Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9734
Peer-review started: May 10, 2021
First decision: June 5, 2021
Revised: June 14, 2021
Accepted: June 30, 2022
Article in press: June 30, 2022
Published online: September 26, 2022
Processing time: 493 Days and 15.6 Hours
Gallbladder hemorrhage is a life-threatening disorder. Trauma (accidental or iatrogenic such as a percutaneous biopsy or cholecystectomy surgery), chole
We report the case of a 76-year-old male patient. An urgent contrast computed tomography scan demonstrated relevant distension of the gallbladder filled with hyperdense non-homogeneous content. The gallbladder walls were of regular thickness. Near the anterior wall a focus of suspected active bleeding was observed. Due to the progressive decrease in hemoglobin despite three blood transfusions, this was an indication for urgent surgery.
Early diagnosis of this potentially fatal pathology is essential in order to plan a strategy and eventually proceed with urgent surgical treatment.
Core Tip: Gallbladder hemorrhage is an uncommon life-threatening disorder. There are many causes of this condition: trauma, cholelithiasis, biliary tract parasitosis, vasculitis, vascular malformations, autoimmune and neoplastic diseases and coagulopathies. We report the case of a 76-year-old male patient. An urgent contrast computed tomography scan demonstrated relevant distension of the gallbladder filled with hyperdense non-homogeneous content and a focus of suspected active bleeding. The patient underwent urgent surgery to stop the hemorrhage. Early diagnosis of this insidious and potentially fatal pathology is essential to plan the best treatment strategy for patients.
- Citation: Valenti MR, Cavallaro A, Di Vita M, Zanghi A, Longo Trischitta G, Cappellani A. Gallbladder hemorrhage–An uncommon surgical emergency: A case report. World J Clin Cases 2022; 10(27): 9734-9742
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9734.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9734
Gallbladder hemorrhage is a rare condition, which can be difficult to diagnose. It manifests symptoms present in other more common pathologies, such as fever, nausea, abdominal pain, and Murphy's sign. Trauma (accidental or iatrogenic such as a percutaneous biopsy or cholecystectomy surgery), cho
The patient complained of abdominal pain and constipation.
We report the case of a 76-year-old male patient who attended the emergency room due to abdominal pain and constipation.
In the anamnesis he presented osteoporosis, parkinsonism, vertebral stabilization (metal plates and screws) for L2-L3 arthrodesis (2016), L1-L2 spondylodiscitis, chronic pain in the lumbar region, stiffness in the upper limbs and lower limbs, small steps and impairment of the extensor muscles of the spinal column with bent spine syndrome. In July 2020, due to trauma, he attended the emergency room, where, lacking diagnostic evidence, he was discharged and transferred to a rehabilitation institution. He had been taking the following drugs for the last few years at home: Pantoprazole, CardioASA, Bromazepam, Durogesic, and Cardicor.
No relevant personal and family history.
On physical examination, the patient appeared oriented, cooperative, eupnoic, malnourished, with muscle atrophy and widespread hypotonia. Abdominal examination demonstrated diffuse abdominal pain. His heart rate was 68 bpm, blood pressure was 120/70 mmHg, and temperature was 36°C.
Blood chemistry showed the following: hemoglobin 11.2 g/dL; white blood cell count 10.790/μL; total bilirubin 0.50 mg/dL; aspartate aminotransferase 40 U/L; alanine aminotransferase 28 U/L; alkaline phosphatase 115 U/L; amylase 406 U/L; C-reactive protein: 150 mg/L.
To assess the suspicion of chronic pancreatitis, the patient underwent abdominal ultrasound, and the pancreas showed multiple calcifications in the parenchyma. Moreover, the aorta demonstrated an irregular caliber with progressive stenosis. This finding required an in-depth study; therefore, CT angiography was performed and the common right artery demonstrated CT signs of dissection and ulcerated atheromatous plaque at the origin. Dilated gallbladder, slightly dilated extrahepatic biliary tract, increased volume in the pancreatic gland with small hypodense formations in the pancreas head (maximum diameter 3 mm) were also highlighted. Due to the finding of ulcerated atheromatous plaque, Fondaparinux 2.5 mg/d was administered as suggested by the vascular surgeon consultant.
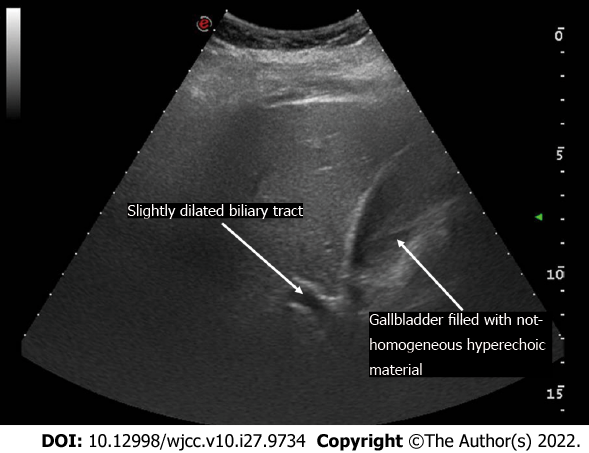
However, the persistence of continuous lumbar pain led the patient to NSAIDs and morphine-like analgesic self-administration, the dosage of which was increased and reduced according to the patient's symptoms relief. Approximately 10 d after Fondaparinux administration, the patient suddenly experienced severe anemia, hyperbilirubinemia, increased cholestasis and transaminase. On physical examination the abdomen was painless. No blood was found in the stool. An urgent abdominal ultrasound, with the patient still in bed, was performed. Evidence of distended gallbladder filled with non-homogeneous hyperechoic material and a slightly dilated intrahepatic biliary tract were observed (Figure 1). The common bile duct was not visible due to intestinal gas.
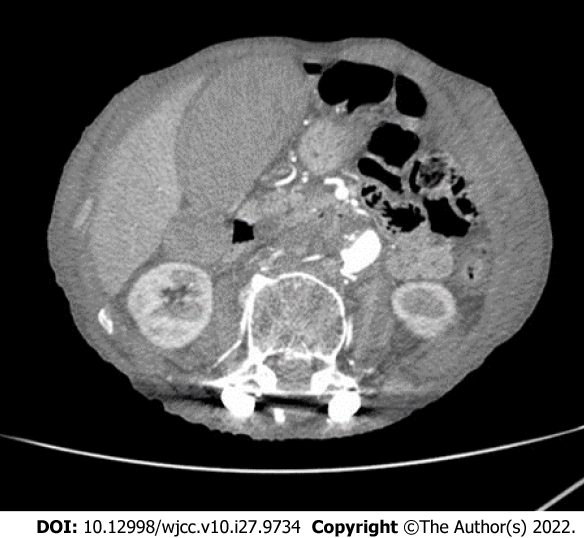
Therefore, the patient underwent an urgent CT scan, which demonstrated relevant distension of the gallbladder filled with hyperdense non-homogeneous content. The gallbladder walls were of regular thickness. Near the anterior wall, a focus of suspected active bleeding was noted. Intra- and extra-hepatic biliary ducts demonstrated wider dilatation when compared to the previous CT scan (Figure 2).
Gallbladder hemorrhage.
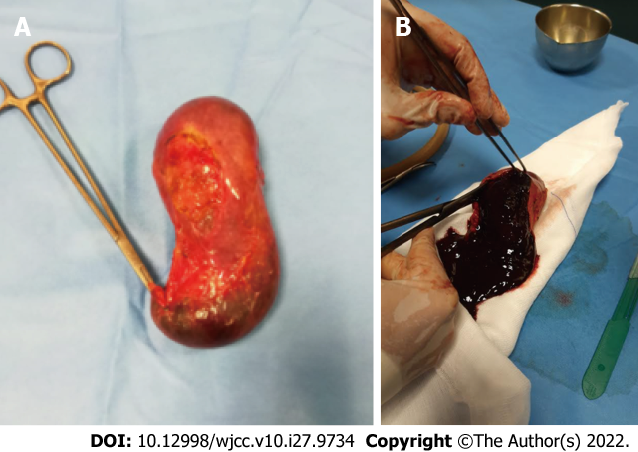
Our hospital is an emergency referring center, with multidisciplinary expertise readily available. An interventional radiological consultation was sought with the aim of evaluating the risk-benefit ratio of cystic artery embolization and/or cholecystostomy. The risk of gallbladder necrosis due to cystic artery occlusion and the risk of hemoperitoneum due to percutaneous drainage led the surgical team to select upfront surgery. The decrease in hemoglobin despite three blood transfusions, coagulation disorders and worsening of his general condition required an effective and timely solution. Therefore, the patient underwent urgent surgery. Open cholecystectomy was performed. Choledocotomy with Kehr tube apposition completed the surgery due to the presence of dilated hepatocoledocus (approximately 25 mm) (Figure 3A). When the gallbladder was inspected at the backtable, it appeared entirely occupied by clots (Figure 3B).
A further blood transfusion, plasma and supportive medical therapy were administered during the perioperative period. The patient had a regular post-operative course until discharge. The T tube was removed 50 d after surgery. Histological examination demonstrated acute lithiasic cholecystitis without any relevant finding.
Gallbladder hemorrhage is a rare complication of cholelithiasis, and is difficult to diagnose due to the non-specificity of the symptoms, which may easily lead to possible thoracic aortic dissection for back pain or acute cholecystitis for right hypochondrium pain. It can also manifest with fever, nausea, jaundice, melena and increased indices of inflammation and markers of liver damage in blood tests (neutrophilic leukocytosis, hypertransaminasemia, hyperbilirubinemia)[1-4].
Among the causes of gallbladder hemorrhage, trauma, neoplasms of the biliary tract, lithiasic cholecystitis, parasitosis, vasculitis, autoimmune diseases, and primary or secondary coagulopathies (e.g., liver cirrhosis, renal failure) have been reported[5-10]. Most patients diagnosed with gallbladder hemorrhage have comorbidities and most take anticoagulants and NSAIDs. To date, approximately 51 case reports have been reported in the literature since 1980[5]. We performed a brief revision of the cases reported in the literature, and their treatment strategies (Table 1). Among the reports, over 80% of patients underwent surgery with cholecystectomy. Of these, 6/45 patients underwent elective laparoscopic cholecystectomy after conservative treatment. Open surgery was dominant in the urgent setting (24 vs 15 patients), and we could hypothesize that this surgical technique was chosen with the aim of better evaluation and control of extra-gallbladder sources of hemorrhage.
| Ref. | Journal | Patient age/gender | Anti-coagulation | Treatment choice |
| Nguyen D et al[16], 2021 | Journal of Radiology Case Reports | N | Cystic artery embolization, cholecystectomy | |
| Chen X et al[17], 2021 | Hepatobiliary Surgery and Nutrition | 63 F | Not mentioned | ERCP and ENBD, cholecystectomy |
| Leaning[18], 2021 | Journal of Surgical Case Reports | 73 M | Y-Apixaban | Laparoscopic Cholecystectomy |
| Azam et al[19], 2021 | Journal of the National Medical Association | 55 M | Y-Apixaban | Cholecystectomy |
| Yam et al[2], 2020 | Radiology Case Reports | 51 F | N | Cystic artery embolization, cholecystostomy, open cholecystectomy |
| Gomes et al[20], 2020 | BMJ Case Reports | 87 M | Y-Aspirin | Open cholecystectomy |
| Kishimoto et al[21], 2020 | Gan To Kagaku Ryoho. Cancer and Chemotherapy | 96 F | N | Laparoscopic cholecystectomy |
| Tarazi et al[5], 2019 | Journal of Surgical Case Reports | 87 M | Y-Warfarin | Cholecystostomy |
| 65 F | Y-Warfarin | Conservative with IV antibiotics | ||
| 92 F | N | Cholecystostomy | ||
| Reens et al[22], 2019 | The Journal of Emergency Medicine | 76 M | Y-Warfarin | Cholecystostomy |
| Itagaki et al[23], 2019 | Journal of Medical Case Reports | 86 F | Y-Edoxaban | Conservative with IV antibiotics, elective laparoscopic cholecystectomy |
| Honda et al[24], 2019 | Journal of Clinical Rheumatology: practical reports on rheumatic & musculoskeletal diseases. | 71 M | N | Laparoscopic cholecystectomy |
| San Juan López C et al[25], 2019 | Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patología Digestiva. | 55 M | N | Laparoscopic cholecystectomy |
| Ng et al[26], 2018 | BMJ Case Reports | 68 F | N | Open cholecystectomy |
| Liefman et al[27], 2018 | International Annals of Medicine | 73 F | Y–Rivaroxaban | Conservative with IV antibiotics, elective laparoscopic cholecystectomy |
| López et al[28], 2018 | Radiology | 84 M | Not mentioned | Laparoscopic cholecystectomy |
| Berndtson et al[29], 2017 | Surgical Infections Case Reports | 75 F | N | Open cholecystectomy |
| Choi et al[30], 2017 | Trauma Image and Procedure | 65 M | N | Laparotomy + open cholecystectomy |
| Kinnear et al[31], 2017 | BMJ Case Reports | 74 M | Y- Apixaban | Laparotomy + open cholecystectomy |
| Sishida et al[32], 2017 | Case Reports in Gastroenterology | 79 M | Y-Heparin for dialysis | ERCP and ENBD |
| Oshiro et al[33], 2017 | International Surgery | 61 F | Y – Warfarin | Conservative with IV antibiotics, elective laparoscopic cholecystectomy |
| Yoshida et al[34], 2017 | J-Stage | 73 M | Y | Laparoscopic cholecystectomy |
| Tsai et al[35], 2016 | Medicine | 80 M | N | Cholecystostomy, elective laparoscopic cholecystectomy |
| Calvo Espino et al[36], 2016 | Cirugía Española | 59 M | N | Laparotomy + Open cholecystectomy |
| Cho et al[37], 2015 | Korean Journal of Thoracic and Cardiovascular Surgery | 61 M | Y-Warfarin | Cholecystostomy drainage |
| Aljiffry et al[38], 2014 | Journal of Surgical Case Reports | 57 M | N | Cystic artery embolization + open cholecystectomy |
| Onozawa et al[39], 2014 | International Surgery | 58 F | N | Laparoscopic cholecystectomy |
| Matsukiyo et al[40], 2014 | J-Stage | 68 F | Y-thrombolysis | Laparotomy + open cholecystectomy |
| Seok et al[41], 2013 | Korean Journal of Internal Medicine | 84 M | N | Laparoscopic cholecystectomy |
| Taniguchi et al[42], 2013 | J-Stage | 48 M | Y-Heparin for dialysis | Laparotomy + open cholecystectomy |
| Choi[43], 2012 | Zeitschrift für Gastroenterologie | 36 M | Y-Aspirin and Clopidogrel | Laparoscopic cholecystectomy |
| Kwon et al[1], 2012 | Korean Journal of Hepatobiliary Pancreatic Surgery | 75 M | Y-Warfarin | Laparoscopic cholecystectomy |
| Perez et al[10], 2011 | Revista Española De Enfermedades digestivas | 24 F | N | Laparoscopic to open cholecystectomy + intra-operative cholangiography |
| Jung et al[44], 2011 | Journal of the Korean Surgical Society | 55 M | N | Laparoscopic cholecystectomy |
| Parekh et al[7], 2010 | JAMA Surgery | 60 M | N | ERCP + Laparoscopic cholecystectomy |
| 50 M | N | Laparoscopic to open cholecystectomy | ||
| Lin et al[45], 2010 | Journal of Internal Medicine of Taiwan | 80 M | Y-Warfarin | Laparoscopic cholecystectomy |
| Chen et al[46], 2010 | The American Journal of the Medical Sciences | Elderly M | Y-Heparin | Laparoscopic cholecystectomy |
| Miyamoto et al[5], 2009 | J-Stage | 42 F | N | Conservative with IV antibiotics, elective laparoscopic cholecystectomy |
| Oh et al[47], 2009 | Journal of the Korean Society of Magnetic Resonance in Medicine | 40 M | Not mentioned | Laparoscopic cholecystectomy |
| Lai et al[8], 2009 | Journal of Chinese Medical Association | 81 M | Y-Heparin for dialysis | Conservative with IV antibiotics, elective laparoscopic cholecystectomy |
| Morris et al[48], 2008 | Case Reports in Gastroenterology | 91 F | N | Open cholecystectomy |
| Pandya et al[6], 2008 | Abdominal Imaging | 85 F | Y-Warfarin | Conservative with IV antibiotics |
| Kim et al[49], 2007 | World Journal of Gastroenterology | 55 M | N | Cholecystostomy drainage |
| Gremmels et al[50], 2004 | Journal of Ultrasound in Medicine | 66 M | N | Laparotomy + open cholecystectomy |
| Hanaki et al[5], 2000 | J-Stage | 66 M | Not mentioned | Laparotomy + open cholecystectomy |
| Nishiwaki et al[51], 1999 | Journal of Gastroenterology | 58 M | N | Laparotomy + open cholecystectomy |
| Stempel et al[14], 1993 | Journal of Vascular and Interventional Radiology | 78 M | Y-Heparin during AAA repair | Cholecystostomy drainage |
| Brady et al[9], 1985 | Disease of the Colon & Rectum | 79 M | N | Open cholecystectomy |
| Berland et al[52], 1980 | Journal of Computed Assisted Tomography | 56 M | N | Laparotomy + open cholecystectomy |
The elevated prevalence (47%) of patients treated with antiplatelet agents and/or anticoagulants clearly underlines these drugs as risk factors. However, the role of other causes of hemorrhage (accidental or iatrogenic trauma, cholelithiasis, neoplasm, vascular anomalies and coagulopathies) in patients who did not take the aforementioned drugs is not insignificant.
Finally, we can assume that the incidence of this rare pathology is somehow underestimated, given the small number of cases in the literature. In the case described in this report, the patient had been taking cardioaspirin at home.
Moreover, the finding of dissection of the right iliac artery and ulcerated atheromatous plaque, and the thromboembolic risk derived from the patient's bed rest due to chronic lumbar pain suggested the administration of low molecular weight heparin. The self-administration and potential abuse of NSAIDs may have represented an additional risk factor.
Cholelithiasis and the intake of antithrombotic drugs may have played a primary role in the etiology of gallbladder hemorrhage. The damage caused by gallbladder mucosal stones usually heals spontaneously, but this may not occur in patients taking anticoagulants, creating blood oozing that can result in acute bleeding. The patient's medical history, physical examination, laboratory tests and radiological imaging are relevant to the diagnosis, to exclude other pathologies[11,12], in order to promptly plan a strategy, as gallbladder hemorrhage represents a potentially fatal surgical emergency. An initial evaluation with ultrasound can be carried out. Most cases of gallbladder hemorrhage demonstrate ultrasound features not common in acute cholecystitis.
The sonographic findings in hemorrhagic cholecystitis include focal wall thickening, intraluminal membranes and non-shadowing, non-mobile intraluminal echogenic material. There may be some echogenic layering material for which the differential diagnosis includes sludge[13]. The suspicion can be further confirmed by CT examination, which may demonstrate high attenuation within the gallbladder lumen with layering high attenuation fluid-fluid level representing blood or sludge. An early phase contrast-enhanced CT helps to detect active extravasation of contrast and blush within the lumen of the gallbladder[5,6].
The most suitable treatment for gallbladder bleeding is urgent laparoscopic or laparotomic cholecystectomy. In some selected cases, it is possible to plan a non-interventional strategy with antibiotic therapy and supportive medical therapy, postponing subsequent cholecystectomy surgery[5,10].
Rarely, in the case of patients ineligible for surgery, a percutaneous cholecystostomy may be indicated[14,15]. In our case, given the patient’s sudden anemia, despite blood transfusions and supportive medical therapy, due to the persistence of hemodynamic instability we proceeded with urgent surgery.
Gallbladder hemorrhage is a life-threatening complication of cholelithiasis. Early diagnosis of this potentially fatal pathology is essential in order to plan a treatment strategy and eventually proceed with urgent surgical treatment, to ensure timely life-saving decisions and the best results for the patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Kai K, Japan; Yasukawa K, Japan S-Editor: Wu YXJ L-Editor: Webster JR P-Editor: Wu YXJ
| 1. | Kwon JN. Hemorrhagic cholecystitis: report of a case. Korean J Hepatobiliary Pancreat Surg. 2012;16:120-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Yam MKH, Sim SW, Tam KY, Li YL. A 51-year-old female presenting with shock due to hemorrhagic cholecystitis. Radiol Case Rep. 2020;15:2547-2549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Hasegawa T, Sakuma T, Kinoshita H, Nakagawa Y, Kawachiya T, Hara J, Teraoka H. A Case of Hemorrhagic Cholecystitis and Hemobilia Under Anticoagulation Therapy. Am J Case Rep. 2021;22:e927849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Rahesh J, Anand R, Ciubuc J, Athas V, Brooks S, Ronaghan C. Atraumatic spontaneous hemorrhagic cholecystitis. Proc (Bayl Univ Med Cent). 2020;34:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Tarazi M, Tomalieh FT, Sweeney A, Sumner D, Abdulaal Y. Literature review and case series of haemorrhagic cholecystitis. J Surg Case Rep. 2019;2019:rjy360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Pandya R, O'Malley C. Hemorrhagic cholecystitis as a complication of anticoagulant therapy: role of CT in its diagnosis. Abdom Imaging. 2008;33:652-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Parekh J, Corvera CU. Hemorrhagic cholecystitis. Arch Surg. 2010;145:202-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Lai YC, Tarng DC. Hemorrhagic acalculous cholecystitis: an unusual location of uremic bleeding. J Chin Med Assoc. 2009;72:484-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Brady E, Welch JP. Acute hemorrhagic cholecystitis causing hemobilia and colonic necrosis. Dis Colon Rectum. 1985;28:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | García Pérez R, Ruiz de Angulo D, López Poveda MJ, Febrero Sánchez B, Navas Carrillo D, Parrilla Paricio P. Hemorrhagic cholecystitis and hemobilia: two infrequent complications of systemic lupus erythematosus. Rev Esp Enferm Dig. 2011;103:431-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Cavallaro A, Piccolo G, Di Vita M, Zanghì A, Cardì F, Di Mattia P, Barbera G, Borzì L, Panebianco V, Di Carlo I, Cavallaro M, Cappellani A. Managing the incidentally detected gallbladder cancer: algorithms and controversies. Int J Surg. 2014;12 Suppl 2:S108-S119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 12. | Cavallaro A, Piccolo G, Panebianco V, Lo Menzo E, Berretta M, Zanghì A, Di Vita M, Cappellani A. Incidental gallbladder cancer during laparoscopic cholecystectomy: managing an unexpected finding. World J Gastroenterol. 2012;18:4019-4027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 13. | Chinn DH, Miller EI, Piper N. Hemorrhagic cholecystitis. Sonographic appearance and clinical presentation. J Ultrasound Med. 1987;6:313-317. [PubMed] [DOI] [Full Text] |
| 14. | Stempel LR, Vogelzang RL. Hemorrhagic cholecystitis with hemobilia: treatment with percutaneous cholecystostomy and transcatheter urokinase. J Vasc Interv Radiol. 1993;4:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Imamura H, Minami S, Isagawa Y, Morita M, Hirabaru M, Kawahara D, Tokai H, Noda K, Inoue K, Haraguchi M, Eguchi S. The impact of antithrombotic therapy in patients undergoing emergency laparoscopic cholecystectomy for acute cholecystitis - A single center experience. Asian J Endosc Surg. 2020;13:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Nguyen D, Goodwin JS, Bhowmik N, Boiteau G, Potts J. Acute Hemorrhagic Cholecystitis with Large Hemoperitoneum: Treatment with Microcoil Embolization and Subsequent Cholecystectomy. J Radiol Case Rep. 2021;15:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Chen X, Yu L. A haemorrhagic cholecystitis presenting as obstructive jaundice. Hepatobiliary Surg Nutr. 2021;10:299-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Leaning M. Surgical case report-acalculous hemorrhagic cholecystitis. J Surg Case Rep. 2021;2021:rjab075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Azam MU, Ibrahim MA, Perry I, Ellison SB, Barrett A, Vega KJ. It's the Bloody Gallbladder! J Natl Med Assoc. 2021;113:252-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Gomes AF, Fernandes S, Martins J, Coutinho J. Carcinoma of the gallbladder presenting as haemorrhagic cholecystitis. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Kishimoto T, Hashimoto Y, Imamura H, Shigetsu K, Murotani M, Yoneda N, Kidogami S, Mokutani Y, Hirose H, Yoshioka S, Endo S, Tamura S, Sasaki Y. [A Case of Rapidly Progressive Gallbladder Cancer Presented with Gallbladder Hemorrhage]. Gan To Kagaku Ryoho. 2020;47:2361-2363. [PubMed] |
| 22. | Reens D, Podgorski B. Hemorrhagic Cholecystitis: A Case of Expedited Diagnosis by Point-of-Care Ultrasound in the Emergency Department. J Emerg Med. 2019;57:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Itagaki H, Katuhiko S. Gallbladder hemorrhage during orally administered edoxaban therapy: a case report. J Med Case Rep. 2019;13:383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Honda F, Tsuboi H, Toko H, Terasaki T, Terasaki M, Shimizu M, Ohyama A, Yagishita M, Takahashi H, Yokosawa M, Asashima H, Hagiwara S, Kondo Y, Matsumoto I, Sumida T. Contrast Enhanced Computed Tomography Revealed Gallbladder Hemorrhage Due to Active Vasculitis in a Patient With Microscopic Polyangiitis. J Clin Rheumatol. 2019;25:e84-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | San Juan López C, Lázaro Sáez M, Hernández Martínez Á, López González J, Vega Sáenz JL. Bleeding from gallbladder varices in a patient with an unknown liver cirrhosis. An exceptional entity. Rev Esp Enferm Dig. 2019;111:723-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Ng ZQ, Pradhan S, Cheah K, Wijesuriya R. Haemorrhagic cholecystitis: a rare entity not to be forgotten. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Liefman D, Wullschleger M. Hemorrhagic cholecystitis: a rare cause of presentation with upper gastrointestinal bleeding. Int Ann Med. 2018;2:5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | López V, Alconchel F. Hemorrhagic Cholecystitis. Radiology. 2018;289:316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Berndtson AE, Hamel MG, Costantini TW, Coimbra R. Acalculous Perforated Hemorrhagic Emphysematous Cholecystitis Caused by Clostridium perfringens in a Patient with Myeloma Taking Daratumumab. Surg Infect Case Rep. 2017;2:1-4. [DOI] [Full Text] |
| 30. | Choi KK, Lee MA, Ma DS, Lee GJ, Yu BC, Lee JN. A Hemorrhagic Cholecystitis in a Penetrating Hepatic Injury Trauma Image Proced. 2017; 2(1): 15-16. Published online: May 31, 2017. [DOI] [Full Text] |
| 31. | Kinnear N, Hennessey DB, Thomas R. Haemorrhagic cholecystitis in a newly anticoagulated patient. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Shishida M, Ikeda M, Karakuchi N, Ono K, Tsukiyama N, Shimomura M, Oishi K, Miyamoto K, Toyota K, Sadamoto S, Takahashi T. Hemorrhagic Cholecystitis in a Patient on Maintenance Dialysis. Case Rep Gastroenterol. 2017;11:488-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Oshiro Y, Tsukamoto S, Owada Y, Takahashi K, Oda T, Sakamoto N, Ohkohchi N. Hemorrhagic Cholecystitis During Anticoagulant Therapy in a Patient With Systemic Lupus Erythematosus and Antiphospholipid Syndrome Undergoing Elective Laparoscopic Cholecystectomy. Int Surg. 2017;105:1-3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Yoshida S, Yokoyama K, Nishida T, Ikuta H. A Case of Gallbladder Hemorrhage Occurred during Anticoagulation Therapy. J Japan Surg Associa. 2017;78:359-364. [DOI] [Full Text] |
| 35. | Tsai JL, Tsai SF. Gallbladder bleeding-related severe gastrointestinal bleeding and shock in a case with end-stage renal disease: A case report. Medicine (Baltimore). 2016;95:e3870. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Calvo Espino P, Chaparro Cabezas MD, Jiménez Cubedo E, Lucena de la Poza JL, Sánchez Turrión V. Perforated hemorrhagic cholecystitis. Cir Esp. 2016;94:e35-e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Cho SH, Lee HY, Kim HS. Anticoagulant Therapy-Induced Gallbladder Hemorrhage after Cardiac Valve Replacement. Korean J Thorac Cardiovasc Surg. 2015;48:432-434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Aljiffry MM, Almulhim AN, Jamal MH, Hassanain MM. Acute cholecystitis presenting with massive intra-abdominal haemorrhage. J Surg Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Onozawa H, Saito M, Yoshida S, Sakuma T, Matsuzaki M, Katagata N, Watanabe F, Yamaguchi Y, Takenoshita S, Nomizu T. Multiple metastatic malignant melanoma presenting intraluminal gallbladder bleeding. Int Surg. 2014;99:600-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Asai K, Watanabe M, Kusachi S, Matsukiyo H, Saito T, Kodama H, Dotai K, Hagiwara O, Enomoto T, Nakamura Y, Okamoto Y, Saida Y, Nagao J. Changes in the therapeutic strategy for acute cholecystitis after the Tokyo guidelines were published. J Hepatobiliary Pancreat Sci. 2013;20:348-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Seok DK, Ki SS, Wang JH, Moon ES, Lee TU. Hemorrhagic cholecystitis presenting as obstructive jaundice. Korean J Intern Med. 2013;28:384-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Taniguchi M, Kanai S, Kitamura M, Nakamura I, Nakamura T, Shimomatsuya T. A case of gallbladder hemorrhage with intraperitoneal bleeding. J Japan Surg Associa. 2013;74:503-507. [DOI] [Full Text] |
| 43. | Choi YS. Gallbladder hemorrhage mimicking acute cholecystitis in a patient under antiplatelet therapy. Z Gastroenterol. 2012;50:285-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Jung YM, Son BK, Ahn SB, Kim DH, Kim EK. Intramural gallbladder hematoma mimicking gallbladder neoplasm in a 55-year-old male patient. J Korean Surg Soc. 2011;81:216-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Lin HP, Lin YC. Isolated intraluminal gallbladder hemorrhage after anticoagulation therapy: Report of a case. Taiwa J Obstet Gynecol. 2010;21:62-65. [DOI] [Full Text] |
| 46. | Chen YY, Yi CH, Chen CL, Huang SC, Hsu YH. Hemorrhagic cholecystitis after anticoagulation therapy. Am J Med Sci. 2010;340:338-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 47. | Oh SY, Park MH, Jee KN, Jeon GS, Kim HJ. Acalculous hemorrhagic cholecystitis with chronic intraluminal hematoma: MRI findings. Magn Reson Imaging. 2009;13:195-198. [DOI] [Full Text] |
| 48. | Morris DS, Porterfield JR, Sawyer MD. Hemorrhagic cholecystitis in an elderly patient taking aspirin and cilostazol. Case Rep Gastroenterol. 2008;2:203-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 49. | Kim YC, Park MS, Chung YE, Lim JS, Kim MJ, Kim KW. Gallstone spillage caused by spontaneously perforated hemorrhagic cholecystitis. World J Gastroenterol. 2007;13:5525-5526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Gremmels JM, Kruskal JB, Parangi S, Kane RA. Hemorrhagic cholecystitis simulating gallbladder carcinoma. J Ultrasound Med. 2004;23:993-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Nishiwaki M, Ashida H, Nishimura T, Kimura M, Yagyu R, Nishioka A, Utsunomiya J, Yamamura T. Posttraumatic intra-gallbladder hemorrhage in a patient with liver cirrhosis. J Gastroenterol. 1999;34:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Berland LL, Doust BD, Foley WD. Acute hemorrhage into the gallbladder diagnosed by computed tomography and ultrasonography. J Comput Assist Tomogr. 1980;4:260-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |