Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9845
Peer-review started: April 27, 2022
First decision: June 8, 2022
Revised: June 27, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: September 26, 2022
Processing time: 141 Days and 21.7 Hours
Coronavirus disease-2019 (COVID-19) is a highly pathogenic respiratory disease that mainly affects adults and elderly patients. Yet, over the past three years, there were an increasing number of infected children; however, only a few cases of infants with reverse-transcription polymerase chain reaction (RT-PCR)-confirmed COVID-19 and chest computed tomography (CT) normal have been reported. Herein, we reported a single case of a patient (a 3-mo-old girl) with COVID-19, including her clinical and imaging findings.
The patient with fever, diarrhea came to fever clinic. Her chest CT was normal. The patient was treated accordingly, the fever disappeared while diarrhea persisted, what’s more, RT-PCR testing of nasopharyngeal swab showed positive results; thus, the patient was admitted to the pediatric department on the 5th day of onset. The child was given systematic treatment, and all her symptoms sig
This report provides useful references for treating infantile COVID-19 cases with diarrhea or other non-respiratory symptoms and normal chest CT scan. Given the persistent positive RT-PCR results of anal swabs, the possibility of fecal-oral transmission of COVID-19 should be considered.
Core Tip: This study reports an atypical infantile case of coronavirus disease-2019 accompanied by diarrhea or other non-respiratory symptoms. We presented the medical history and the whole process of diagnosis and management of the case and did a literature review. In this paper, we share our experience, which might provide a useful reference for pediatricians and radiologists.
- Citation: Ji GH, Li B, Wu ZC, Wang W, Xiong H. Infant with reverse-transcription polymerase chain reaction confirmed COVID-19 and normal chest computed tomography: A case report. World J Clin Cases 2022; 10(27): 9845-9850
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9845.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9845
Coronavirus disease-2019 (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that originated in China in 2019 and rapidly spread worldwide[1]. Although the disease is mainly affecting adults and the elderly, children of all ages can also get infected and experience serious complications. Moreover, while CT features and clinical characteristics of adult COVID-19 patients have been well investigated[2-3], data regarding pediatric patients are still lacking. Clinical reports have suggested that children with COVID-19 usually have mild clinical manifestations, most of which are transient fever or mild respiratory symptoms. Some children may present with diarrhea. Also, non-respiratory symptoms with negative or mild lung imaging findings have also been found in some cases [4]. The coincidence of the outbreak of COVID-19 and the winter-spring flu season was also challenging for establishment of early accurate diagnosis and intervention of pediatric pneumonia. Consequently, a better understanding of clinical and imaging features related to COVID-19 in infants, especially the atypical cases, is urgently needed.
Herein, we reported a single case of a 3-mo old female patient with COVID-19, including her clinical and imaging findings.
A 3 mo and 14 d old female infant visited our department on January 26, 2020 due to a fever that lasted one day and diarrhea that persisted for four days.
Her parents were Wuhan city residents who returned to Jingzhou city on January 18, 2020. Her father had fever and cough on January 25, 2020; the same symptoms were found in the infant one day later.
Patients did not report a history of any underlying disease. The laboratory testing of the infant was: Elevated peripheral white blood cells and lymphocytes, reduced neutrophils, normal C-reactive protein (CRP), elevated lactic dehydrogenase (LDH), alanine aminotransferase (ALT), and aspartate amino
| Time | Jan 26, 2020 | Jan 31, 2020 | Feb 6, 2020 | Feb 23, 2020 | Feb 28, 2020 |
| WBC | 10.39 × 109/L (5-12) | 13.21 × 109/L (5-12) | 12.90 × 109/L (5-12) | 15.4 × 109/L (5-12) | 8.5 × 109/L (5-12) |
| RBC | 4.03×1012/L (4.3-5.8) | 4.38 × 1012/L (4.3-5.8) | 4.09 × 1012/L (4.3-5.8) | 3.99 × 1012/L (4.3-5.8) | 3.63 × 1012/L (4.3-5.8) |
| Hemoglobin | 114 g/L (130-175) | 128 g/L (130-175) | 116.1 g/L (130-175) | 109.9 g/L (130-175) | 109.8 g/L (130-175) |
| Thrombocyte | 196 × 109/L (100-300) | 527 × 109/L (100-300) | 534 × 109/L (100-300) | 418 × 109/L (100-300) | 359 × 109/L (100-300) |
| Neutrophils | 6.62 × 109/L (1.8-6.3) | 0.93 × 109/L (1.8-6.3) | 3.61 × 109/L (1.8-6.3) | 2.33 × 109/L (1.8-6.3) | 1.86 × 109/L (1.8-6.3) |
| Lymphocytes | 2.84 × 109/L (1.1-3.2) | 11.39 × 109/L (1.1-3.2) | 64.6 × 109/L (1.1-3.2) | 11.6 × 109/L (1.1-3.2) | 5.97 × 109/L (1.1-3.2) |
| Influenza A virus | - | ||||
| Influenza B virus | - | ||||
| CRP | 0.47 mg/L (0-8) | 0.11 mg/L (0-8) | 0.49 mg/L (0-8) | 0.35 mg/L (0-8) | |
| Albumin | 44.6 g/L (35-55) | 44.5 g/L (35-55) | 43.9 g/L (35-55) | 43.7 g/L (35-55) | |
| Globulin | 17.0 g/L (20-35) | 16.3 g/L (20-35) | 16.3 g/L (20-35) | 13.8 g/L (20-35) | |
| Albumin/Globulin | 2.62 (1.2-2.5) | 2.73 (1.2-2.5) | 2.69 (1.2-2.5) | 3.17 (1.2-2.5) | |
| ALT | 143 U/L (1-40) | 78 U/L (1-40) | 66 U/L (1-40) | 59 U/L (1-40) | |
| AST | 185 U/L (2-42) | 72 U/L (2-42) | 66 U/L (2-42) | 71 U/L (2-42) | |
| ALP | 212 U/L (35-128) | 217 U/L (35-128) | |||
| LDH | 348 U/L (100-240) | 289 U/L (100-240) | 298 U/L (100-240) | 228 U/L (100-240) | |
| TBA | 12.99 μmol/L (0-10) | 5.16 μmol/L (0-10) | 7.9 μmol/L (0-10) | 4.8 μmol/L (0-10) | |
| CK-MB | 51 U/L (0-20) | 48U/L (0-20) | 63 U/L (0-20) | 34 U/L (0-20) |
The infant’s father and mother were diagnosed with COVID-19 on January 26 and January 29, 2020, respectively.
Physical examination suggested: Body temperature, 36.5ºC; blood pressure, 85/46 mmHg; heart rate, 119 beats per min; respiratory rate, 34 breaths per min. Her breathing was stable, without a nasal fan and three concave signs. The breath sounded thick, no obvious dry-wet rale was heard, heart rate was rhythmic, and no pathological murmur was detected.
The relevant blood tests in the outpatient department and after admission are shown in Table 1.
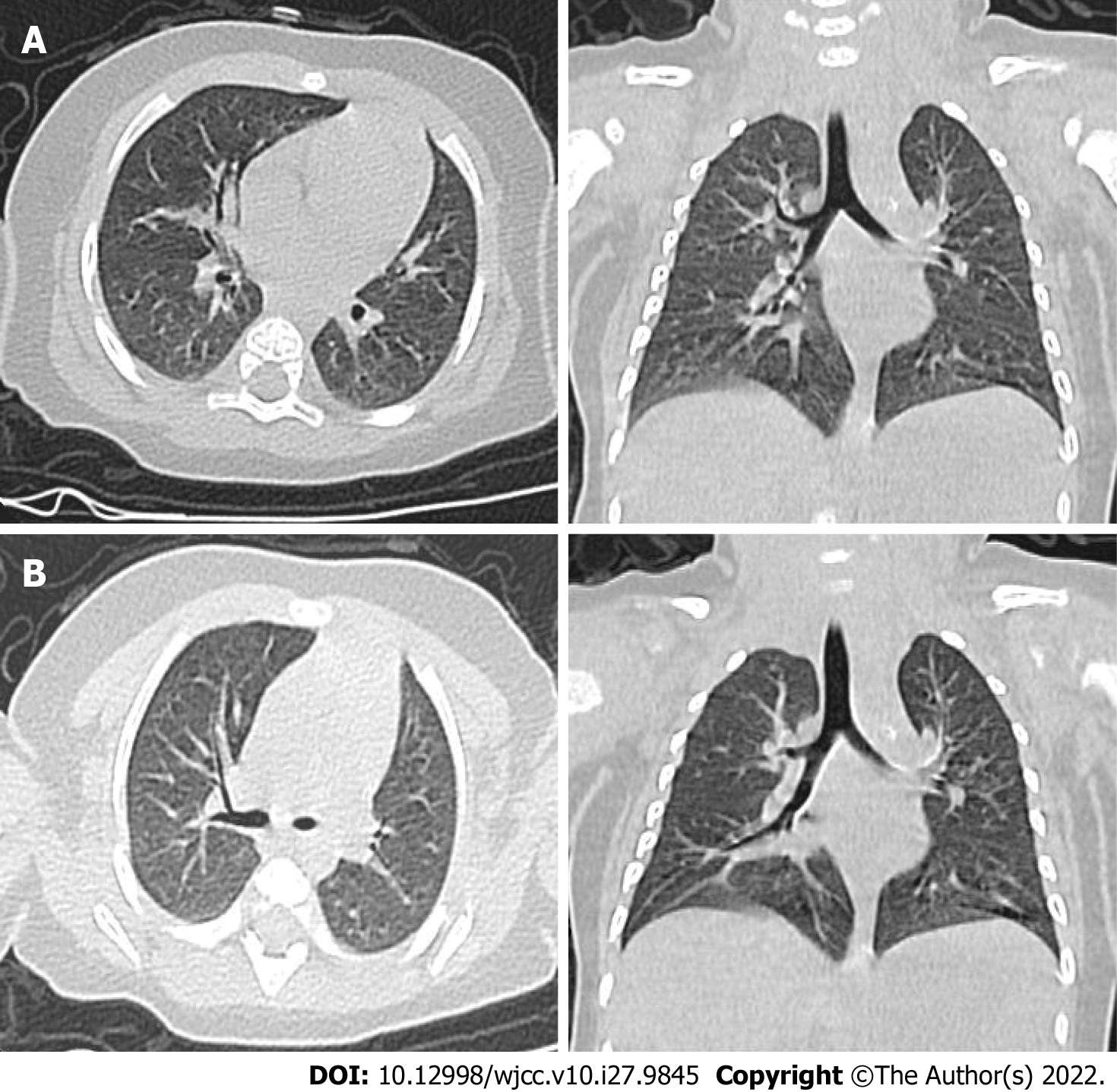
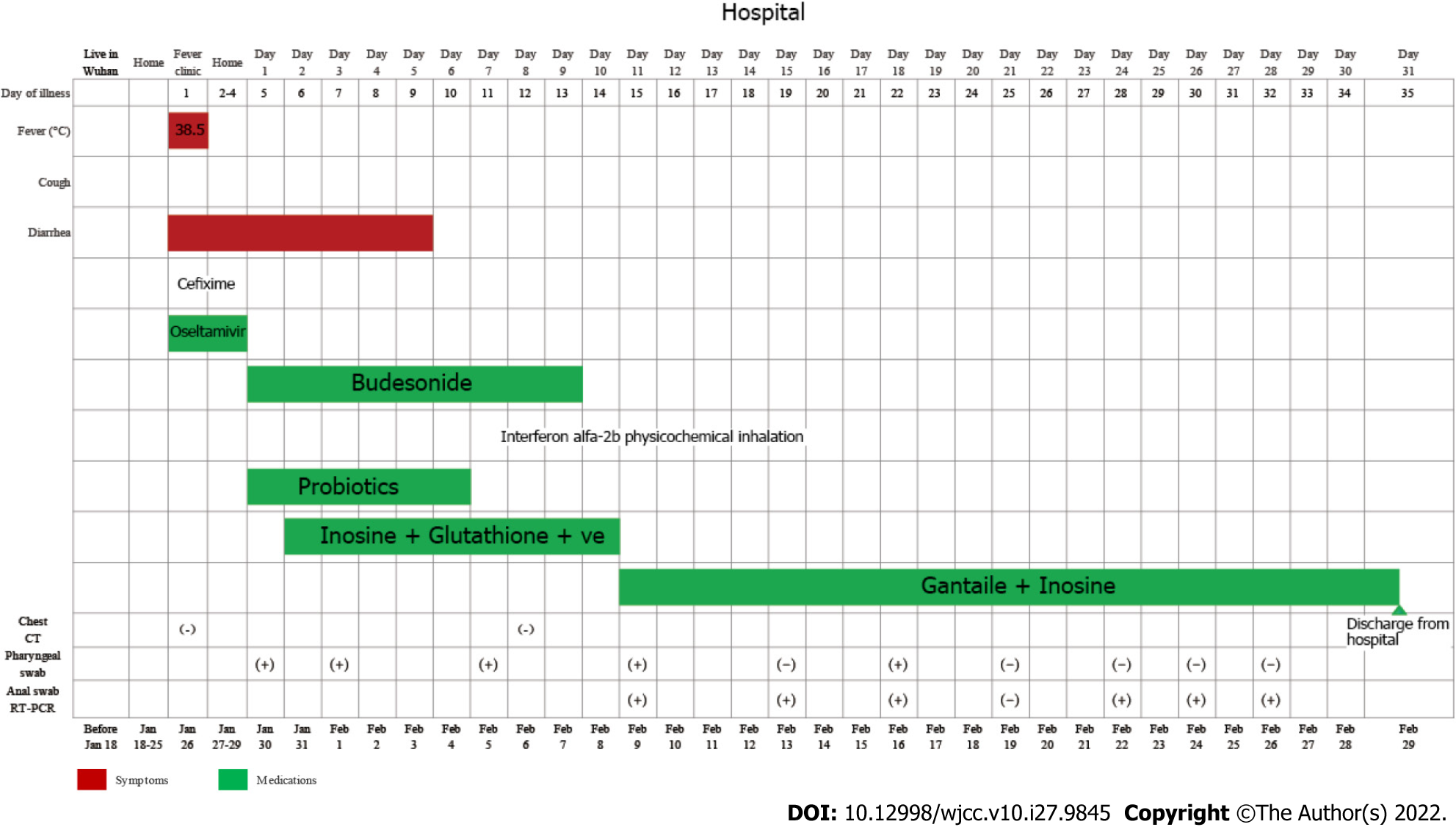
The patient presented with fever and diarrhea. We performed a routine chest CT scan (Figure 1A). After experiential and systematic treatment, fever and diarrhea disappeared on the 6th hospitalization day. However, the RT-PCR result in the nasopharyngeal swab was still positive. For safety, we routinely performed the second chest CT scan (Figure 1B).
Combined with the patient’s medical history and RT-PCR results, the final diagnosis was COVID-19.
After giving cefixime (25 mg/bid, po) and oseltamivir (0.75 mg/bid, po), the infant's body temperature returned to normal; yet, the diarrhea was not still improved on January 28.
After being hospitalized in the pediatric department, the infant was given systematic treatment, including budesonide (1 mg/bid, inh), interferon alfa-2b (140 units/bid, inh), vitamin C (1g/qd, ivdrp), inosine tablets (0.1g/qd, ivdrp), reduced glutathione (0.6g/qd, ivdrp) and probiotics (1g/qd, po). To exclude the possibility of virus transmission by breastfeeding, the breast milk was analyzed by RT-PCR on the 4th hospitalization day, and the results were negative. After systematic treatment, diarrhea disappeared (on the 6th hospitalization day). On the 10th hospitalization day, liver function testing was still abnormal; thus, the attending doctor decided to prescribe hepatoprotective drugs Gantaile tablets (0.1 g/bid, po) and inosine tablets (0.1 g/bid, po). The main symptom, treatment plan, RT-PCR results, and chest CT results of the infant were presented (Figure 2).
On the 31st hospitalization day, all symptoms of the infant were improved significantly (follow-up performed according to the guidelines for the diagnosis and treatment of COVID-19[1]), and the infant was discharged from the hospital.
In view of the fact that the infant was diagnosed with COVID-19 and discharged from the hospital, it is recommended to isolate at home for 14 d and pay attention to personal hygiene and avoid getting cold. The child was required to re-examine the RT-PCR of SARS-CoV-2 in nasopharyngeal and anal swabs after one week, and the liver function after two weeks.
SARS-CoV-2 is primarily transmitted between people via respiratory droplets and contact routes[5]. Lymphopenia occurs in 35%-82.1% of adult patients[3,6]. In this case, lymphocyte count was increased, which was different from the laboratory findings in adult patients. Moreover, ALT, AST, and LDH can be elevated in adult patients, and the proportion of LDH elevation is larger (76%)[6]. The proportion of LDH elevation, in this case, was 45%. Also, according to reports, 86% of adult patients with COVID-19 have elevated CRP, which is a marker of inflammation[6]. Yet, our patient showed normal CRP. The above results show that the clinical manifestations of COVID-19 in infants and young children are different from those seen in adults, which may be related to the fact that children are mostly infected by the second or third-generation virus (the virus virulence is weakened) and due to their lower immune function[7].
The clinical manifestations of children patients are similar to those of adults and mainly include fever and cough. Diarrhea and runny nose have been observed in a few infected children[8]. A recent study[7] suggested that the relatively low reaction of angiotensin-converting enzyme 2 (ACE2), which induces intracellular response in pediatric patients, might be the reason why children present less severe symptoms compared to adults. In this case, the child had a fever and occasional cough lasting for one day. The chest CT examinations were negative in the outpatient department and after admission. Her parents were confirmed with COVID-19; the father had fever and cough; the mother had no respiratory symptoms such as cough, nasal discharge, or shortness of breath. It is important to note that respiratory symptoms may not be a prerequisite for diagnosing COVID-19[9].
SARS-CoV-2 may also cause damage to the heart, liver, kidney, and other organs[2,3]. Mechanistically, SARS-CoV-2 invades human host cells expressing the ACE2 receptor. Although this case tested negative after examining pharyngeal swab on RT-PCR four times (February 19, 22, 24, and 26), the results of anal swab RT-PCR analysis on February 22, 24, and 26 were still positive, which suggested that the virus may invade the digestive system through the ACE2 receptor of the gastrointestinal tract and be transmitted via feces. The current clinical diagnosis and treatment plan suggest that the criteria for discharge from isolation should be a normal temperature for more than 3 days, improved respiratory symptoms, and two consecutively pharyngeal swabs of RT-PCR test negative separated by at least 1 d[1]. Yet, given the persistent positive RT-PCR results of anal swabs (as seen in this case), the possibility of fecal-oral transmission of COVID-19 should also be considered.
Based on the diagnosis and treatment of this case, people of all ages are susceptible to COVID-19, and the degree of susceptibility may be different. In addition, COVID-19 patients may have few or no clinical symptoms, normal chest CT, and even false-negative PR-PCT results. Thus, early chest CT screening, timely follow-up, corresponding pathogen detection, and epidemiological and clinical features analysis should be included in the screening protocol for children with COVID-19. Early diagnosis, isolation, and treatment of COVID-19 are critical for controlling this pandemic.
We would like to thank the patient and our colleagues for participating in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emran TB, Bangladesh; Hueda-Zavaleta M, Peru S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | National Health Commission of the People's Republic of China. The guidlines for the diagnosis and treatment of 2019-nCoV pneumonia (the 7th edition) [cited 3 Mar 2020]. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf.. |
| 2. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14766] [Article Influence: 2953.2] [Reference Citation Analysis (0)] |
| 3. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30114] [Article Influence: 6022.8] [Reference Citation Analysis (3)] |
| 4. | Jiehao C, Jin X, Daojiong L, Zhi Y, Lei X, Zhenghai Q, Yuehua Z, Hua Z, Ran J, Pengcheng L, Xiangshi W, Yanling G, Aimei X, He T, Hailing C, Chuning W, Jingjing L, Jianshe W, Mei Z. A Case Series of Children With 2019 Novel Coronavirus Infection: Clinical and Epidemiological Features. Clin Infect Dis. 2020;71:1547-1551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 422] [Cited by in RCA: 553] [Article Influence: 110.6] [Reference Citation Analysis (0)] |
| 5. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9317] [Article Influence: 1863.4] [Reference Citation Analysis (0)] |
| 6. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12973] [Article Influence: 2594.6] [Reference Citation Analysis (1)] |
| 7. | Fang F, Luo XP. [Facing the pandemic of 2019 novel coronavirus infections: the pediatric perspectives]. Zhonghua Er Ke Za Zhi. 2020;58:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 8. | Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: Different points from adults. Pediatr Pulmonol. 2020;55:1169-1174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 683] [Cited by in RCA: 636] [Article Influence: 127.2] [Reference Citation Analysis (0)] |
| 9. | Del Rio C, Malani PN. 2019 Novel Coronavirus-Important Information for Clinicians. JAMA. 2020;323:1039-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |