Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9790
Peer-review started: April 14, 2022
First decision: June 7, 2022
Revised: June 20, 2022
Accepted: August 16, 2022
Article in press: August 16, 2022
Published online: September 26, 2022
Processing time: 155 Days and 0.9 Hours
Synchronous primary cancers (SPCs) have become increasingly frequent over the past decade. However, the coexistence of duodenal papillary and gallbladder cancers is rare, and such cases have not been previously reported in the English literature. Here, we describe an SPC case with duodenal papilla and gallbladder cancers and its diagnosis and successful management.
A 68-year-old Chinese man was admitted to our hospital with the chief complaint of dyspepsia for the past month. Contrast-enhanced computed tomography of the abdomen performed at the local hospital revealed dilatation of the bile and pancreatic ducts and a space-occupying lesion in the duodenal papilla. Endoscopy revealed a tumor protruding from the duodenal papilla. Pathological findings for the biopsied tissue revealed tubular villous growth with moderate heterogeneous hyperplasia. Surgical treatment was selected. Macroscopic examination of this surgical specimen revealed a 2-cm papillary tumor and another tumor protruding by 0.5 cm in the gallbladder neck duct. Intraoperative rapid pathology identified adenocarcinoma in the gallbladder neck duct and tubular villous adenoma with high-grade intraepithelial neoplasia and local canceration in the duodenal papilla. After an uneventful postoperative recovery, the patient was discharged without complications.
It is essential for clinicians and pathologists to maintain a high degree of suspicion while evaluating such synchronous cancers.
Core Tip: Synchronous primary cancers (SPCs) of the duodenal papilla and gallbladder are rarely reported. Here, we report such a case. The lesion in the duodenal papilla was discovered by imaging examination of a 68-year-old man. Endoscopic biopsy was performed, and the pathological findings revealed moderate heterogeneous hyperplasia. The patient underwent pancreaticoduodenectomy, and intraoperative rapid histopathological examination surprisingly revealed adenocarcinoma in the papillary region and another adenocarcinoma in the gallbladder neck duct. SPC involving both the gallbladder and duodenal papilla is regarded as a rare occurrence. It is essential for the clinician and pathologist to maintain a high degree of suspicion while evaluating such lesions.
- Citation: Chen J, Zhu MY, Huang YH, Zhou ZC, Shen YY, Zhou Q, Fei MJ, Kong FC. Synchronous primary duodenal papillary adenocarcinoma and gallbladder carcinoma: A case report and review of literature. World J Clin Cases 2022; 10(27): 9790-9797
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9790.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9790
With the widespread improvement in early diagnosis and regular medical check-ups, the occurrence of synchronous primary cancers (SPCs) has become increasingly frequent over the past decade[1]. However, it is very rare for duodenal papillary and gallbladder cancers to coexist, and no cases have been reported in the English literature. Here, we describe a case of SPC of the duodenal papilla and gallbladder and its diagnosis and successful management.
A 68-year-old Chinese man was admitted to a local hospital with the chief complaint of dyspepsia.
The patient’s symptoms started a month prior to dyspepsia.
The patient had a history of distal gastric resection with Billroth II anastomosis for a bleeding marginal ulcer 30 years ago.
The patient denied any family history.
After hospitalization, the patient’s temperature was 37°C, heart rate was 88 beats per minute, respiratory rate was 19 breaths per minute, blood pressure was 127/79 mmHg and oxygen saturation in room air was 100%. The clinical examination showed no pathological signs.
Blood tests, including tumor markers, showed that levels were completely normal except for glutamyl transpeptidase (GGT; 379 U/L, normal: 10-60 U/L) and alkaline phosphatase (ALP; 174 U/L, normal: 45-125 U/L).
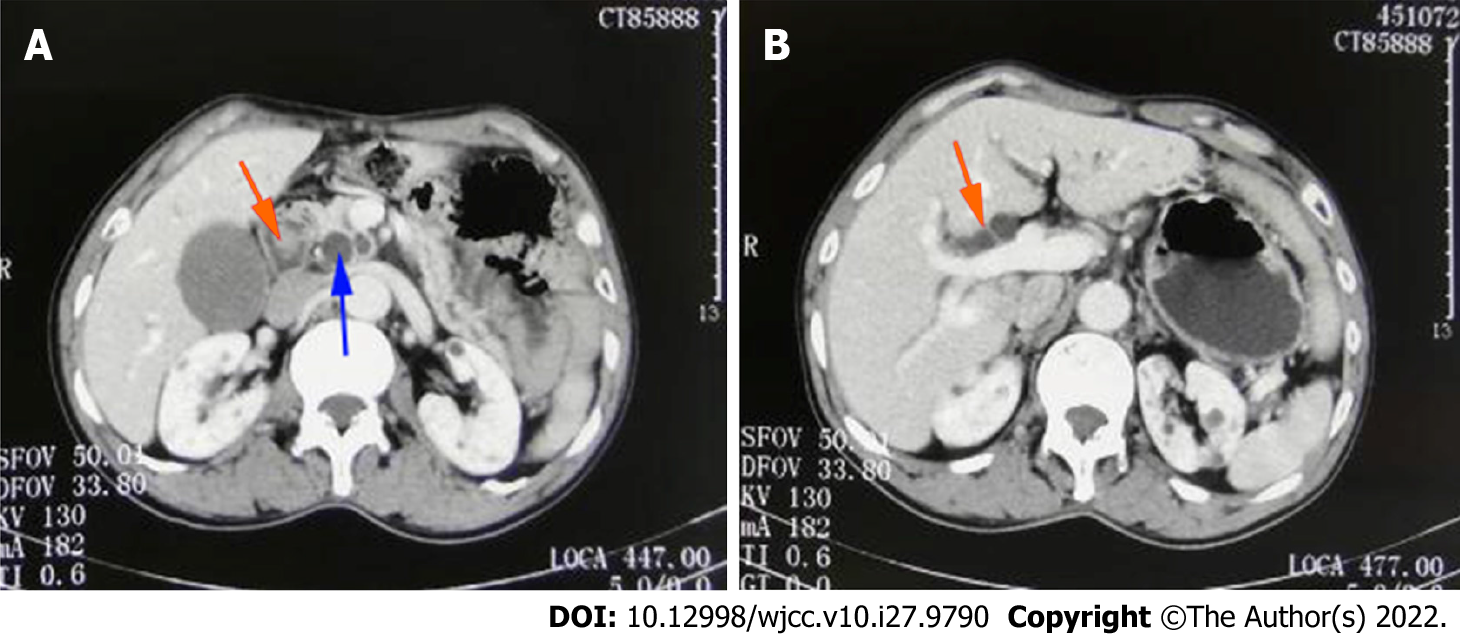
Contrast-enhanced computed tomography of the upper abdomen performed at the local hospital revealed dilatation of the intrahepatic bile duct, common bile duct and pancreatic duct and a space-occupying lesion in the duodenal papilla (Figure 1).
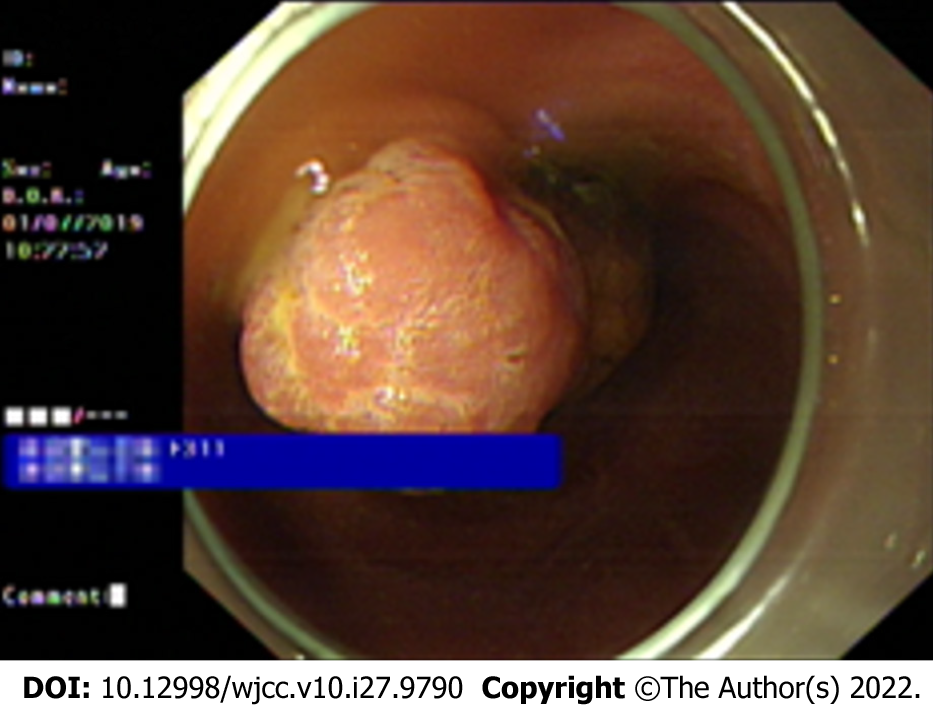
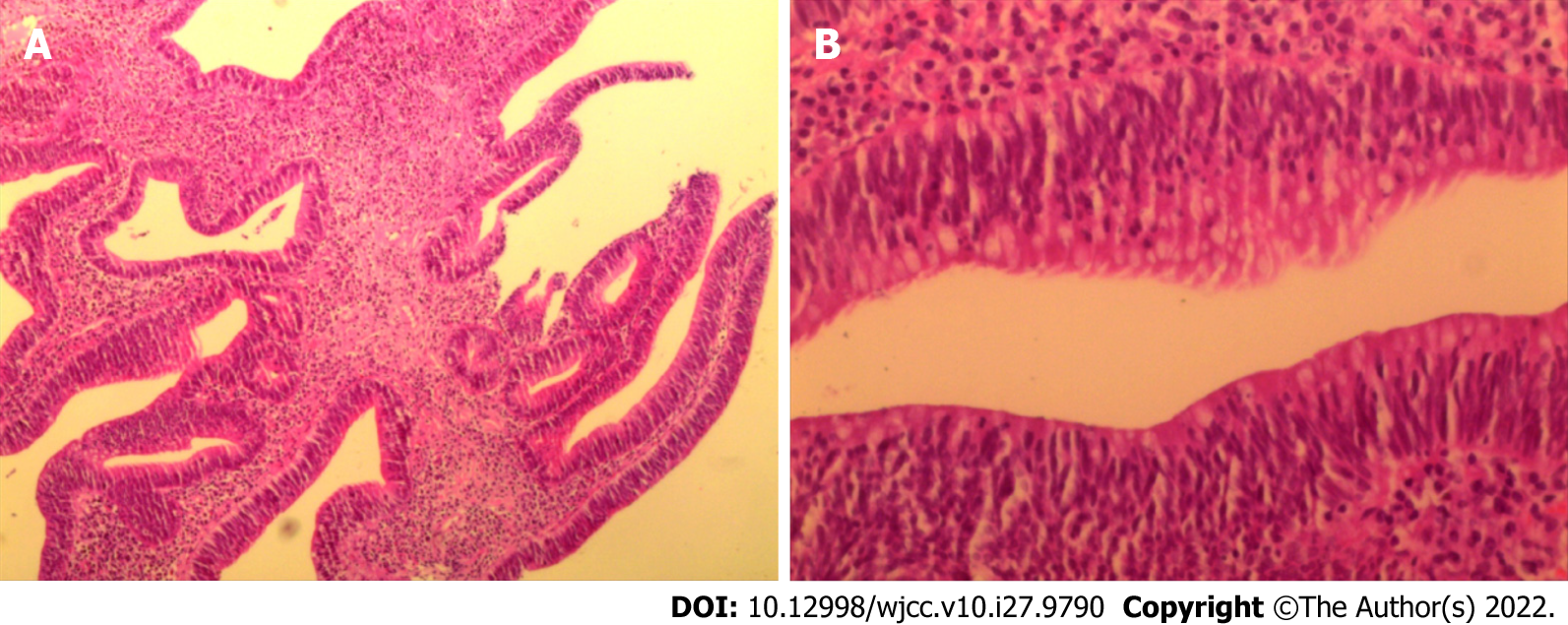
Endoscopic biopsy was performed because of the unclear nature of this occupancy. Endoscopy showed a tumor protruding from the duodenal papilla (Figure 2), and the pathological findings revealed that the biopsy tissue presented tubular villous growth with moderate heterogeneous hyperplasia (Figure 3).
Based on the above physical examination features and imaging data, a provisional diagnosis of space-occupying lesion in the duodenal papilla was made. After surgical resection, the final diagnoses were gall bladder adenocarcinoma and duodenal papilla adenocarcinoma.
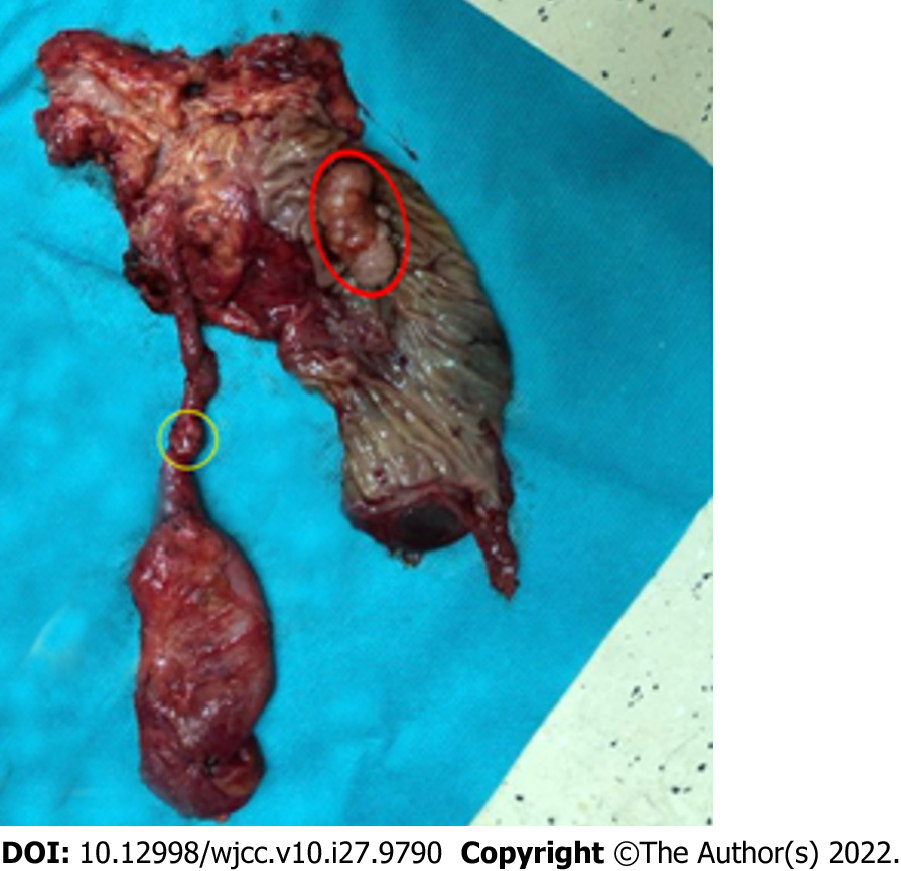
Since malignancy of the space-occupying lesion in the duodenal papilla could not be ruled out, surgical treatment was selected after communication with the patient and his family members. The patient was informed of the possible risks involved in this surgery before consent for the operation was obtained. Based on a careful preoperative evaluation and no obvious findings of contraindications of the surgery, the patient underwent a pancreaticoduodenectomy (Whipple’s procedure) on July 11, 2019. Macroscopic examination of this surgical specimen revealed a 2-cm papillary tumor and another tumor with a 0.5-cm protrusion in the gallbladder neck duct (Figure 4). Intraoperative rapid pathology revealed adenocarcinoma without basement membrane breakthrough in the gallbladder neck duct and tubular villous adenoma with high-grade intraepithelial neoplasia and local canceration in the duodenal papilla. The examination also showed that no metastases were found in the resected lymph nodes. The cooccurrence of duodenal papillary and gallbladder cancers is very rare. The two tumors were independent of each other, and there was no relationship with metastasis.
The final pathological tumor stage was pT1bN0M0 for adenocarcinoma of the gall bladder and pT1N0M0 for adenocarcinoma of the duodenal papilla, and the patient was not provided adjuvant therapy. After an uneventful recovery, the patient was discharged without complications on postoperative Day 20. After one year, he was followed up by us, and there was no evidence of tumor recurrence.
The most common synchronous cancers are colorectum (37.2%), lung (18.6%), esophagus (16.8%), liver (9.7%), kidney (4.4%) and stomach (3.4%)[2]. The simultaneous occurrence of multiple cancers in the papilla of Vater and ampulla of Vater is rare, with approximately 7 cases and 14 cases, respectively, reported thus far in the English-language medical literature[3-21] (Table 1). However, this report is the first to detail the SPC of the duodenal papilla and gallbladder. The incidence of SPC from the biliary tree has been reported to vary from 5.0 to 7.4%[22], and it is important to distinguish between SPC and secondary deposits. The following diagnostic criteria have been adopted by most clinicians to differentiate synchronous primaries from malignant deposits: (1) Lack of anatomical continuity between two tumors; (2) a growth pattern typical of a primary tumor; and (3) clear histological differences between two tumors[23,24]. According to the above criteria, this case was determined to be SPC. Ultimately, both the gallbladder and duodenal papilla were labeled as primary adenocarcinomas by the pathologist as they had histological differences and a growth pattern typical of a primary tumor.
| Cases | Age (yr)/Sex | Tumor location | Treatment | Prognosis (mo) |
| Ueno et al[3] | 58/M | Common bile duct, gallbladder, papilla of Vater (severe dysplasia) | Surgical resection | 30/Disease-free survival |
| Seo et al[4] | 42/F | Major and minor duodenal papilla of Vater | Endoscopic papillectomy | 16/Disease-free survival |
| Parthasarathy et al[5] | 60/F | Major and minor duodenal papilla of Vater | Surgical resection | 8/Disease-free survival |
| Matheus et al[6] | 50/F | Major and minor duodenal papilla of Vater | Surgical resection | 24/Disease-free survival |
| Tamura et al[7] | 78/M | Lung, papilla of Vater | Surgical resection | 60/Disease-free survival |
| Takahashi et al[8] | 66/M | Erythroleukemia,stomach, papilla of Vater | Jejuno-choledochostomy | N/A |
| Nishihara et al[9] | 53/M | common bile duct, pancreas,papilla of Vater | Surgical resection | N/A |
| de Garcia de la Vega et al[10] | 77/M | Esophagus, ampulla of Vater | Surgical resection | 24/Recurrence due to liver metastasis |
| Sastry et al[11] | 81/M | Pancreas, ampulla of Vater | Surgical resection | 10/Die of liver metastasis |
| Cokmert et al[12] | 63/F | sigmoid colon, ampulla of Vater | Surgical resection | N/A |
| Fukaya et al[13] | 69/M | esophagus, stomach, ampulla of Vater | Surgical resection | 12/Die of progressive disease |
| Wohlauer et al[14] | 76/M | common bile duct, ampulla of Vater | Surgical resection | N/A |
| Rajalingam et al[15] | 72/M | right colon, ampulla of Vater | Surgical resection | 8/Disease-free survival |
| Aurello et al[16] | 33/F | Duodenum, ampulla of Vater | Surgical resection | 24/Disease-free survival |
| Athanasopoulos et al[17] | 43/M | common bile duct, ampulla of Vater | Surgical resection | 18/Disease-free survival |
| Eriguchi et al[18] | 83/M | Stomach, ampulla of Vater | Surgical resection | 3/Disease-free survival |
| Eriguchi et al[18] | 74/M | Colon, ampulla of Vater | Surgical resection | 24/ Die of liver metastasis |
| Eriguchi et al[18] | 68/M | Renal pelvis, ampulla of Vater | Surgical resection | 14/ Die of progressive disease |
| Mafune et al[19] | 64/M | Esophagus, ampulla of Vater | Surgical resection | 13/Disease-free survival |
| González Sánchez et al[20] | 50/F | Colon, ampulla of Vater | Surgical resection | N/A |
| Yoshida et al[21] | 58/M | Sigmoid colon, ampulla of Vater | Surgical resection | N/A |
To date, the pathogenesis of SPC has not been elucidated. Several factors are involved, including genetic factors, environmental carcinogens, hormones, dietary factors, previous therapy, infective agents, smoking and alcohol use[25,26]. First, gallbladder cancer may be caused by infectious agents or gallstones due to chronic inflammation and recurrent trauma[27,28]. A reasonable assumption indicates that chronic irritation of the mucosa leads to dysplasia and causes malignant changes[29]. Additionally, 62.5% of SPCs of the biliary tract have been reported to be associated with abnormal pancreaticobiliary junction (APBJ) caused by persistent reflux of pancreatic juice with subsequent biliary inflammation[30-32]. In our case, the cystic duct was too long and had low confluence with the common bile duct. An excessively long cystic duct is adverse to bile outflow, and the duct can be easily blocked and infected by gram-negative bacilli. Eventually, these factors may lead to tumorigenesis. Second, duodenal papillary adenocarcinoma is a relatively uncommon malignant tumor that accounts for less than 1% of all gastrointestinal cancers[33]. Smoking is an important risk factor, and chronic infection and heredity are considered important susceptibility factors[18]. In the process of canceration, mutations in genes such as K-ras, p53 and p21/Waf1 play an important role[34,35].
Preoperative diagnosis of duodenal papilla occupancy is useful for making therapeutic decisions. Endoscopic biopsy has become a popular diagnostic tool and is used in a diverse range of digestive tract diseases. Histopathology from biopsy remains the gold standard for diagnosis. The positive rate of endoscopic biopsy is low, although the diagnostic value of the endoscopic appearance seems to be superior to that of endoscopic biopsy[36]. In the study case, endoscopy revealed a tumor protruding from the duodenal papilla, and endoscopic biopsy did not diagnose a malignant tumor. These findings demonstrated the importance of the endoscopic description of duodenal papilla. In addition, we were unable to diagnose this gallbladder carcinoma preoperatively. The presence of SPC was a histological surprise.
Few reports have focused on the treatment of patients with this rare disease, which remains a key challenge[37]. Curative resection, if possible, is the most effective method of prolonging patient survival. It is also important to note that surgical procedures may not necessarily lead to better prognosis in patients with SPC. Hepatopancreatoduodenectomy is indicated in locally advanced GBC patients with extensive retropancreatic lymphadenopathy that cannot be cleared without pancreatoduodenectomy. Moreover, HPD is associated with significant morbidity, with an overall major complication rate of approximately 50%. Thus, avoiding extensive hepatectomy has reduced morbidity after HPD[38,39].
In this case, a malignant tumor of the duodenal papilla could not be excluded, and the patient successfully underwent pancreaticoduodenectomy. To our surprise, adenocarcinoma of the gallbladder neck duct and involvement in the muscularis were discovered. Because the cystic duct presents low confluency with the common bile duct and the tumor was located on the gallbladder neck duct, no further treatment was needed, and an R0 resection was achieved with the classical Whipple’s procedure. After an uneventful postoperative recovery, the patient was discharged without complications. The follow-up data 1 year after the operation were collected, and no tumor recurrence or metastasis was found.
SPC involving both the gallbladder and duodenal papilla is regarded as a rare occurrence but is becoming increasingly common during hepatobiliary surgery. It is essential for clinicians and pathologists to maintain a high degree of suspicion while evaluating these lesions and to look for the existence of APBJ. At the same time, it is necessary to develop a more accurate diagnostic tool and implement more refined treatment strategies to correctly diagnose SPC.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hasan A, Egypt; Rakić M, Croatia S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Jin K, Xu J, Chen J, Chen M, Chen R, Chen Y, Chen Z, Cheng B, Chi Y, Feng ST, Fu D, Hou B, Huang D, Huang H, Huang Q, Li J, Li Y, Liang H, Lin R, Liu A, Liu J, Liu X, Lu M, Luo J, Mai G, Ni Q, Qiu M, Shao C, Shen B, Sheng W, Sun J, Tan C, Tan H, Tang Q, Tang Y, Tian X, Tong D, Wang X, Wang J, Wang W, Wang Y, Wu Z, Xue L, Yan Q, Yang N, Yang Y, Yang Z, Yin X, Yuan C, Zeng S, Zhang R, Yu X. Surgical management for non-functional pancreatic neuroendocrine neoplasms with synchronous liver metastasis: A consensus from the Chinese Study Group for Neuroendocrine Tumors (CSNET). Int J Oncol. 2016;49:1991-2000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Lee JH, Bae JS, Ryu KW, Lee JS, Park SR, Kim CG, Kook MC, Choi IJ, Kim YW, Park JG, Bae JM. Gastric cancer patients at high-risk of having synchronous cancer. World J Gastroenterol. 2006;12:2588-2592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Ueno G, Ishikawa S, Ichikawa Y, Hagi T, Taniura N, Chong H, Kanazawa A, Takayama S, Nishihara M, Maruyama K, Shimada M, Lee K, Oka H, Maeda T. [A case of synchronous cancer of the gall bladder, common bile duct, and the papilla of vater]. Gan To Kagaku Ryoho. 2014;41:1521-1523. [PubMed] |
| 4. | Seo YK, Choi JS. Endoscopic Papillectomy for Synchronous Major and Minor Duodenal Papilla Neuroendocrine Tumors. Korean J Gastroenterol. 2018;72:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Parthasarathy S, Pottakkat B, Yootla M, Reddy SN, Reddy KM. Synchronous adenocarcinomas of the papilla major and minor. JOP. 2008;9:332-334. [PubMed] |
| 6. | Matheus AS, Jukemura J, Montagnini AL, Kunitake T, Patzina RA, da Cunha JE. Synchronous adenocarcinoma of the major and minor duodenal papilla. J Gastrointest Surg. 2008;12:1301-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Tamura K, Takamori S, Hayashi A, Miwa K, Fukunaga M, Maeshiro K, Nakamura H, Tamae T, Isomoto H, Shirouzu K. Resection of synchronous lung and Vater's papilla cancer. Kurume Med J. 2003;50:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 8. | Takahashi T, Kazama Y, Shimizu H, Yoshimoto M, Tsujisaki M, Aoki S, Imai K. Myelodysplastic syndrome progresses rapidly into erythroleukemia associated with synchronous double cancers of the stomach and the papilla of Vater. Int J Hematol. 2001;74:64-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Nishihara K, Tsuneyoshi M, Shimura H, Yasunami Y. Three synchronous carcinomas of the papilla of Vater, common bile duct and pancreas. Pathol Int. 1994;44:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | de Garcia de la Vega M, Faber B, Schalbar C, Foxius A, Groot-Koerkamp H, Decker G. Combined one-stage esophagectomy and duodeno-pancreatectomy for synchronous cancers of the esophagus and pancreatic ampulla in an elderly patient. Acta Chir Belg. 2021;121:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Sastry A, Wayne M, Steele J, Iskandar M, Yuan S, Cooperman AM. Three synchronous, sporadic and separate periampullary and pancreatic tumors: more than a coincidence? World J Surg Oncol. 2014;12:382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Cokmert S, Demir L, Akder Sari A, Kucukzeybek Y, Can A, Akyol M, Bayoglu IV, Dirican A, Erten C, Tarhan MO. Synchronous appearance of a high-grade neuroendocrine carcinoma of the ampulla vater and sigmoid colon adenocarcinoma. Case Rep Oncol Med. 2013;2013:930359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Fukaya M, Abe T, Yokoyama Y, Itatsu K, Nagino M. Two-stage operation for synchronous triple primary cancer of the esophagus, stomach, and ampulla of Vater: report of a case. Surg Today. 2014;44:967-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Wohlauer MV, McManus MC, Brauer B, Hedges J, Gajdos C. Synchronous presentation of ampullary adenocarcinoma and common bile duct cancer: report of a case and review of literature. JOP. 2012;13:536-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Rajalingam R, Javed A, Gondal R, Arora A, Nag HH, Agarwal AK. Non-familial double malignancy of the colon and ampulla of Vater: a case report and review of literature. Saudi J Gastroenterol. 2012;18:143-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Aurello P, Petrucciani N, D'Angelo F, Nigri G, Picchetto A, Cicchini C, Maglio R, Ramacciato G. Synchronous signet-ring cell carcinoma of the duodenum and ampullary intestinal-type carcinoma. Am Surg. 2011;77:E262-E264. [PubMed] |
| 17. | Athanasopoulos PG, Arkadopoulos N, Stafyla V, Tympa A, Kairi E, Ryzman-Louloudis C, Smyrniotis V. A rare combination of an endocrine tumour of the common bile duct and a follicular lymphoma of the ampulla of Vater: a case report and review of the literature. World J Surg Oncol. 2011;9:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Eriguchi N, Aoyagi S, Tamae T, Nishimura K, Hamada S, Kawabata M, Kodama T, Jimi A. Carcinoma of the ampulla of Vater associated with other organ malignancies. Kurume Med J. 2001;48:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Mafune K, Tanaka Y, Ma YY, Takubo K. Synchronous cancers of the esophagus and the ampulla of Vater after distal gastrectomy: successful removal of the esophagus, gastric remnant, duodenum, and pancreatic head. J Surg Oncol. 1995;60:277-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | González Sánchez JA, López-Ríos Fernández F, González Conde R, Miguel Velasco JE, Casas Pinillos MS, Larrauri Martínez J. [Carcinoma of the Vater's ampulla and colonic carcinoma with synchronous onset]. Rev Esp Enferm Dig. 1993;83:459-461. [PubMed] |
| 21. | Yoshida J, Morisaki T, Yamaguchi K, Itoh T, Yokohata K, Kishikawa H, Iino H. Carcinoma in adenoma of the ampulla of Vater synchronous with cancer of the sigmoid colon. Dig Dis Sci. 1990;35:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Kodaganur S, Hosamani IR. Synchronous malignancies of the gall bladder and common bile duct: a case report. World J Surg Oncol. 2016;14:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Gertsch P, Thomas P, Baer H, Lerut J, Zimmermann A, Blumgart LH. Multiple tumors of the biliary tract. Am J Surg. 1990;159:386-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Demandante CG, Troyer DA, Miles TP. Multiple primary malignant neoplasms: case report and a comprehensive review of the literature. Am J Clin Oncol. 2003;26:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 164] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 25. | Park SL, Caberto CP, Lin Y, Goodloe RJ, Dumitrescu L, Love SA, Matise TC, Hindorff LA, Fowke JH, Schumacher FR, Beebe-Dimmer J, Chen C, Hou L, Thomas F, Deelman E, Han Y, Peters U, North KE, Heiss G, Crawford DC, Haiman CA, Wilkens LR, Bush WS, Kooperberg C, Cheng I, Le Marchand L. Association of cancer susceptibility variants with risk of multiple primary cancers: The population architecture using genomics and epidemiology study. Cancer Epidemiol Biomarkers Prev. 2014;23:2568-2578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Kim C, Chon H, Kang B, Kim K, Jeung HC, Chung H, Noh S, Rha S. Prediction of metachronous multiple primary cancers following the curative resection of gastric cancer. BMC Cancer. 2013;13:394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Kim JW, Han JW, Jung SY, Jung JP, Kim JW. Synchronous double primary malignant tumor of the gallbladder and liver: a case report. World J Surg Oncol. 2011;9:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Zhang ZG, Chen Y, Ji R, Zhao YJ, Wang J, Robinson L, Chen XP, Zhang L. Synchronous cancers of gallbladder carcinoma and combined hepatocellular cholangiocarcinoma: an unusual case and literature review. BMC Cancer. 2018;18:1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 556] [Cited by in RCA: 738] [Article Influence: 56.8] [Reference Citation Analysis (0)] |
| 30. | Fujii T, Kaneko T, Sugimoto H, Okochi O, Inoue S, Takeda S, Nagasaka T, Nakao A. Metachronous double cancer of the gallbladder and common bile duct. J Hepatobiliary Pancreat Surg. 2004;11:280-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Hara H, Morita S, Ishibashi T, Sako S, Dohi T, Otani M, Iwamoto M, Inoue H, Tanigawa N. Studies on biliary tract carcinoma in the case with pancreaticobiliary maljunction. Hepatogastroenterology. 2002;49:104-108. [PubMed] |
| 32. | Agarwal N, Kumar S, Sharma S. Synchronous adenocarcinoma of the gall bladder and pancreas in a young woman. Trop Gastroenterol. 2013;34:50-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Tsuji S, Itoi T, Sofuni A, Mukai S, Tonozuka R, Moriyasu F. Tips and tricks in endoscopic papillectomy of ampullary tumors: single-center experience with large case series (with videos). J Hepatobiliary Pancreat Sci. 2015;22:E22-E27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Kimura W, Futakawa N, Zhao B. Neoplastic diseases of the papilla of Vater. J Hepatobiliary Pancreat Surg. 2004;11:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 35. | Fischer HP, Zhou H. Pathogenesis of carcinoma of the papilla of Vater. J Hepatobiliary Pancreat Surg. 2004;11:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 36. | DeOliveira ML, Triviño T, de Jesus Lopes Filho G. Carcinoma of the papilla of Vater: are endoscopic appearance and endoscopic biopsy discordant? J Gastrointest Surg. 2006;10:1140-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Cartapatti M, Machado RD, Muller RL, Magnabosco WJ, Santos AC, Chapin BF, Melani A, Talvane A, Tobias-Machado M, Faria EF. Synchronous abdominal tumors: is combined laparoscopic surgery in a single approach a safe option? Int Braz J Urol. 2018;44:483-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Sakamoto Y, Nara S, Kishi Y, Esaki M, Shimada K, Kokudo N, Kosuge T. Is extended hemihepatectomy plus pancreaticoduodenectomy justified for advanced bile duct cancer and gallbladder cancer? Surgery. 2013;153:794-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 39. | Vijayaraj P, Chandrasekar S, Kalayarasan R, Pottakkat B. Double Trouble: Synchronous Adenocarcinoma of Gallbladder and Pancreas. J Gastrointest Cancer. 2018;49:358-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |