Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9859
Peer-review started: May 3, 2022
First decision: June 8, 2022
Revised: June 14, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: September 26, 2022
Processing time: 136 Days and 11.5 Hours
Eisenmenger syndrome (ES) is an uncorrected congenital cardiac defect with a left-to-right shunt, leading to pulmonary arterial hypertension. Patients with ES are susceptible to hemodynamic alterations during noncardiac surgery with general anesthesia, which increases perioperative morbidity and mortality. Monitored anesthesia care (MAC) is often used during minor procedures in patients with cardiac disease. However, few reports on MAC in patients with ES exist.
A 49-year-old man was admitted for a severe headache lasting 30 d. He had been diagnosed with a large perimembranous ventricular septal defect (VSD) with bidirectional shunt flow and pulmonary arterial hypertension 10 years ago. A round mass in the right frontal lobe was revealed by Magnetic resonance imaging. Stereotactic aspiration using a neuronavigation system was performed under MAC. The patient was stayed in the hospital for 5 d, and discharged without complications.
MAC may be effective for craniotomy in patients with ES.
Core Tip: Monitored anesthesia care (MAC) is often used during minor procedures in patients with cardiac disease. However, there are few reports on MAC in patients with Eisenmenger syndrome (ES). We report a case of MAC using dexmedetomidine and remifentanil for craniotomy in a patient with ES.
- Citation: Ri HS, Jeon Y. Monitored anesthesia care for craniotomy in a patient with Eisenmenger syndrome: A case report. World J Clin Cases 2022; 10(27): 9859-9864
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9859.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9859
Eisenmenger syndrome (ES) is an advanced form of pulmonary arterial hypertension caused by congenital heart disease[1]. ES is characterized by irreversible severe pulmonary hypertension and a left-to-right shunt. When pulmonary artery pressure reaches the systemic level, ES cannot be resolved[1]. As the life expectancy of patients with ES has improved in recent decades, the number of adult patients undergoing noncardiac surgery has steadily increased[2,3]. Patients with ES undergoing noncardiac surgery are at high risk for fatal or life-threatening complications during the perioperative period[4-8]; perioperative systemic inflammatory response, hypoxemia, or hypercapnia and activation of the sympathetic nervous system can lead to deterioration of pulmonary hypertension and right heart failure in patients with ES[9-11]. Therefore, anesthetic management of patients with ES is challenging, and comprehensive, evidence-based guidelines for anesthetic management are needed[12]. Monitored anesthesia care (MAC) is an anesthetic technique that provides conscious sedation with a local anesthetic and sedative for minor surgeries, including cardiovascular interventions and craniotomy. Herein, we report the case of a patient with ES who underwent MAC for craniotomy for a brain abscess.
A 49-year-old man (170 cm, 48.4 kg) was admitted for a severe headache.
The headache lasted for 30 d.
He had been diagnosed with a large perimembranous ventricular septal defect (VSD) with bidirectional shunt flow and pulmonary arterial hypertension 10 years ago. He had exertional dyspnea and heart function classified as New York Heart Association Class Ⅲ and was on medications, including bosentan, furosemide, and spironolactone.
He was on medications, including bosentan, furosemide, and spironolactone.
He had exertional dyspnea and heart function classified as New York Heart Association Class Ⅲ.
Preoperative blood laboratory assessments, such as complete blood count and liver and kidney tests, were unremarkable.
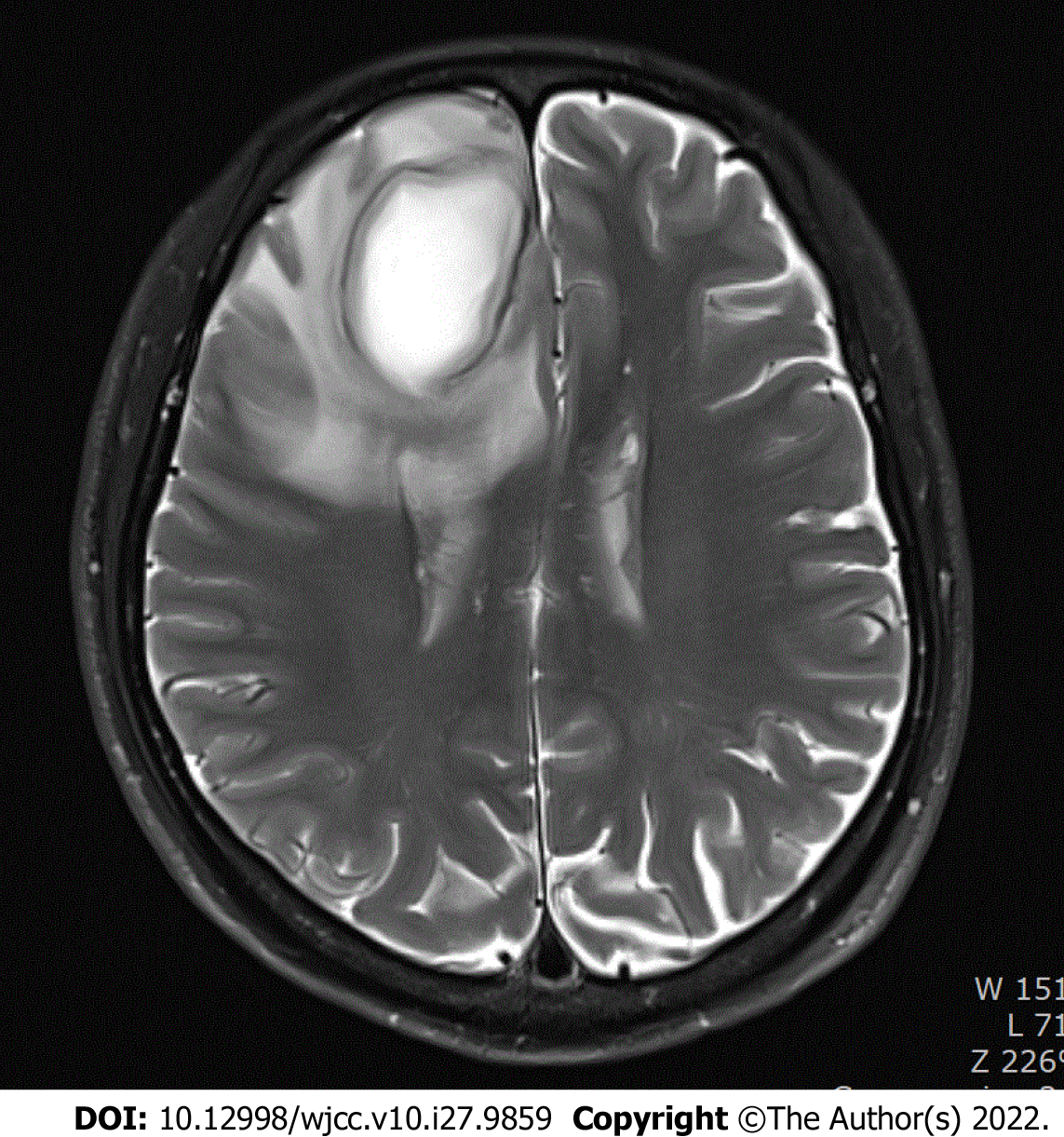
Electrocardiography (ECG) revealed sinus rhythm with left ventricular hypertrophy. Cardiac catheterization demonstrated a pulmonary artery pressure of 101/62 mmHg, pulmonary vascular resistance of 15.1 Woods units, and cardiac output of 3.44 L/min. Echocardiography revealed a large VSD (18 mm) with bidirectional shunt flow, a D-shaped left ventricle with normal systolic ejection function (56%), right ventricular hypertrophy with preserved right ventricular contractibility, and resting pulmonary hypertension with trivial tricuspid regurgitation. Magnetic resonance imaging revealed a round mass in the right frontal lobe, which was suspected to be a brain abscess (Figure 1).
We suspected that the patient had a brain abscess in the area of the right frontal lobe.
The patient was scheduled to undergo stereotactic aspiration using a neuronavigation system (StealthStation® S7, Medtronic, Inc., Louisville, CO, United States) under MAC. Premedication was not administered. Standard monitoring included ECG, pulse oximetry, invasive blood pressure measurement, and esophageal stethoscope temperature measurement.
Before induction of MAC, a 20 G catheter was inserted into the left radial artery, and arterial blood gas analysis on room air showed a pH of 7.49, partial pressure of carbon dioxide (PaCO2) of 30 mmHg, partial pressure of oxygen (PaO2) of 53 mmHg, bicarbonate ion (HCO3-) concentration of 22.1 mmol/L, and oxygen saturation (SaO2) of 89.9%. Cardiac output (CO), stroke volume (SV), and stroke volume variation (SVV) were continuously measured using a FloTrac®/Vigileo device (Edwards Lifesciences, Irvine, CA, United States). CO, SV, and SVV were 6.1 L/min, 100 mL/beat, and 5%, respectively. Oxygen was provided at 20 L/min with a fraction of inspired oxygen (FiO2) of 0.95 using a high-flow nasal cannula (HFNC) (Flo EasyTM, Westmed, Inc., Tucson, AZ, United States) during the perioperative period. MAC was induced with dexmedetomidine at a loading dose of 1 μg/kg for 30 min. After infiltration of 2% lidocaine into the insertion site, a central venous catheter was inserted into the right internal jugular vein. During the procedure, remifentanil and dexmedetomidine were infused at the rate of 0.02 μg/kg/min and 0.8-1.2 μg/kg/h, respectively. To manage the pulmonary hypertension, remodulin was infused intravenously at a rate of 0.01 μg/kg/min. The patient was placed in the supine position on a horseshoe headrest. Local anesthesia at the incision site was induced with 0.5% bupivacaine with 1:200000 epinephrine, and craniotomy was performed. Stereotactic aspiration was performed, and 20 mL of yellow discharge was extracted. During surgery, the heart rate was 60-80 beats/min, spot oxygen saturation was 97%-99%, mean arterial pressure was 99-86 mmHg, and body temperature was 36.6 °C. CO, SV, and SVV were 4.6-6.1 L/min, 69-100 mL/beat, and 5%-9%, respectively. Arterial blood gas analysis showed that pH, PaCO2, PaO2, HCO3-, and SaO2 were 7.42, 42.0 mmHg, 94.0 mmHg, 27.2 mmol/L, and 97.0%, respectively. The surgery lasted for 60 min, and the patient tolerated the surgery without dysrhythmia or hemodynamic changes. After discontinuation of MAC, the patient was conscious and transferred to the surgical intensive care unit (ICU).
In the surgical ICU, oxygen was provided at a rate of 4 L/min via a facemask.
The patient cooperated well. The patient was transferred to the ward on postoperative day 3, and 2 d later, he was discharged without complications. The timeline of this case is shown in Table 1.
| Item | Timeline | |
| Preoperative | 1 | Admission for a severe headache lasting 30 d |
| 2 | Past history-Large perimembranous VSD with bidirectional shunt flow and pulmonary arterial hypertension 10 years ago | |
| 3 | MRI-A round mass in the right frontal lobe | |
| 4 | Plan-craniotomy under MAC | |
| Perioperative | 5 | Arterial cannulation and arterial blood gas analysis |
| 6 | Advanced hemodynamic monitoring-CO, SV, SVV | |
| 7 | Oxygen supply-high-flow nasal cannula | |
| 8 | MAC induction with dexmedetomidine loading | |
| 9 | Central venous catheterization | |
| 10 | Remifentanil, remodulin infusion | |
| 11 | Neuronavigation system set | |
| 12 | Craniotomy and stereotactic aspiration | |
| Postoperative | 13 | ICU for 3 d |
| 14 | Discharge on POD 5 | |
ES is defined as an untreated congenital cardiac defect with a left-to-right shunt that results in elevation of pulmonary arterial pressure at a systemic level[13]. The main anesthetic goals in patients with ES are as follows: (1) Maintain euvolemia; (2) optimize systematic vascular resistance; and (3) avoid the elements that increase pulmonary vascular resistance (pain, hypoxia, and hypercapnia)[3,14,15].
MAC with sedation has been implemented in anesthesia management of patients with ES, even for minor surgical procedures. The major concerns in MAC are (1) hypoxia and hypercarbia due to oversedation and lack of adequate airway support, and (2) potential agitation and uncontrollable behaviors due to the paradoxical reaction of sedative agents[13].
Dexmedetomidine, an alpha-2 adrenoreceptor agonist, has sedative and analgesic effects. It can induce sedation without respiratory depression and could, therefore, be a good choice to sedate patients with Eisenmenger features, while avoiding hypoxemia or hypercapnia. Intravenous anesthetics, such as propofol, have myocardial depression and respiratory inhibition effects, which can cause problems in patients with severe pulmonary arterial hypertension. Dexmedetomidine is less likely to cause paradoxical reactions than other anesthetics, such as benzodiazepines. The disadvantage of dexmedetomidine is the slow time of action. However, neuronavigation preparation took 30 min; therefore, it was used without inconvenience.
Although the use of opioids can cause respiratory depression and chest wall rigidity, we used a minimal dose of remifentanil while providing oxygen through an HFNC and adjusting it as needed. This was because intraoperative pain could not be sufficiently controlled with dexmedetomidine alone. HFNC is a recent noninvasive technique that provides heated and humidified gas. HFNC was applied to patients with pulmonary arterial hypertension to avoid hypoxia and hypercarbia, thereby decreasing the need for intubation[16]. In this case, HFNC with 0.95% FiO2 was performed, and the intraoperative vital signs were stable.
FloTrac®/Vigileo is a minimally invasive hemodynamic monitoring device that can be used via the radial artery[17]. Advanced hemodynamic variables (CO, SV, and SVV) were monitored, but systemic vascular resistance was not. Monitoring of advanced hemodynamic variables allowed the patient to remain stable without the use of vasoactive agents. A pulmonary artery catheter could be used; however, it is difficult to place it appropriately in patients with pulmonary hypertension without sedation and poses a risk of fatal complications.
MAC with dexmedetomidine and remifentanil may be effective for craniotomy in patients with ES. Supplementing oxygen via HFNC is advisable to avoid hypoxia.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta A, India; Wang XQ, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Jung JW. Pulmonary arterial hypertension of congenital heart diseases: from reversible pulmonary hypertension to Eisenmenger syndrome. Korean Circ J. 2007;37:287-297. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Park HY, Lee HD, Kwak HJ, Lee JY, Kim HS. Anesthetic management for a patient with Eisenmenger syndrome undergoing dacryocystorhinostomy: A case report. Anesth Pain Med. 2010;5:56-59. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Bala R, Pirkad A, Saini S, Banerjee A. Anesthetic management of a patient with Eisenmenger syndrome: what next when one technique fails? Anaesth Pain Intensive Care. 2016;20:327-329. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Deljou A, Sabov M, Kane GC, Frantz RP, DuBrock HM, Martin DP, Schroeder DR, Johnson MQ, Weingarten TN, Sprung J. Outcomes After Noncardiac Surgery for Patients with Pulmonary Hypertension: A Historical Cohort Study. J Cardiothorac Vasc Anesth. 2020;34:1506-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Smilowitz NR, Armanious A, Bangalore S, Ramakrishna H, Berger JS. Cardiovascular Outcomes of Patients With Pulmonary Hypertension Undergoing Noncardiac Surgery. Am J Cardiol. 2019;123:1532-1537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Disselkamp M, Adkins D, Pandey S, Coz Yataco AO. Physiologic Approach to Mechanical Ventilation in Right Ventricular Failure. Ann Am Thorac Soc. 2018;15:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Kaw R, Pasupuleti V, Deshpande A, Hamieh T, Walker E, Minai OA. Pulmonary hypertension: an important predictor of outcomes in patients undergoing non-cardiac surgery. Respir Med. 2011;105:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Ramakrishna G, Sprung J, Ravi BS, Chandrasekaran K, McGoon MD. Impact of pulmonary hypertension on the outcomes of noncardiac surgery: predictors of perioperative morbidity and mortality. J Am Coll Cardiol. 2005;45:1691-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 250] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 9. | Forrest P. Anaesthesia and right ventricular failure. Anaesth Intensive Care. 2009;37:370-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Vongpatanasin W, Brickner ME, Hillis LD, Lange RA. The Eisenmenger syndrome in adults. Ann Intern Med. 1998;128:745-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 169] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Raines DE, Liberthson RR, Murray JR. Anesthetic management and outcome following noncardiac surgery in nonparturients with Eisenmenger's physiology. J Clin Anesth. 1996;8:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Seo JS, So KY, Kim SH. Perioperative anesthetic considerations in patients with pulmonary hypertension undergoing non-cardiac and non-obstetric surgeries. Med Biol Sci Eng. 2019;2:31-39. [DOI] [Full Text] |
| 13. | Bennett J. Anaesthesia recommendations for Eisenmenger syndrome. Anästh Intensivmed. 2021;62:S173-S182. [DOI] [Full Text] |
| 14. | Kopka A, McMenemin IM, Serpell MG, Quasim I. Anaesthesia for cholecystectomy in two non-parturients with Eisenmenger's syndrome. Acta Anaesthesiol Scand. 2004;48:782-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Burbridge MA, Brodt J, Jaffe RA. Ventriculoperitoneal Shunt Insertion Under Monitored Anesthesia Care in a Patient With Severe Pulmonary Hypertension. A A Case Rep. 2016;7:27-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Gupta B, Kerai S, Kakkar K, Gupta L. Role of High-flow Nasal Oxygen Therapy in Cases with Pulmonary Hypertension in an Intensive Care Unit Setting. Indian J Crit Care Med. 2019;23:458-461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Botsch A, Firstenberg MS. Comment on the Edwards FloTrac™/Vigileo versus pulmonary artery catheter study: What is really going on with this patient? Int J Crit Illn Inj Sci. 2017;7:183-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |