Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9873
Peer-review started: May 3, 2022
First decision: June 8, 2022
Revised: June 30, 2022
Accepted: August 15, 2022
Article in press: August 15, 2022
Published online: September 26, 2022
Processing time: 136 Days and 1.2 Hours
When herpes zoster is complicated with paralytic ileus, this mostly involves acute intestinal pseudo-obstruction of Ogilvie’s syndrome manifesting as obvious dilat
A 76-year-old female patient complained of right upper quadrant pain. Two days later, a blistering, right-sided rash of the thoracoabdominal dermatome (T5-T10) emerged in conjunction with small intestinal dilatation and the inability to defec
This case shows that herpes zoster may induce small bowel pseudo-obstruction in addition to colonic pseudo-obstruction. Epidural block can not only treat inter
Core Tip: In addition to pain, herpes zoster may also cause bowel pseudo-obstruction, mainly colonic pseudo-obstruction. We present a rare small bowel pseudo-obstruction caused by herpes zoster. In this case, the small bowel pseudo-obstruction was relieved when an epidural block was used to treat the pain. Here, we explain the effective mechanism of treatment. Given that sympathetic innervation of the small bowel occurs by way of the T9 and T10 branches, an epidural catheter inserted from T9-T10, local anesthetics effectively blocked the sympathetic nerves innervating the small bowel. We suggest to promote small bowel peristalsis, to expand small bowel blood vessels and to improve small bowel function to relieve small bowel pseudo-obstruction.
- Citation: Lin YC, Cui XG, Wu LZ, Zhou DQ, Zhou Q. Resolution of herpes zoster-induced small bowel pseudo-obstruction by epidural nerve block: A case report. World J Clin Cases 2022; 10(27): 9873-9878
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9873.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9873
Shingles not only cause neuralgia but some patients may also have bowel pseudo-obstruction, also known as Ogilvie’s syndrome. This type of bowel obstruction usually blocks the cecum and colon. Pseudo-obstruction of the small bowel occurs in very few patients[1,2]. In the past, the application of antiviral therapy, gastrointestinal decompression, enema, and other therapies was able to relieve intestinal obstruction, but there were still a few patients with intestinal obstruction that could not be relieved, resulting in intestinal ischemic necrosis and perforation, requiring surgical treatment[3]. This article focuses on a rare case of herpes zoster complicated by small bowel pseudo-obstruction. The immediate pain and small bowel pseudo-obstruction caused by herpes zoster were relieved by epidural block after failure of conservative treatment. Similar cases have not been reported in the literature. The diagnostic and therapeutic process and possible mechanisms of effective therapy are reported and discussed below.
Right upper quadrant pain for more than 2 d, which worsened 3 h prior to admission.
More than 2 d prior, the 76-year-old female patient had developed intermittent, dull pain in the right upper quadrant with no obvious cause. There was no radiating pain in other body parts. There was also no chest tightness, fever, yellow eyes, yellow urine, yellow skin, nausea, vomiting, abdominal distension, diarrhea, low back pain, hematuria or other discomfort. Three hours prior to this admission, the patient’s symptoms worsened and became unbearable.
The patient had a 2-year history of hypertension, irregular use of calcium channel blockers, and poor blood pressure (BP) control.
The patient denied any family history of malignant tumors.
Physical examination vital signs: body temperature: 36.5 °C, BP: 130/90 mmHg, heart rate (HR): 82 beats per min, and respiratory rate: 19 breaths per min. The cardiopulmonary examination was normal. The patient exhibited right upper quadrant tenderness, a positive Murphy sign, no obvious pain on percussion of both kidneys, no abdominal pressure, decreased bowel sounds, and no signs of abdominal irritation.
The white blood cell count was normal, the neutrophil ratio was 78.5%, and the liver function tests were normal.
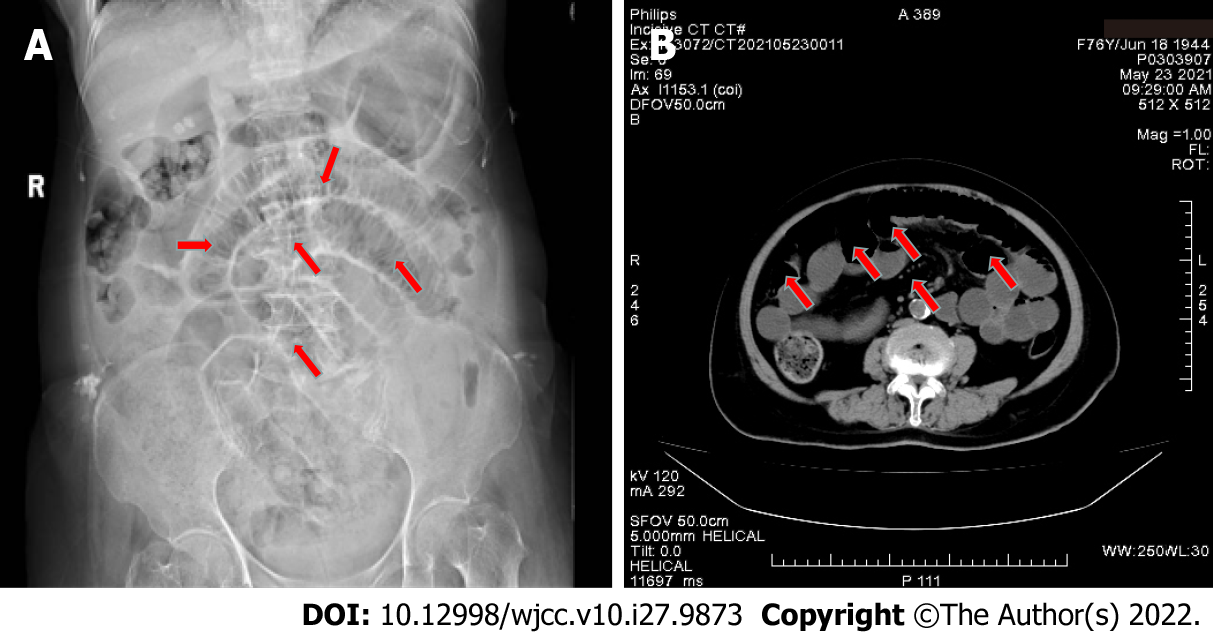
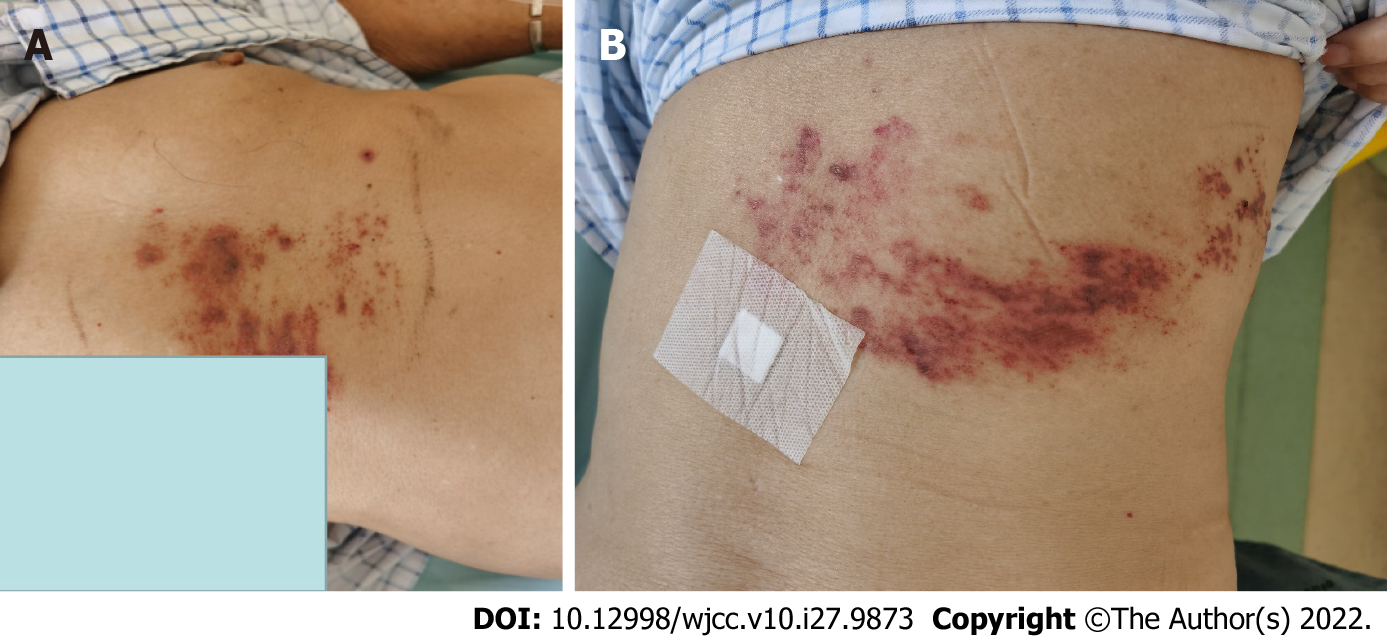
On the 1st day after admission, the patient still had paroxysmal pain in the right upper quadrant. Magnetic resonance imagery showed multiple gallstones, so the condition was misdiagnosed as pain from gallstones. On the 2nd day after admission, the pain was accompanied by abdominal distension, and defecation and exhalation from the anus ceased. On the 3rd day after admission, a cluster of red blisters was found on the right abdomen, extending beyond the midline of the back, involving the T5-T10 dermatomes, with small clusters of blisters and obvious tenderness (Figure 1). A dermatological diagnosis of herpes zoster was made. Plain abdominal radiographs and three-dimensional helical computed tomography showed stepped dilatation of the small bowel, suggesting low-grade small bowel obstruction, but no obvious obstruction was found (Figure 2).
Herpes zoster complicated by small bowel pseudo-obstruction.
Fasting and enemas, topical compound polymyxin B ointment, red light irradiation, intramuscular injection of acyclovir, vitamin B1 injection, oral mecobalamin tablets, and other treatments did not relieve the pain or abdominal distension. On the 5th day after admission, an anesthesiologist was invited for consultation, and the anesthesiologist recommended epidural block therapy. After entering the operating room, superficial venous access was established, and after monitoring, the vital signs were stable. Epidural puncture was performed between T9 and T10. The catheter was advanced 4 cm into the epidural space, and then 1%-lidocaine 3 mL was delivered. Thereafter, the patient passed intestinal gas and defecated. Ten minutes later, 10 mL of a solution containing 0.75%-ropivacaine (2 mL), betamethasone sodium phosphate (5.26 mg), vitamin B12 (0.5 mg), and 0.9%-normal saline (11 mL, total of 15 mL) was injected. Gas and stool were again passed, and the abdominal distension resolved. However, the BP dropped to 85/56 mmHg, and the HR dropped to 52 beats/min. The level of anesthesia was assessed as T4-T12. The BP returned to the normal range (145-126/85-70 mmHg) by injection of ephedrine hydrochloride 6 mg. After 30 min of observation, the patient was sent back to the ward after reaching hemodynamic stability.
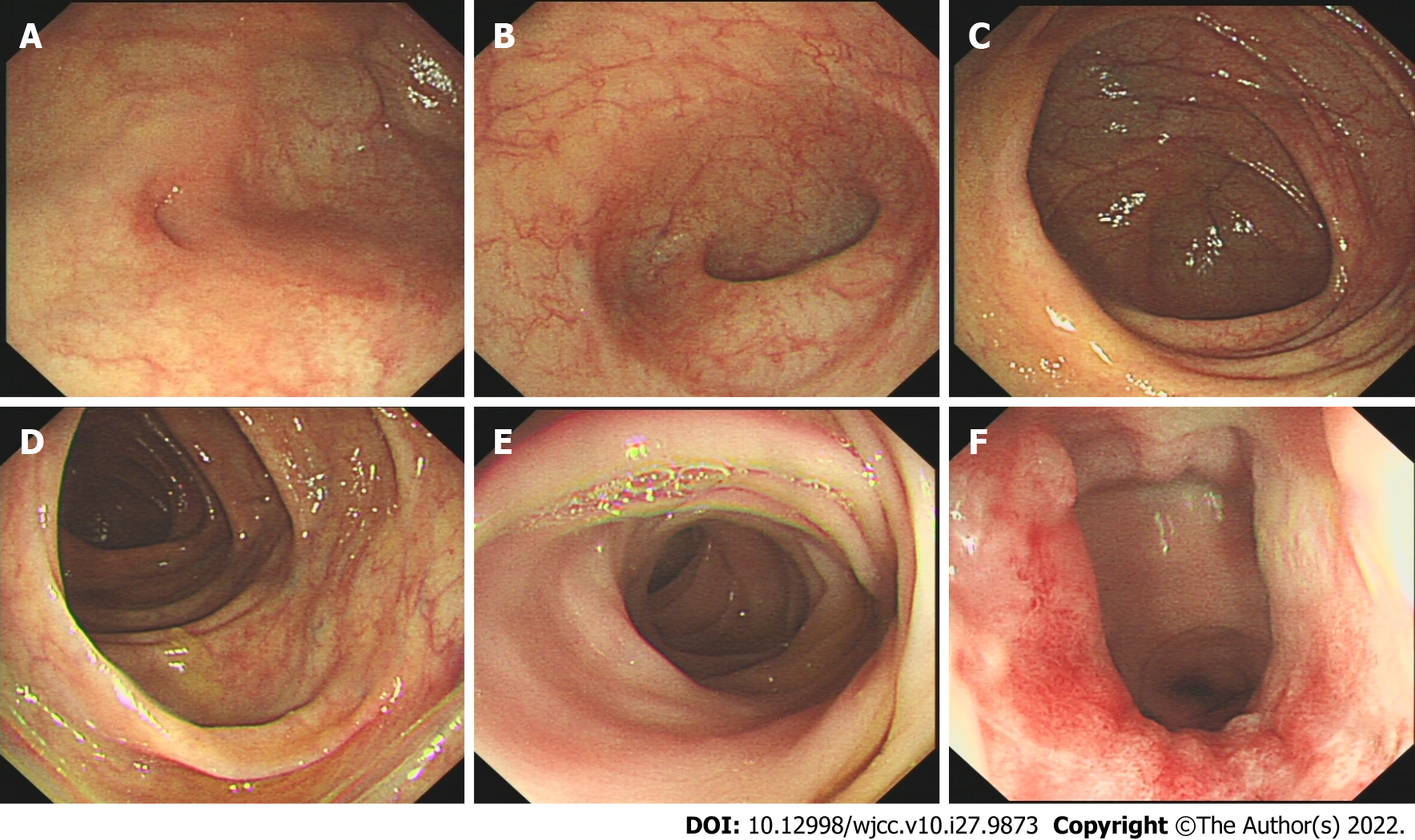
Antiviral and neurotrophic therapy continued after the epidural block. Three days after epidural block, the herpes lesions were dry and crusted, there was no abdominal distension (Figure 3), and a semiliquid diet was started. Gastrointestinal endoscopy performed on day 5 after epidural block showed no abnormalities (Figure 4), and on day 7, the patient was fully recovered.
Varicella-zoster virus (VZV) is a neurotropic virus that persists in nerve cells in the dorsal root ganglia of the spinal cord[4,5]. When immunity is weakened, the virus is activated, migrates along neuronal axons, grows shingles on the skin, and can further invade the visceral nerve fibers of the sympathetic and parasympathetic nerves, causing gastrointestinal and urinary tract dysfunction. Severe cases may be complicated with intestinal pseudo-obstruction and intestinal ischemia perforation, requiring surgical treatment[6]. In acute colonic pseudo-obstruction, also known as Ogilvie's syndrome, the typical X-ray findings of Ogilvie's syndrome are marked dilatation of the cecum, ascending colon, and transverse colon. The clinical presentation is similar to that of mechanical ileus, with abdominal pain, bloating, and constipation[2].
Various theories on the pathogenesis of zoster-related gut obstruction are as follows: (1) Direct viral damage to intestinal nerve fibers (submucosal, myenteric plexuses) and muscle layers[7]; (2) Damage to spinal nerves of the lateral thoracolumbosacral column, blocking sacral parasympathetic nerves and thus impeding intestinal contractility[8]; (3) Hemorrhagic infarction of the abdominal sympathetic ganglia (implicated as being the chief means of colonic pseudo-obstruction)[9]; and (4) Afferent nerve fiber blockade, reducing gastrointestinal motility and culminating in acute intestinal pseudo-obstruction[10].
Anaya-Prado et al[11] also reported small bowel pseudo-obstruction caused by herpes zoster, which is thought to have the same mechanism as that of colonic pseudo-obstruction. Herpes zoster virus stimulates sympathetic nerves, inhibits small intestinal peristalsis, constricts small intestinal blood vessels (with positive VZV DNA exhibited on small intestinal biopsy), and damages the myenteric plexus and muscularis propria.
Traditional management of zoster-induced intestinal obstruction has largely been conservative, relying on methods such as acyclovir, analgesia, neurotrophic agents and enemas. Such actions are meant to reduce the sympathetic inflammatory response and improve blood supply to the gut, thereby increasing tone and motility. In 1999, Ponec and associates[12] slowly administered IV neostigmine (2.0 mg) to 8 patients with colonic pseudo-obstruction, who then released gas and stool within 3-30 min post-injection and experienced less distension. Neostigmine accumulates gut acetylcholine (Ach) in cholinergic nerve endings, manifesting as M- and N-like effects of Ach, and excites gastrointestinal smooth muscle.
During the 1920s and 1930s, intraspinal anesthesia was shown to qualitatively increase gastro
Lee et al[14] performed epidural blocks in 8 patients with herpes zoster and associated colonic pseudo-obstruction. Epidural puncture was performed at the T11-T12 intercostal space, delivering 0.25% bupivacaine at a nominal dose, a loading dose of 5-10 mL, and a continuous epidural infusion of 3 mL/h for 60 h. Defecation ensued in 5 patients, reducing the diameter of the cecum.
Given that sympathetic innervation of the small intestine occurs by way of the T9 and T10 branches and that the primary viral manifestations in the patient involved T5-T10, an epidural catheter inserted from T9-T10 local anesthetics effectively blocked the sympathetic nerves innervating the small intestine. Consequently, the patient readily expelled gas and stool. The epidural block of this patient was not administered by continuous pump injection of local anesthetics. Instead, a mixture of local anesthetics, hormones and vitamin B12 was used as the blocking solution. The main consideration was that the local anesthetics had a short action time, while the hormones had a long action time, which could have inhibited the inflammatory response; vitamin B12 possibly played a role in nerve nutrition. Qian et al[15] reported that high-dose and long-term use of hormones may induce herpes zoster, suggesting that the lowest possible dose and shortest duration of treatment be recommended. The patient in this case had a single application with a low hormone dose, so this is unlikely to cause recurrent herpes zoster.
The present case shows that herpes zoster may induce small bowel pseudo-obstruction in addition to colonic pseudo-obstruction. Epidural block can not only treat inter
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Al-Ani RM, Iraq; Šimurina T, Croatia; Soe KK, United States S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Pai NB, Murthy RS, Kumar HT, Gerst PH. Association of acute colonic pseudo-obstruction (Ogilvie's syndrome) with herpes zoster. Am Surg. 1990;56:691-694. [PubMed] |
| 2. | Edelman DA, Antaki F, Basson MD, Salwen WA, Gruber SA, Losanoff JE. Ogilvie syndrome and herpes zoster: case report and review of the literature. J Emerg Med. 2010;39:696-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 3. | Ben Ameur H, Boujelbene S, Beyrouti MI. [Treatment of acute colonic pseudo-obstruction (Ogilvie's Syndrome). Systematic review]. Tunis Med. 2013;91:565-572. [PubMed] |
| 4. | Kennedy PG, Graner MW, Gunaydin D, Bowlin J, Pointon T, Yu X. Varicella-Zoster Virus infected human neurons are resistant to apoptosis. J Neurovirol. 2020;26:330-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Zerboni L, Sen N, Oliver SL, Arvin AM. Molecular mechanisms of varicella zoster virus pathogenesis. Nat Rev Microbiol. 2014;12:197-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 313] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 6. | Chen JJ, Gershon AA, Li Z, Cowles RA, Gershon MD. Varicella zoster virus (VZV) infects and establishes latency in enteric neurons. J Neurovirol. 2011;17:578-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Pui JC, Furth EE, Minda J, Montone KT. Demonstration of varicella-zoster virus infection in the muscularis propria and myenteric plexi of the colon in an HIV-positive patient with herpes zoster and small bowel pseudo-obstruction (Ogilvie's syndrome). Am J Gastroenterol. 2001;96:1627-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Tribble DR, Church P, Frame JN. Gastrointestinal visceral motor complications of dermatomal herpes zoster: report of two cases and review. Clin Infect Dis. 1993;17:431-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 9. | Nomdedéu JF, Nomdedéu J, Martino R, Bordes R, Portorreal R, Sureda A, Domingo-Albós A, Rutllant M, Soler J. Ogilvie's syndrome from disseminated varicella-zoster infection and infarcted celiac ganglia. J Clin Gastroenterol. 1995;20:157-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Hosoe N, Sakakibara R, Yoshida M, Wakabayashi T, Kikuchi H, Yamada T, Kawahara K, Kishi M. Acute, severe constipation in a 58-year-old Japanese patient. Gut. 2011;60:1059, 1093. [PubMed] |
| 11. | Anaya-Prado R, Pérez-Navarro JV, Corona-Nakamura A, Anaya-Fernández MM, Anaya-Fernández R, Izaguirre-Pérez ME. Intestinal pseudo-obstruction caused by herpes zoster: Case report and pathophysiology. World J Clin Cases. 2018;6:132-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 12. | Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999;341:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 331] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 13. | Mashour GA, Peterfreund RA. Spinal anesthesia and Ogilvie's syndrome. J Clin Anesth. 2005;17:122-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Lee JT, Taylor BM, Singleton BC. Epidural anesthesia for acute pseudo-obstruction of the colon (Ogilvie's syndrome). Dis Colon Rectum. 1988;31:686-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Qian J, Banks E, Macartney K, Heywood AE, Lassere MN, Liu B. Corticosteroid Use and Risk of Herpes Zoster in a Population-Based Cohort. Mayo Clin Proc. 2021;96:2843-2853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |