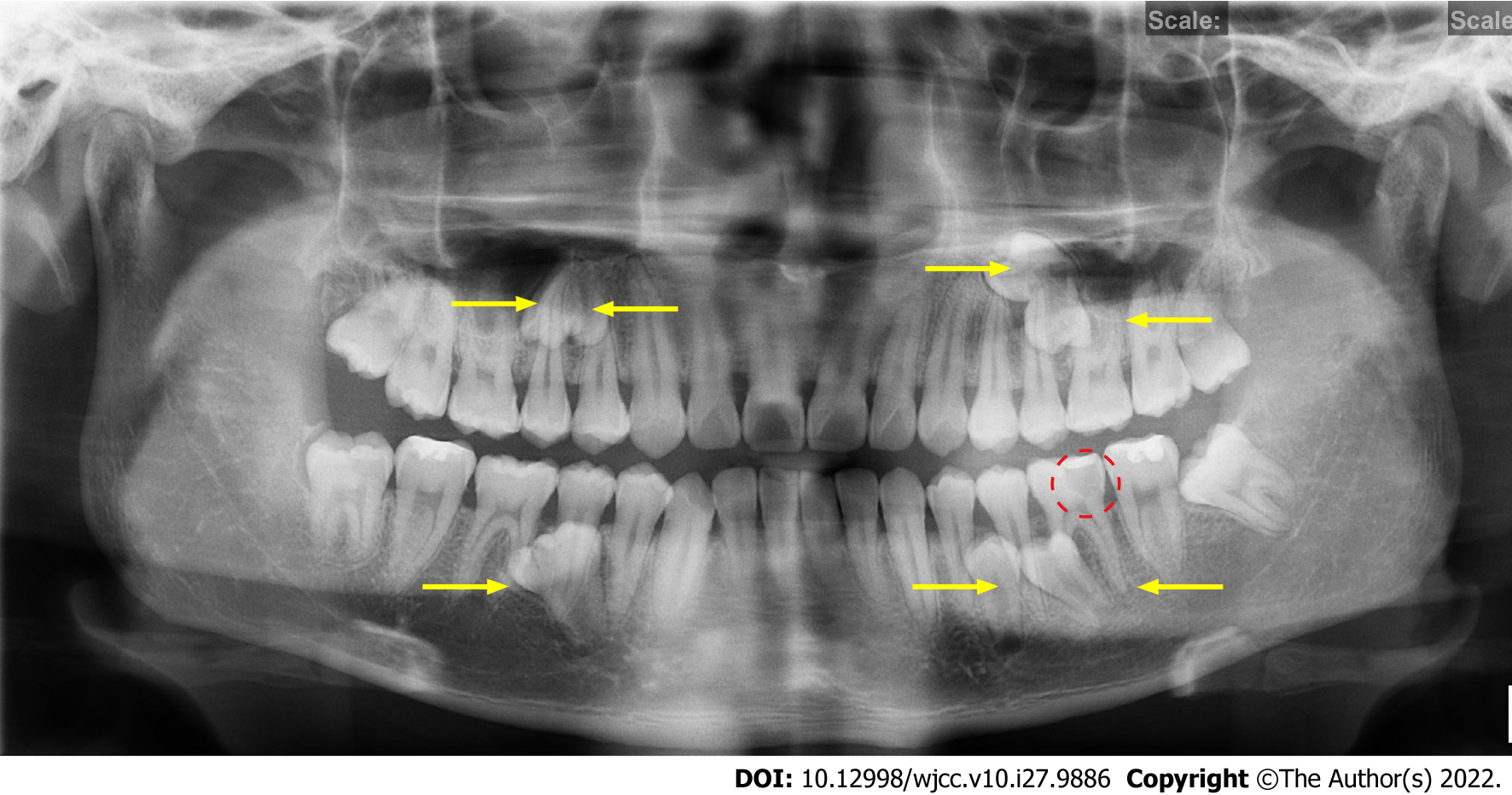
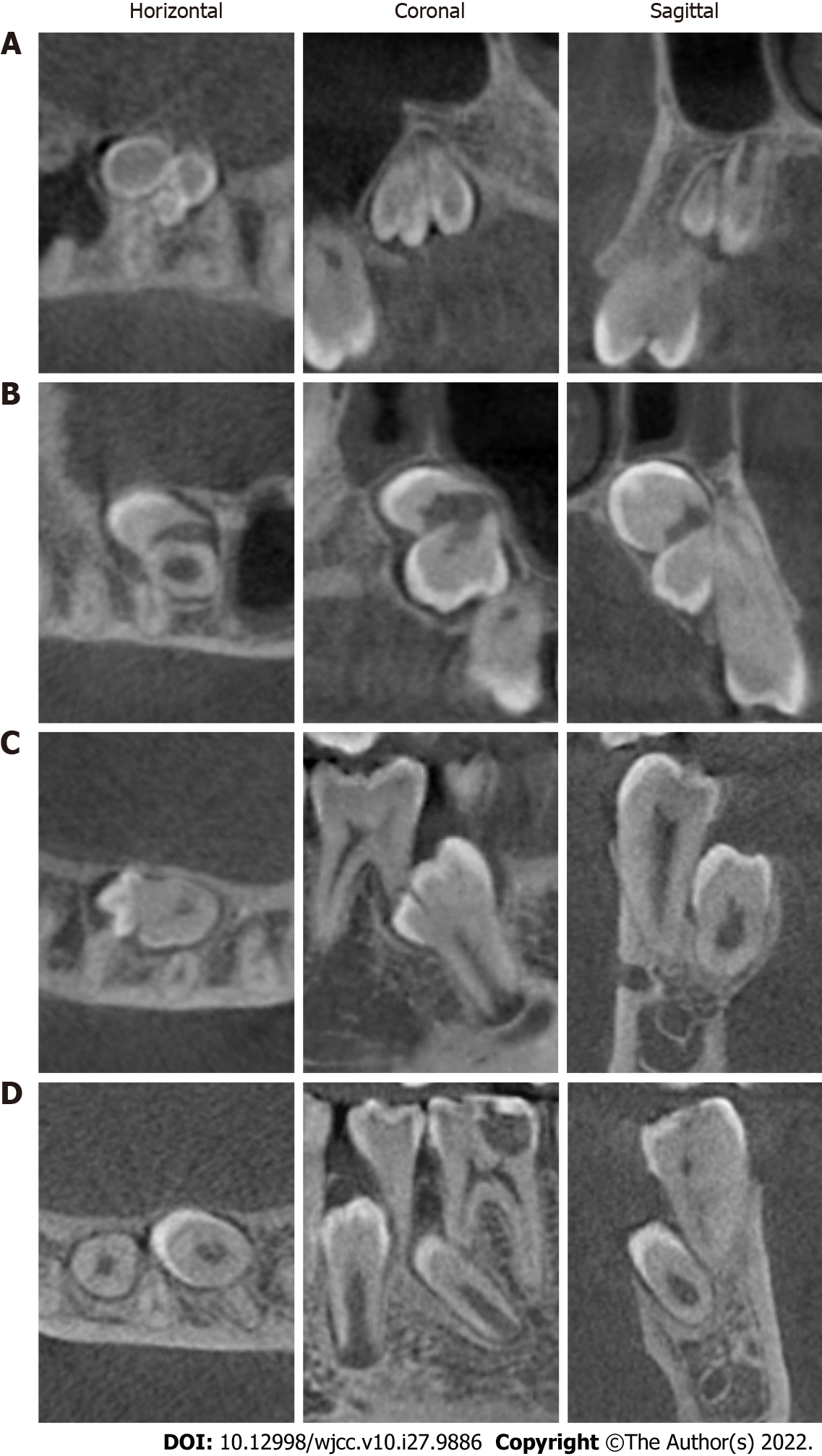
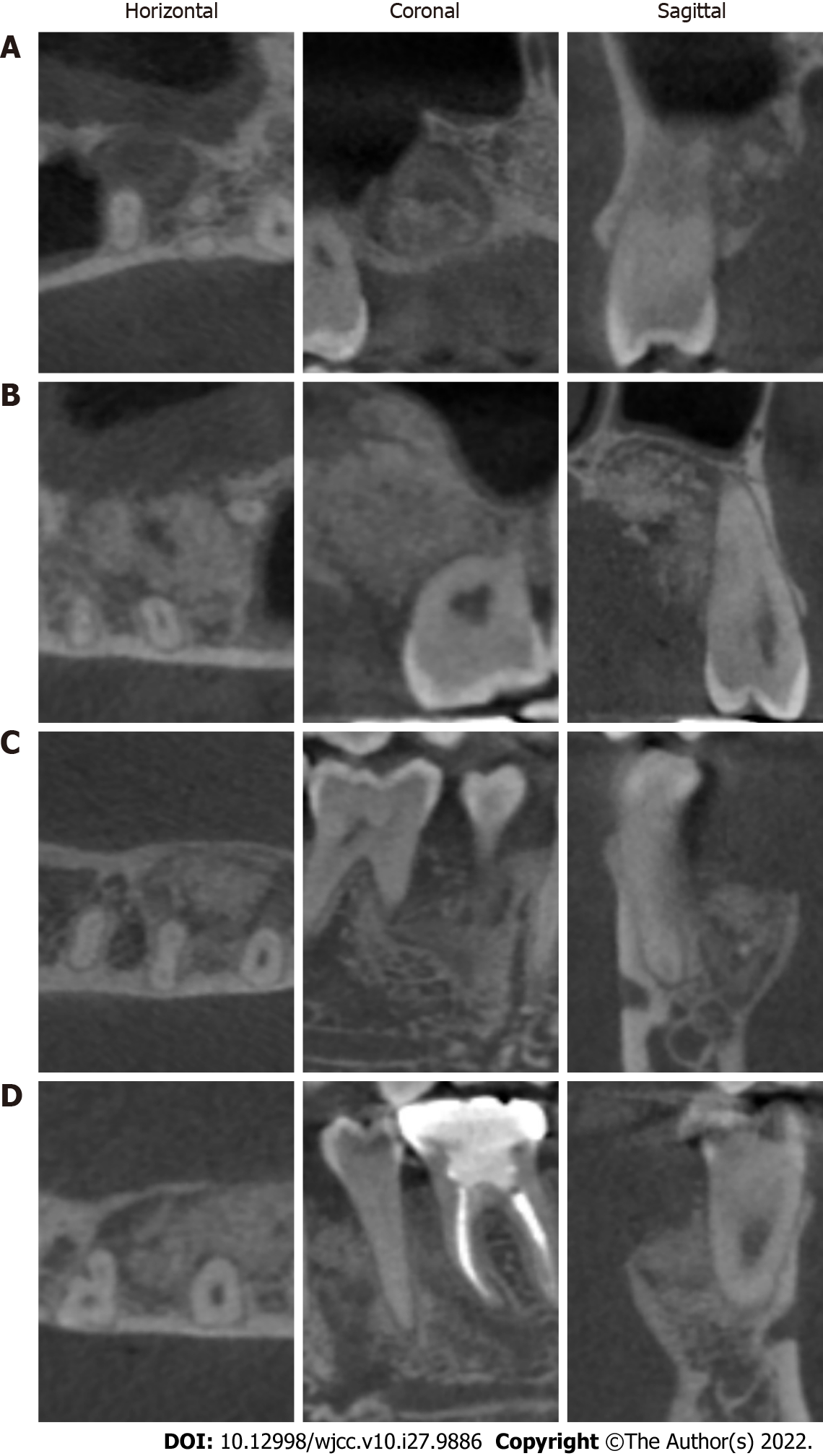
The panoramic radiograph (Figure 1) showed seven bilateral deeply impacted SNTs in the premolar and molar area without any displacement of the permanent teeth and a local low-density area close to the pulp cavity in tooth #36. In addition, there were two impacted mandibular third molars. CBCT imaging (Figure 2) showed the seven impacted SNTs relative to the maxillary sinus floor, inferior alveolar nerve and the adjacent permanent teeth root. In the maxilla, four of the impacted SNTs, which resembled conical-shaped crowns, were present in the palatal regions of the bilateral premolars and molars. Furthermore, a slight resorption of the palatal bone plate was present in these regions. The other three impacted SNTs, which resembled supplemental premolars, were located in the bilateral mandibular premolar and molar area. In addition, there were two impacted mandibular third molars.
Accordingly, the patient was diagnosed with chronic pulpitis of tooth #36, bilateral, multiple impacted SNTs and bilateral impacted mandibular third molars.
The patient’s intervention complied with the requirements of the Declaration of Helsinki. The patient was informed of the unpredicted situation.
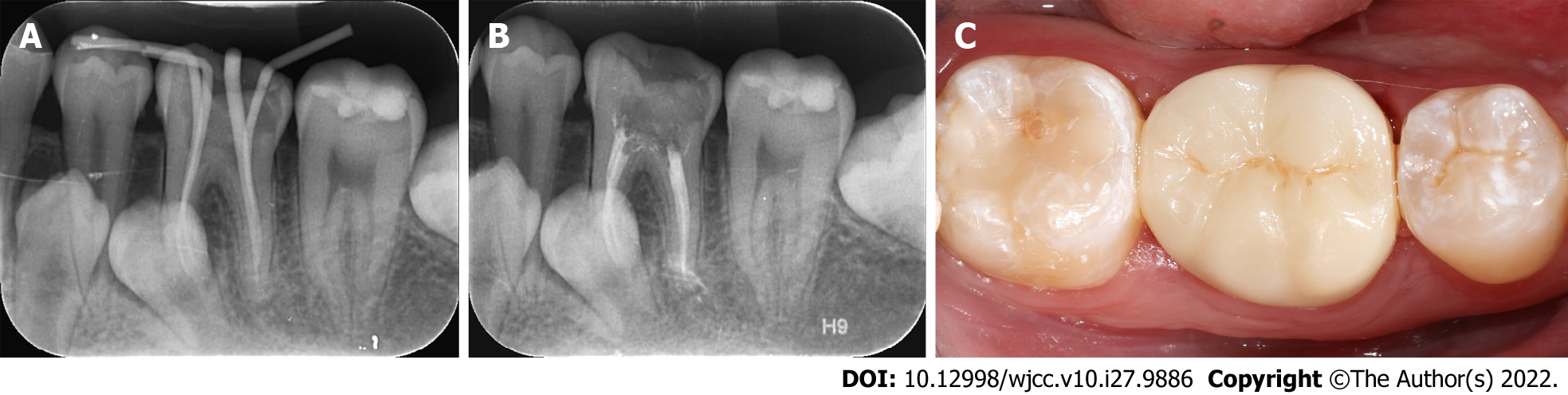
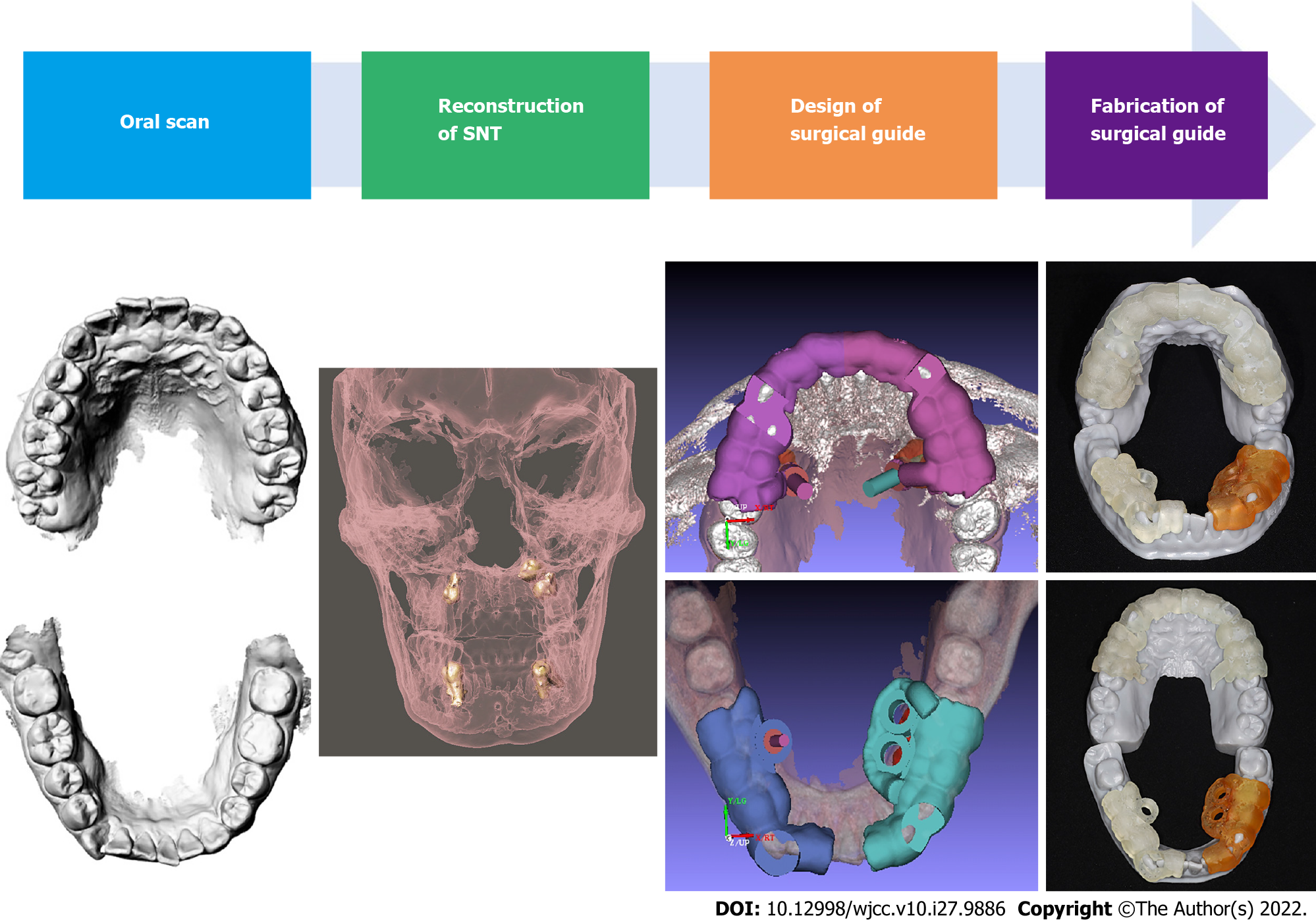
A root canal treatment was proposed for tooth #36, followed by an all-ceramic crown restoration (Figure 3). The seven impacted SNTs were extracted in turn. Preoperatively, to reconstruct the shape of the impacted SNTs and determine whether the lingual or palatal approach should be used for surgical extraction, computer-aided design (CAD) software (Mimics Research, Materialise, Leuven, Belgium; 3-Matic, Materialise, Leuven, Belgium) was used to transform the data into three-dimensional images. Information on the maxillary and mandibular models was obtained by an oral scan (PANDA P2, FREQTY, China) and input into CAD software. After matching, we accurately restored the patient’s mucosal structure and determined the incision line. The edge of the positioning guide plate was modified according to the principle of tooth-supported plates. Finally, individualized digital positioning guide plates were prepared using 3D printing technology (Figure 4).
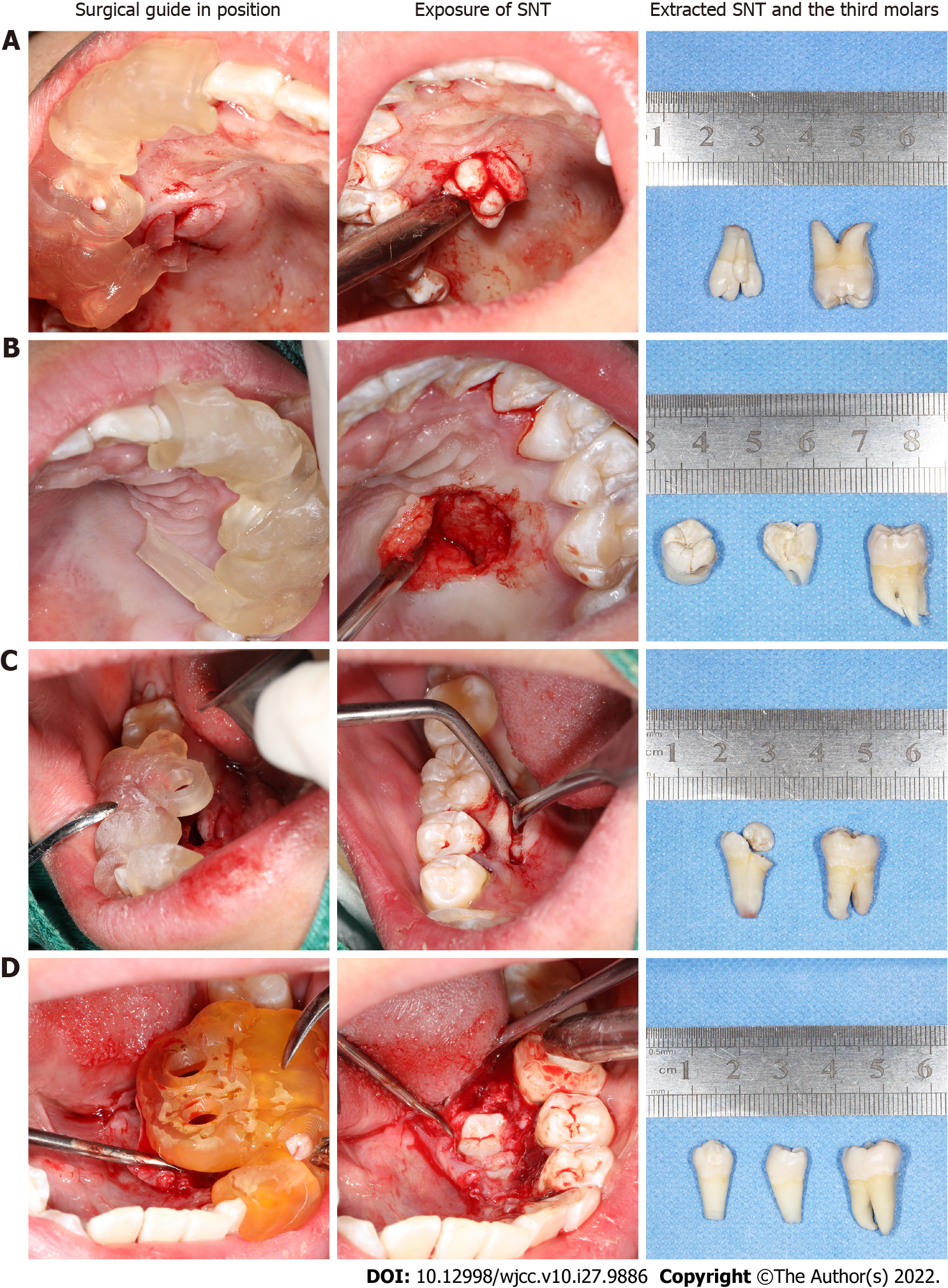
The seven impacted SNTs were extracted in the following order: right maxilla, left maxilla, right mandible, and left mandible. Additionally, teeth #18, #28, #38, and #48 were extracted, respectively (Figure 5). The patient's venous blood was drawn to prepare concentrated growth factor (CGF) before each surgical extraction. After the preoperative preparation, the patient’s mouth was rinsed with 0.12% chlorhexidine solution for 3 min. Local anesthesia was administered with a 2.5 mL 4% articaine hydrochloride and epinephrine tartrate injection (Produits Dentaires Pierre Rolland, France). During the operation, the positioning guide plate was placed in the left mandible, and a trapezoid surgical flap was elevated from tooth #34 to tooth #36. Then, the two impacted SNTs were extracted with the aid of the digital positioning guide plate. The socket was thoroughly debrided and irrigated. Next, "sticky bone" (a mixture of Bio-Oss and CGF) was placed into the socket. Subsequently, the wound was sutured with 5-0 silk. Postoperatively, 250 mg of amoxicillin was prescribed (thrice daily for 5 d). The patient was instructed to rinse with mouthwash with chlorhexidine solution for 10 d and avoided chewing in the surgical area. The sutures were removed after 10 d. The impacted SNTs in the other three quadrants were extracted in the same way using the digital positioning guide plates.
The patient was admitted for follow-up after 10 d for suture removal. Visible vascularization of the soft tissue was found, and there was no swelling or pain after the surgery. Three months postoperatively, panoramic radiographs and CBCT images showed visible regeneration of the bone tissue (Figures 6 and 7). The patient was satisfied with the treatment outcomes.
The pathogenesis of SNTs remains unclear, and several theories have been suggested, including tooth germ dichotomy, hyperactivity of the dental lamina, atavism and a combination of genetic and environmental factors. Tooth germ dichotomy[21] refers to the splitting of a normally developing tooth bud into two buds caused by embryonic aberrations or trauma during odontogenesis. In addition, during facial development, the remaining epithelium of the dental lamina undergoes localized and independent overactivity when embryo aberration occurs, also known as hyperactivity of the dental lamina[22], which leads to the appearance of SNTs. The atavism theory[23] suggests that SNTs emerge to restore the teeth lost by humans during the evolutionary process, and in some individuals, it may be a response to the original number of ancestral teeth. However, this theory can only explain the appearance of supplemental teeth. Many scholars have found that SNTs are closely associated with genetic and environmental factors[24]. It has been reported that SNTs are autosomal dominant, and children whose parents have SNTs have a 5.9 times higher risk of having SNTs[24]. In this case, we can only exclude the last etiological theory based on the clinical examination.A single SNT is usually a simple manifestation of an abnormal number of teeth, while multiple SNTs are usually a manifestation of a syndrome of developmental abnormalities such as cleft lip and palate, cleidocranial dysostosis, and Gardner’s syndrome[25-27]. It is rare to find multiple SNTs in individuals with no other associated disease or syndrome. In the present case, the patient had an uneventful medical history, and the possibility of any syndromes was ruled out. The present case, in which the patient had seven SNTs without any syndromes, appears to be rare.
Intraoral examination of unerupted SNTs is difficult, and most SNTs are diagnosed by chance during radiographic inspection. In the present case, the SNTs were discovered by chance as a radiographic finding. Radiographs are the most reliable and definitive method for diagnosing SNTs. Although panoramic radiographs can provide valid information for the diagnosis of SNTs, they cannot provide precise positions for the impacted SNTs in relation to adjacent anatomical structures. Compared with panoramic radiographs, CBCT allows a more visual and precise observation of the number, location, and morphology of impacted SNTs in three dimensions[28,29] and is therefore helpful in developing a precise surgical protocol.
The treatment of SNTs depends on the location and clinical features of the SNTs[30]. Additionally, early diagnosis is very important for avoiding complications and alleviating any deformities that have occurred. If there are any pathological changes or if the SNTs prevent the eruption or cause the displacement of permanent teeth, they should be extracted as soon as possible. In this case, surgical extraction was performed in all 4 quadrants according to the clinical signs and the proximity of these teeth to the roots of the first molars, which predisposed them to resorption of the first molar roots.
Alveolar surgery should be performed as minimally invasively and precisely as possible. Multiple impacted SNTs should be extracted while avoiding damage to adjacent teeth and other anatomical structures. The operator should take care to avoid causing intraoperative complications such as nerve or vascular injury. Currently, the localization of impacted SNTs can be obtained by CBCT imaging. However, a simple and effective positioning device is needed to act as a bridge to translate the preoperative CBCT information into the surgical procedure. According to the literature, such devices typically include surgical navigation systems and CAD/computer-aided manufacturing (CAM) digital positioning guide plates[31,32]. However, compared to surgical navigation systems, the surgical guide plate is more convenient, practical, and precise and has a greater safety profile, thus reducing surgical risks. In this case, the surgical positioning guide plate was designed with CAD/CAM technology to extract the impacted SNTs. The 2-3 mm guide plate was designed to permit a lingual/palatal approach, is tooth-supported and extends from the lingual protuberance over the incisive to facilitate retention. It is simple and practical, and extraction surgery can be performed under direct vision. Precise positioning reduces the area of the flap, decreases intraoperative bleeding, shortens the extraction time, and reduces postoperative adverse reactions and complications in patients[33,34]. Moreover, the surgeries in this case were all performed under local anesthesia, broadening the applicability of the digital positioning guide plate to other outpatient programs.
However, there are some limitations in the application of digital positioning guide plates. The production of the digital positioning guide plates requires external processing, which increases the preoperative preparation time. In addition, the cost of investigating and manufacturing the guide plates would make the treatment more expensive for the patient. Finally, 3D-printed surgical guide plates have certain limitations in terms of the accuracy of replication, which requires further study[35].
Although the production cost of digital guide plates is high, there is still some room for improvement in accuracy. However, this situation will change as the technology advances and is continuously explored by dentists. Currently, digital guide plates are used not only in alveolar surgery but also in periodontal surgery[36] and implant bone augmentation[37] to achieve more precise, aesthetic and efficient treatment results. In summary, the application of digital guide plates contributes to safe and minimally invasive oral treatment, shortens treatment time and enhances patient comfort.
The present case is an apparently rare presentation of bilateral impacted multiple SNTs without any syndromes. Early diagnosis and management of impacted SNTs is important for reducing the occurrence of complications and alleviating the existing malformations. Minimally invasive surgery has always been one of the goals of alveolar surgeons. The application of an individualized digital positioning guide plate can improve the accuracy and safety of the surgical procedure for impacted SNTs, compensating for some of the limitations of navigation-assisted tooth extraction techniques. The use of a digital positioning guide plate in the extraction of complex SNTs can reduce the difficulty of the procedure, decrease the operative time and alleviate the patient's postoperative reaction and is therefore worth promoting in clinical practice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eccher A, Italy; Sawai MA, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Parolia A, Kundabala M, Dahal M, Mohan M, Thomas MS. Management of supernumerary teeth. J Conserv Dent. 2011;14:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Rajab LD, Hamdan MA. Supernumerary teeth: review of the literature and a survey of 152 cases. Int J Paediatr Dent. 2002;12:244-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 264] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 3. | Hyun HK, Lee SJ, Ahn BD, Lee ZH, Heo MS, Seo BM, Kim JW. Nonsyndromic multiple mandibular supernumerary premolars. J Oral Maxillofac Surg. 2008;66:1366-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Sasaki H, Funao J, Morinaga H, Nakano K, Ooshima T. Multiple supernumerary teeth in the maxillary canine and mandibular premolar regions: a case in the postpermanent dentition. Int J Paediatr Dent. 2007;17:304-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Shah A, Gill DS, Tredwin C, Naini FB. Diagnosis and management of supernumerary teeth. Dent Update. 2008;35:510-512, 514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Meighani G, Pakdaman A. Diagnosis and management of supernumerary (mesiodens): a review of the literature. J Dent (Tehran). 2010;7:41-49. [PubMed] |
| 7. | Scheiner MA, Sampson WJ. Supernumerary teeth: a review of the literature and four case reports. Aust Dent J. 1997;42:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Vinay Kumar Bhardwaj, Jai Ram Kaundal, Anil Chug, Sanjeev Vaid, Abhishek Soni, Mohinder Chandel. Rare occurrence of bilaterally impacted mandibular supernumerary teeth. Dent Hypotheses. 2012;3:83-85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Garvey MT, Barry HJ, Blake M. Supernumerary teeth--an overview of classification, diagnosis and management. J Can Dent Assoc. 1999;65:612-616. [PubMed] |
| 10. | Zhu M, Liu C, Ren S, Lin Z, Miao L, Sun W. Fusion of a supernumerary tooth to right mandibular second molar: a case report and literature review. Int J Clin Exp Med. 2015;8:11890-11895. [PubMed] |
| 11. | Guerrero ME, Shahbazian M, Elsiena Bekkering G, Nackaerts O, Jacobs R, Horner K. The diagnostic efficacy of cone beam CT for impacted teeth and associated features: a systematic review. J Oral Rehabil. 2011;38:208-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Ata-Ali F, Ata-Ali J, Peñarrocha-Oltra D, Peñarrocha-Diago M. Prevalence, etiology, diagnosis, treatment and complications of supernumerary teeth. J Clin Exp Dent. 2014;6:e414-e418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Jun SH, Kim CH, Ahn JS, Padwa BL, Kwon JJ. Anatomical differences in lower third molars visualized by 2D and 3D X-ray imaging: clinical outcomes after extraction. Int J Oral Maxillofac Surg. 2013;42:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Louvrier A, Marty P, Barrabé A, Euvrard E, Chatelain B, Weber E, Meyer C. How useful is 3D printing in maxillofacial surgery? J Stomatol Oral Maxillofac Surg. 2017;118:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 15. | Prasad TS, Sujatha G, Muruganandhan J, Patil S, Raj AT. Three-dimensional Printing in Reconstructive Oral and Maxillofacial Surgery. J Contemp Dent Pract. 2018;19:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Chen X, Xu L, Sun Y, Politis C. A review of computer-aided oral and maxillofacial surgery: planning, simulation and navigation. Expert Rev Med Devices. 2016;13:1043-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Azarmehr I, Stokbro K, Bell RB, Thygesen T. Surgical Navigation: A Systematic Review of Indications, Treatments, and Outcomes in Oral and Maxillofacial Surgery. J Oral Maxillofac Surg. 2017;75:1987-2005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 109] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 18. | Demian N, Pearl C, Woernley TC 3rd, Wilson J, Seaman J. Surgical Navigation for Oral and Maxillofacial Surgery. Oral Maxillofac Surg Clin North Am. 2019;31:531-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Zeren KJ. Minimally invasive extraction and immediate implant placement: the preservation of esthetics. Int J Periodontics Restorative Dent. 2006;26:171-181. [PubMed] |
| 20. | Lee H, Chae YK, Choi S, Jih MK, Lee J-W, Choi SC, Nam OH. Feasibility of a 3D Surgical Guide Technique for Impacted Supernumerary Tooth Extraction: A Pilot Study with 3D Printed Simulation Models. Appl Sci. 2019;9:3905. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Anthonappa RP, Omer RS, King NM. Characteristics of 283 supernumerary teeth in southern Chinese children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e48-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Cassetta M, Altieri F, Di Mambro A, Galluccio G, Barbato E. Impaction of permanent mandibular second molar: a retrospective study. Med Oral Patol Oral Cir Bucal. 2013;18:e564-e568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Yokose T, Sakamoto T, Sueishi K, Yatabe K, Tsujino K, Kubo S, Yakushiji M, Yamaguchi H. Two cases with supernumerary teeth in lower incisor region. Bull Tokyo Dent Coll. 2006;47:19-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Wang XX, Zhang J, Wei FC. Autosomal dominant inherence of multiple supernumerary teeth. Int J Oral Maxillofac Surg. 2007;36:756-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Tereza GP, Carrara CF, Costa B. Tooth abnormalities of number and position in the permanent dentition of patients with complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 2010;47:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Bufalino A, Paranaíba LM, Gouvêa AF, Gueiros LA, Martelli-Júnior H, Junior JJ, Lopes MA, Graner E, De Almeida OP, Vargas PA, Coletta RD. Cleidocranial dysplasia: oral features and genetic analysis of 11 patients. Oral Dis. 2012;18:184-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Álvarez Salgado JA, González-Llanos Fernández de Mesa F, Villaseñor Ledezma JJ, Cañizares Méndez ML, Paredes Sansinenea I, Rodríguez de Lope-Llorca A, Mollejo Villanueva M. [Ectopic craniopharyngioma and Gardner's syndrome: Case report and literature review]. Neurocirugia (Astur). 2017;28:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Kapila S, Conley RS, Harrell WE Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40:24-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 185] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 29. | Becker A, Chaushu S, Casap-Caspi N. Cone-beam computed tomography and the orthosurgical management of impacted teeth. J Am Dent Assoc. 2010;141 Suppl 3:14S-18S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Shih WY, Hsieh CY, Tsai TP. Clinical evaluation of the timing of mesiodens removal. J Chin Med Assoc. 2016;79:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Wang J, Cui NH, Guo YJ, Zhang W. Navigation-Guided Extraction of Impacted Supernumerary Teeth: A Case Report. J Oral Maxillofac Surg. 2017;75:1136.e1-1136.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Jo C, Bae D, Choi B, Kim J. Removal of Supernumerary Teeth Utilizing a Computer-Aided Design/Computer-Aided Manufacturing Surgical Guide. J Oral Maxillofac Surg. 2017;75:924.e1-924.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Chen X, Yuan J, Wang C, Huang Y, Kang L. Modular preoperative planning software for computer-aided oral implantology and the application of a novel stereolithographic template: a pilot study. Clin Implant Dent Relat Res. 2010;12:181-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Burge J, Saber NR, Looi T, French B, Usmani Z, Anooshiravani N, Kim P, Forrest C, Phillips J. Application of CAD/CAM prefabricated age-matched templates in cranio-orbital remodeling in craniosynostosis. J Craniofac Surg. 2011;22:1810-1813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 35. | Werz SM, Zeichner SJ, Berg BI, Zeilhofer HF, Thieringer F. 3D Printed Surgical Simulation Models as educational tool by maxillofacial surgeons. Eur J Dent Educ. 2018;22:e500-e505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 36. | Coachman C, Valavanis K, Silveira FC, Kahn S, Tavares AD, Mahn E, Parize H, Saliba FMP. The crown lengthening double guide and the digital Perio analysis. J Esthet Restor Dent. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 37. | Tarce M, Merheb J, Meeus M, de Faria Vasconcelos K, Quirynen M. Surgical guides for guided bone augmentation: An in vitro study. Clin Oral Implants Res. 2022;33:558-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |