Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9510
Peer-review started: May 9, 2022
First decision: June 16, 2022
Revised: June 25, 2022
Accepted: August 16, 2022
Article in press: August 16, 2022
Published online: September 16, 2022
Processing time: 116 Days and 0 Hours
Diffuse retinal pigment epitheliopathy (DRPE) associated with bullous retinal detachment is a severe variant of DRPE that is frequently misdiagnosed and often improperly treated.
A 36-year-old female patient complained of "painless vision decline in the left eye with obscuration for 10 d". Slit-lamp microscopic fundus examination revealed white-yellow subretinal exudates in the posterior pole in both eyes, retinal detachment with shifting subretinal fluid in the left eye, and no retinal hiatus. Fundus fluorescein angiography revealed multiple subretinal leakage foci and localized hypofluorescent lesions with patched hyperfluorescence. There was fluorescence leakage in the retinal vessels in the retinal detachment area and occluded blood vessels in the lower and peripheral areas. Indocyanine green angiography revealed multifocal lamellar hyperfluorescence in the middle stage and low fluorescence in the retinal detachment area in the late stage. Retinal anatomical reduction significantly improved with intravitreal conbercept injections.
Intravitreal injection of conbercept can anatomically reattach the retina in patients with bullous retinal detachment.
Core Tip: The study patient exhibited a considerable improvement in retinal anatomical reduction after intravitreal injections of conbercept. Nevertheless, due to the the macular area destruction, we observed unsatisfactory improvement in best-corrected visual acuity. Based on the study findings, intravitreal injection of a vascular endothelial growth factor inhibitor may be a considered potent therapeutic option for cases of bullous retinal detachment of diffuse retinal pigment epitheliopathy. This treatment is uncomplicated and harmless and precludes adopting complex surgical techniques associated with high risk of complications.
- Citation: Xiang XL, Cao YH, Jiang TW, Huang ZR. Intravitreous injection of conbercept for bullous retinal detachment: A case report. World J Clin Cases 2022; 10(26): 9510-9517
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9510.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9510
Bullous retinal detachment is an extremely rare manifestation of diffuse retinal pigment epitheliopathy (DRPE) or chronic central serous chorioretinopathy (CSCR). It is difficult to treat and can eventually result in loss of vision due to irreversible retinal damage[1-2]. The clinical features of this disease include multiple serous vesicular retinal detachments at the posterior pole and the periphery of the fundus. Multiple retinal detachments often fuse into one large retinal detachment and are located below because of gravity and fluid accumulation. This disease is very easily misdiagnosed and is, thus, often treated improperly, which leads to rapid deterioration of the patient's condition, resulting in permanent visual damage or even blindness[1-3].
Herein, we report a case of bullous retinal detachment with retinal reattachment after vitreous injection of conbercept.
A 36-year-old female patient complained of "painless vision decline in the left eye with dark shadow covering for 10 d".
Ten days previously, she had a feeling of decreased vision with dark shadow covering in her left eye.
The patient neither had a history of ocular trauma or surgery nor a family history of ocular diseases. She denied any history of systemic disorders or sojourns in the epidemic-stricken area and was not receiving any medication at the time.
The patient had a 14-year-old daughter with type 1 diabetes mellitus combined with diabetic cataracts.
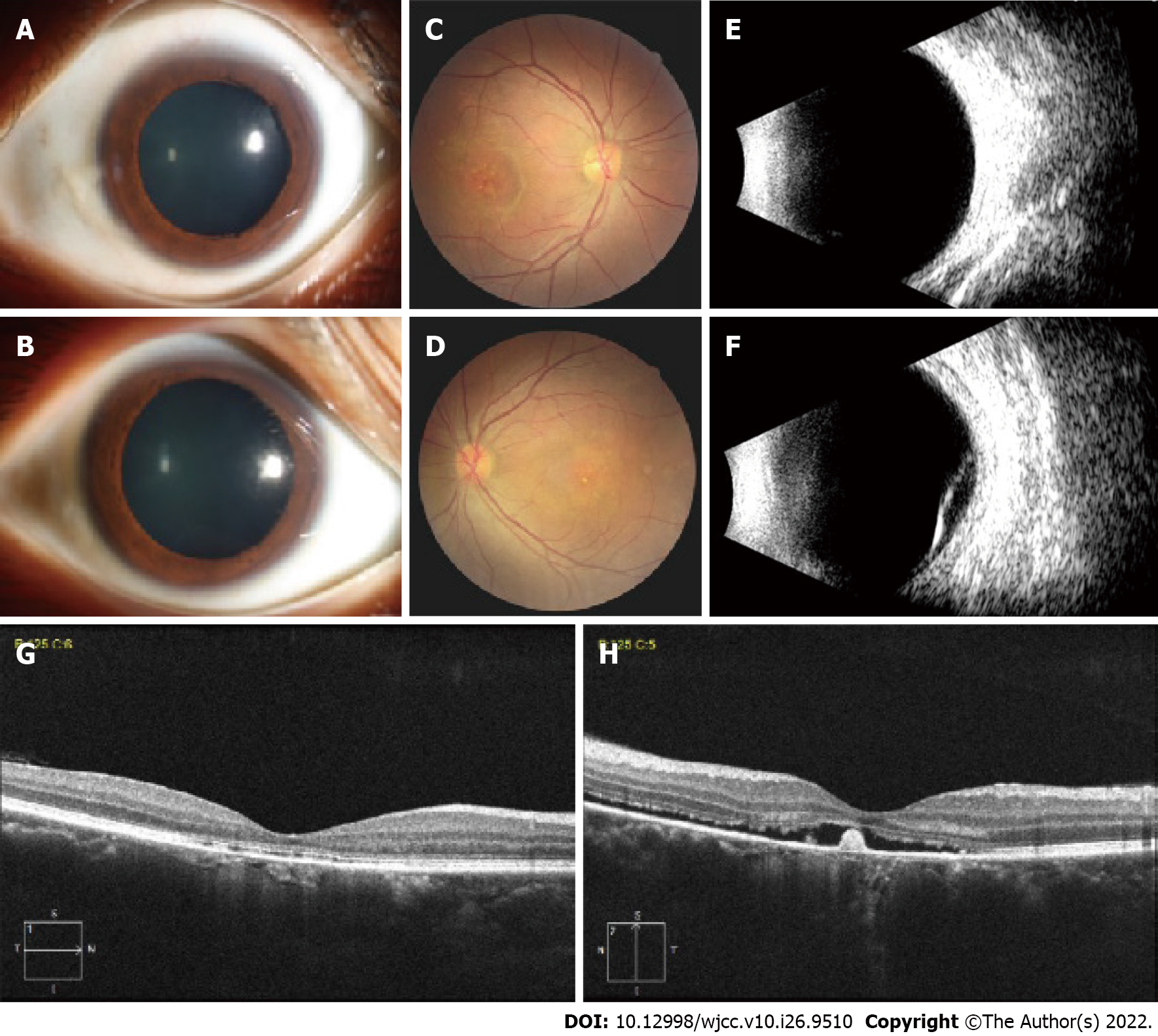
On her first visit to our department, her best-corrected visual acuity (BCVA) was 20/30 in the right eye and 20/100 in the left eye. Slit-lamp microscopic examination revealed no inflammatory signs in the anterior chamber (Figure 1A and B) or vitreous in either eye. Dilated fundus examination revealed white-yellow subretinal exudates in the posterior pole in both eyes, corrugated inferior bullous retinal detachment with shifting of subretinal fluid, and no retinal hiatus (Figure 1C and D).
Laboratory tests, such as routine blood tests, infectious diseases, blood biochemistry, and tumor indicators, were normal. The results of chest computed tomography and electrocardiogram were also normal.
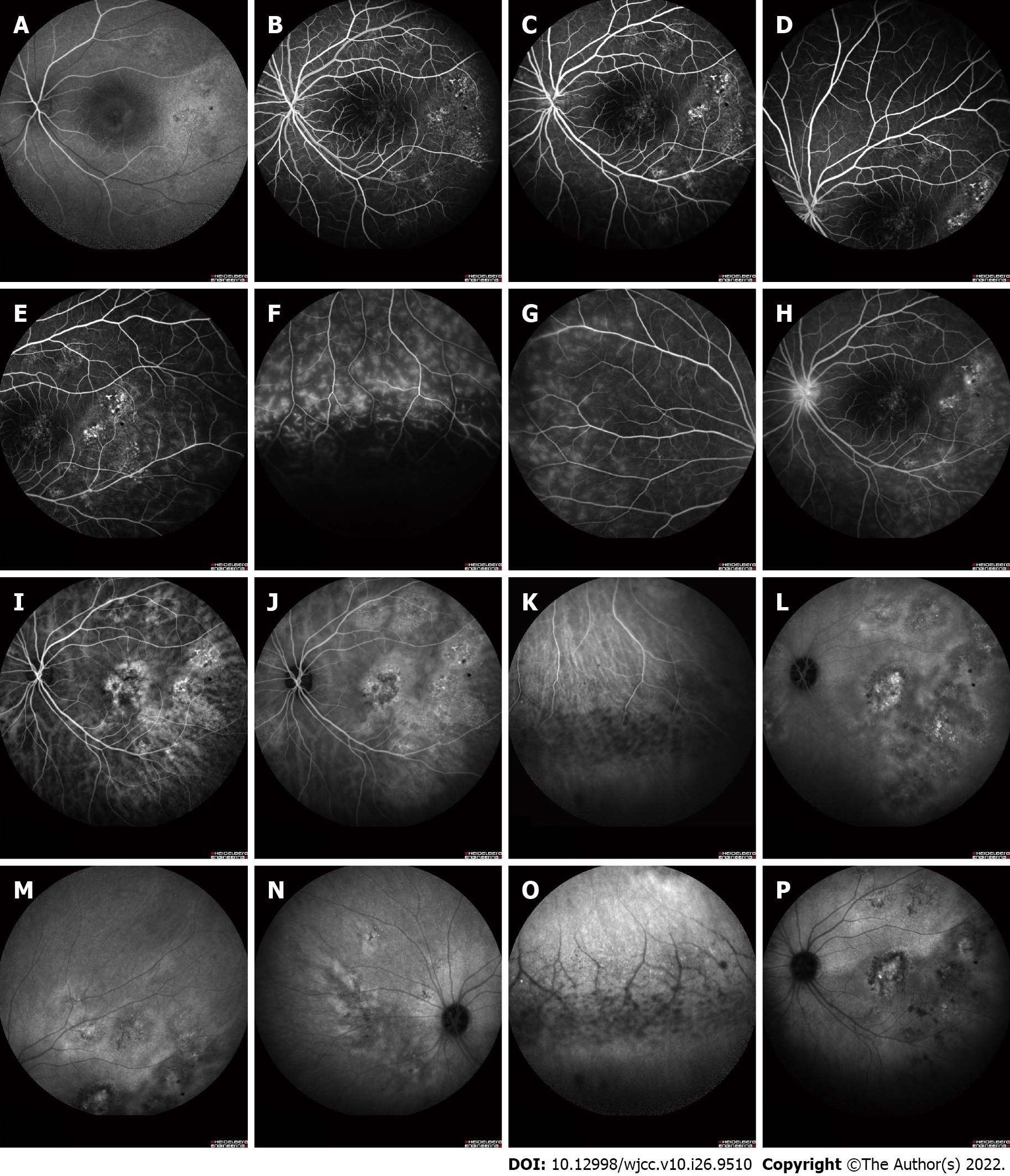
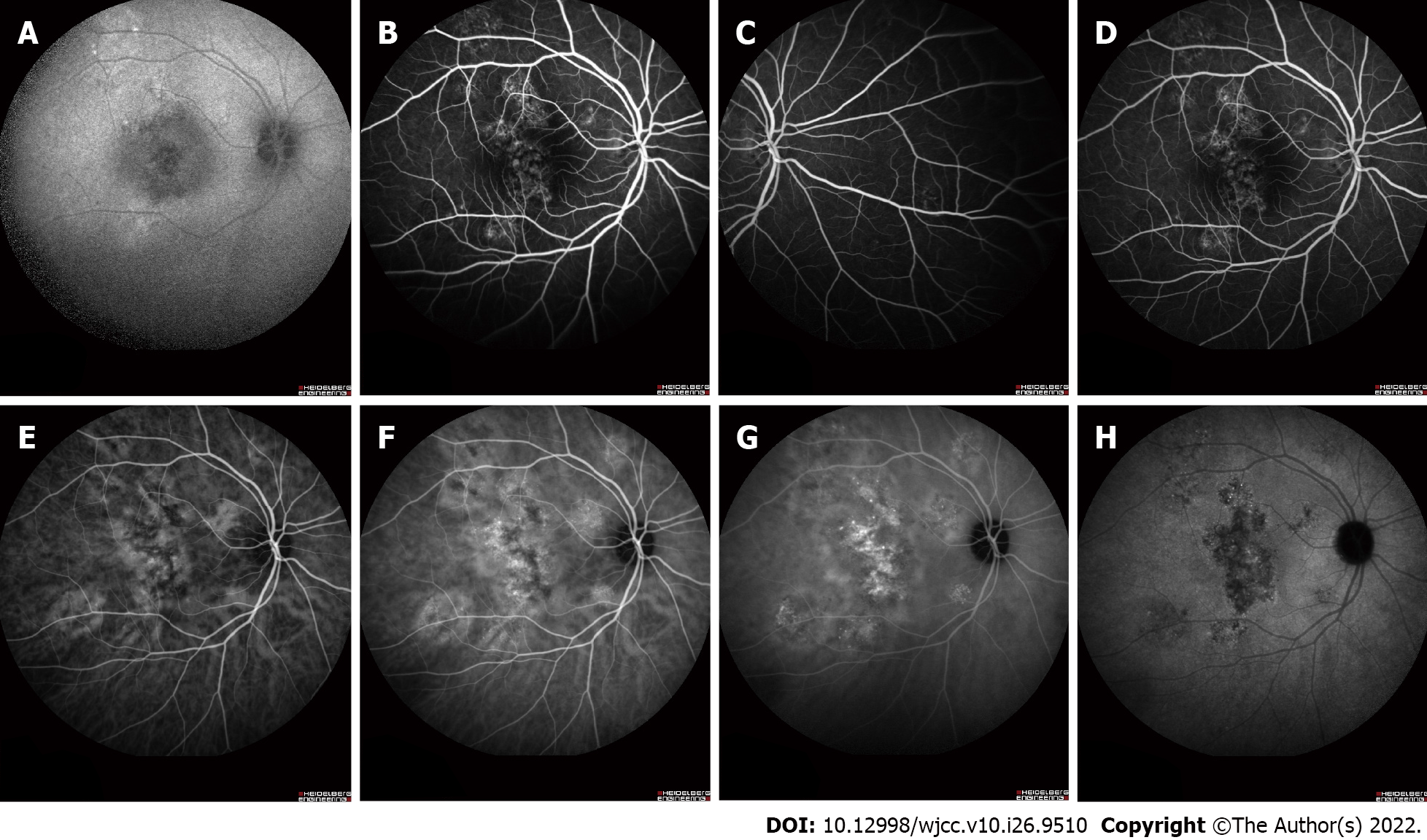
Ophthalmic B-scan ultrasonography confirmed a bullous retinal detachment in the left eye (Figure 1F). B-scan ultrasonography of the right eye revealed normal findings (Figure 1E). Optical coherence tomography (OCT) showed a discontinuous band of retinal pigment epithelium in the right eye (Figure 1G) and neurosensory detachment at the fovea with some hyperreflective material suggestive of fibrin in the left eye (Figure 1H). Fundus fluorescein angiography (FFA) revealed multiple patchy leakage foci in the retina, with localized low fluorescence damage and patchy high fluorescence. Retinal vascular fluorescence leakage was observed in the retinal detachment area. Some retinal vessels in the non-detachment area showed slight leakage, and the optic disc exhibited slight leakage in the late stage (Figure 2A-H). Indocyanine green angiography (ICGA) showed multifocal flakes with high fluorescence in the middle stage and low fluorescence in the retinal detachment area in the late stage (Figure 2I-P). FFA and ICGA of the right eye were also abnormal (Figure 3).
Based on the abovementioned clinical, laboratory, and imaging findings, the patient was diagnosed with DRPE complicated by bullous exudative retinal detachment.
Treatment consisted of intravitreal injections of conbercept (0.05 mL/0.5 mg) under sterile conditions. Topical corticosteroids were not advised, and follow-up commenced without any other specific interventions. According to the BCVA and OCT results, reinjection was administered as needed. The patient received a second injection of the same dose 1 mo after the first injection. Eventually, the patient received two injections.
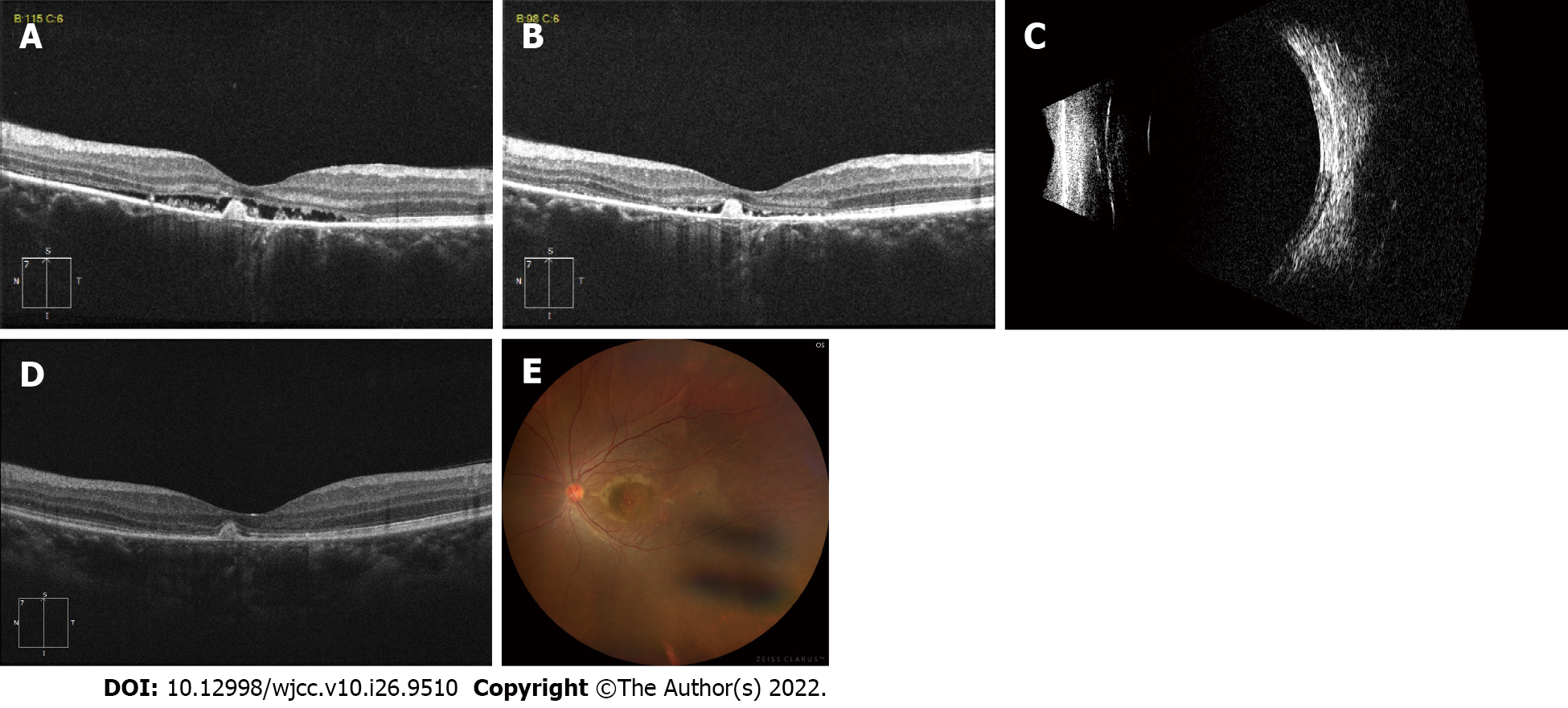
One month after the first injection, the BCVA in the left eye was 20/100; however, fundus examination showed reduced neurosensory detachment, and OCT indicated that the subretinal fluid volume was reduced (Figure 4A). One month after the second injection, her BCVA increased to 20/50. The subretinal fluid was almost completely absorbed; however, a small amount of fluid was still visible in the central fovea of the macula, under which a highly reflective signal could be observed (Figure 4B and C). Six months after the second injection, her BCVA was 20/50, and the subretinal fluid was completely absorbed (Figure 4D and E).
We describe a case of intravitreal injection of conbercept that cured bullous retinal detachment. After two intravitreal injections, the patient exhibited retinal reattachment. DRPE is the idiopathic form of central serous chorioretinopathy (CSC), which has a poorer prognosis than typical CSC[1]. As a unique type of exudative retinal detachment, bullous retinal detachment is an atypical manifestation of CSC[4], also known as bullous central serous chorioretinopathy (bCSCR). Tsukahara and Uyama[5] further detailed the pathogenesis of this disease as follows: increased choroidal vascular permeability alters RPE, thereby damaging RPE outer blood-retina barrier. Subsequently, fibrinogen and protein leak out, and subretinal exudation occurs. DRPE associated with bullous retinal detachment is frequently misdiagnosed[2]. Differential diagnoses include rhegmatogenous retinal detachment or exudative detachment, such as Vogt-Koyanagi-Harada disease, posterior scleritis, metastatic tumors, uveal effusion syndrome, and other disorders. This condition is aggravated by the use of steroids. Incorrect treatment can cause the condition to worsen rapidly, leading to permanent visual impairment and even blindness[2]. The correct diagnosis of DRPE may prevent complications from the misuse of corticosteroids, as well as unnecessary surgery and vision loss.
The current patient had a normal axial length and no evidence of uveitis, ciliochoroidal detachment, or ocular signs was observed. Intraocular tumors and choroidal detachment were excluded using B-type ultrasonography. Prolonged retinal detachment may manifest as vascular leakage in the area of detachment on FFA, and because the subretinal fluid changes with position, the upper retina may also show slight vascular leakage, with slightly higher fluorescence around the optic disc. ICGA indicated primary choroidal hyperpermeability with secondary retinal pigment epithelium dysfunction in both eyes. Although this patient complained of reduced visual acuity in one eye, changes in the retinal pigment epithelium (RPE) were visible in both eyes on FFA and ICGA. Scholars in Japan have reported the average age of onset of DRPE to be 43.1 years[6]. Similarly, Chinese scholars reported that the average age was 40.5 ± 6.7 years, and the male-to-female ratio was 5:1[3]. The present study patient was 36 years old, which was within the age range reported in the literature.
Choroidal vascular dysfunction is an important feature of DRPE pathophysiology[7]. DRPE is characterized by the dilation of vessels in the outer layer of the choroid, atrophy of the inner layer of the choroid, and thick choroidal features with high choroidal permeability[7,8]. Laser photocoagulation and/or photodynamic therapy[3,9,10] are potential treatment options for patients with threatened visual acuity[11]. Vitrectomy and internal drainage of the subretinal fluid have also been reported as treatment options for retinal detachment in DRPE[12]. Intravitreal injection of anti-vascular endothelial growth factor (VEGF) is also considered[13]. Anti-VEGF drugs are used for treating such diseases because of their anti-permeability characteristics, which reduce the high permeability of choroidal blood vessels[14,15]. To date, there has been only one case report of treatment of bCSCR with intravitreal injection of anti-VEGF without clinical improvement[16]. The patient was treated unsuccessfully with intravitreal bevacizumab (1.25 mg) and ranibizumab (0.5 mg) followed by successful treatment with reduced fluence photodynamic therapy[16]. Ranibizumab and bevacizumab are derived from a murine monoclonal antibody[15].
We selected the anti-VEGF agent, conbercept, which is a recombinant fusion protein with different chemical structure and pharmacological properties from other anti-VEGF drugs. Conbercept is fused by VEGF receptors 1 and 2 to the Fc portion of human immunoglobulin G1 that blocks VEGF-B, placental growth factor, and all VEGF-A isoforms[15]. We proposed the potential efficacy of conbercept in bullous retinal detachment, considering its anti-permeability properties in decreasing choroidal vascular hyperpermeability. The current patient demonstrated a significant improvement in retinal anatomical reduction following intravitreal injections of conbercept. However, because of the destruction of the macular area, there was limited improvement in BCVA.
Stress events may be predisposing factors for bullous retinal detachment[16,17]. The stress factor was observed in this case. Ultimately, we performed binocular cataract phacoemulsification and intraocular lens implantation for the patient's daughter free of charge and recommended that they visit the ophthalmology clinic on a regular basis. At the time of the final follow-up, the ocular conditions of both the patient and her daughter were stable.
In conclusion, we describe a case of intravitreal injection of conbercept that cured the bullous retinal detachment of DRPE. This case suggests that intravitreal injection of a VEGF inhibitor may be a considered therapeutic option for patients with bullous retinal detachment of DRPE. This treatment is safe and simple, avoiding the need for complex surgical techniques with high risk of complications. However, our conclusion is based on a single case report with no long-term outcomes. Therefore, a larger case series and longer follow-up periods are needed to further explore such treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Beji H, Tunisia; Nuño JSZ, Mexico S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Canakis C, Livir-Rallatos C, Panayiotis Z, Livir-Rallatos G, Persidis E, Conway MD, Peyman GA. Ocular photodynamic therapy for serous macular detachment in the diffuse retinal pigment epitheliopathy variant of idiopathic central serous chorioretinopathy. Am J Ophthalmol. 2003;136:750-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Kunavisarut P, Pathanapitoon K, van Schooneveld M, Rothova A. Chronic central serous chorioretinopathy associated with serous retinal detachment in a series of Asian patients. Ocul Immunol Inflamm. 2009;17:269-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Gao T, Qu J, Xiao J, Hu J, Zhao M. Photodynamic therapy for bullous retinal detachment: a single-center experience of case series with a 6-month follow-up study. Graefes Arch Clin Exp Ophthalmol. 2018;256:1429-1439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Gass JD. Bullous retinal detachment. An unusual manifestation of idiopathic central serous choroidopathy. Am J Ophthalmol. 1973;75:810-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 86] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Tsukahara I, Uyama M. Central serous choroidopathy with bullous retinal detachment. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1978;206:169-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Otsuka S, Ohba N, Nakao K. A long-term follow-up study of severe variant of central serous chorioretinopathy. Retina. 2002;22:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Kaye R, Chandra S, Sheth J, Boon CJF, Sivaprasad S, Lotery A. Central serous chorioretinopathy: An update on risk factors, pathophysiology and imaging modalities. Prog Retin Eye Res. 2020;79:100865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 153] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 8. | Sartini F, Menchini M, Posarelli C, Casini G, Figus M. Bullous Central Serous Chorioretinopathy: A Rare and Atypical Form of Central Serous Chorioretinopathy. A Systematic Review. Pharmaceuticals (Basel). 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Kuroyanagi K, Sakai T, Kasai K, Tsuneoka H. Spectral domain optical coherence tomography and angiographic findings in multifocal posterior pigment epitheliopathy treated with low-fluence photodynamic therapy. Clin Exp Optom. 2013;96:126-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Ng WW, Wu ZH, Lai TY. Half-dose verteporfin photodynamic therapy for bullous variant of central serous chorioretinopathy: a case report. J Med Case Rep. 2011;5:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Yannuzzi LA, Slakter JS, Gross NE, Spaide RF, Costa D, Huang SJ, Klancnik JM Jr, Aizman A. Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina. 2003;23:288-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 327] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 12. | Kang JE, Kim HJ, Boo HD, Kim HK, Lee JH. Surgical management of bilateral exudative retinal detachment associated with central serous chorioretinopathy. Korean J Ophthalmol. 2006;20:131-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Pitcher JD 3rd, Witkin AJ, DeCroos FC, Ho AC. A prospective pilot study of intravitreal aflibercept for the treatment of chronic central serous chorioretinopathy: the CONTAIN study. Br J Ophthalmol. 2015;99:848-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Torres-Soriano ME, García-Aguirre G, Kon-Jara V, Ustariz-Gonzáles O, Abraham-Marín M, Ober MD, Quiroz-Mercado H. A pilot study of intravitreal bevacizumab for the treatment of central serous chorioretinopathy (case reports). Graefes Arch Clin Exp Ophthalmol. 2008;246:1235-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Mao J, Zhang C, Liu C, Shen L, Lao J, Shao Y, Chen Y, Tao J. The Efficacy of Intravitreal Conbercept for Chronic Central Serous Chorioretinopathy. J Ophthalmol. 2019;2019:7409426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Wykoff CC, Lujan BJ, Rosenfeld PJ. Photodynamic therapy of bullous central serous chorioretinopathy with subretinal exudate and a tear of the retinal pigment epithelium. Retin Cases Brief Rep. 2009;3:218-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Spaide RF, Goldbaum M, Wong DW, Tang KC, Iida T. Serous detachment of the retina. Retina. 2003;23:820-46; quiz 895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |