Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9361
Peer-review started: April 6, 2022
First decision: May 29, 2022
Revised: June 11, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 149 Days and 3.4 Hours
Multicystic biliary hamartoma (MCBH) is a rare hamartomatous nodule of the liver, which has recently been described as a new category of hepatic nodular cystic lesion. Most of them are benign. The imaging findings are similar to those of many other hepatic cystic lesions, but MCBH also has some notable features, such as large cysts, smooth cyst walls, and lack of communication with the hepatic duct. Due to the non-specific radiology, preoperative diagnosis is difficult, and is usually diagnosed by postoperative pathology. Complete resection is the best treatment option, and the postoperative prognosis is good.
When the patients have MCBH, the symptoms may not very typical, and they require a combination of imaging and pathology for diagnosis. Under normal circumstances, the prognosis of MCBH is good. However, in patients with MCBH, more cases need to be observed for verification.
When the patients have MCBH, the symptoms may not very typical, and they require a combination of imaging and pathology for diagnosis. Under normal circumstances, the prognosis of MCBH is good. However, in patients with MCBH, more cases need to be observed for verification.
Core Tip: Intrahepatic multicystic biliary hamartoma (MCBH) is a relatively rare disease with relatively few cases reported in the English literature. We review previously reported articles on MCBH on our essay, summarizing some of their characteristics and treatment. More importantly, we studied and interpreted a case that we found during our clinical work. In this essay, we describe his clinical manifestations, imaging performance, laboratory test results, pathological manifestations and surgery. We also discuss and summarize the characteristics of MCBH. We hope to better diagnose MCBH through imaging examination and pathological examination through our essay.
- Citation: Wang CY, Shi FY, Huang WF, Tang Y, Li T, He GL. Intrahepatic multicystic biliary hamartoma: A case report. World J Clin Cases 2022; 10(26): 9361-9367
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9361.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9361
Bile duct hamartoma was described for the first time by von Meyenburg in a pathology report. Subsequently, it was depicted on contrast-enhanced magnetic resonance imaging. In 1975, McLoughlin and Phillips first described its angiographic characteristics. Later, others described the computed tomography (CT) and ultrasound characteristics of multicystic biliary hamartoma (MCBH)[1]. As for the etiology of MCBH, biliary plate malformations may be one of the pathological causes, which can be ascribed to abnormal embryogenesis of the biliary ductal system. As a type of fibrous polycystic liver diseases, MCBH needs to be differentiated from the others include congenital liver fibrosis, autosomal dominant polycystic liver disease, Caroli's disease, and choledochal cyst. However, only a few cases have been published in the world literature[2]. The previous literatures have never reported patient aged lower than 30 years old with MCBH, nevertheless, the age of this patient is only 14 years old, and apart from this, the large size of the cyst is unprecedented. Here we describe this unique case report and the literature review of MCBH.
Physical examination showed abnormal lumps in the intra-abdominally. Further consultation and physical examination revealed no evidence of the following: Headache and dizziness, dyspnea and shortness of breath, diarrhea and melena, and frequent and/or urgent micturition.
No history of present illness.
No significant past illness.
No family history or relevant genetic information.
Physical examination showed abnormal lumps in the intra-abdominally.
Total bilirubin (TBil), 9.7 μmol/L; direct bilirubin, 4.5 μmol/L; albumin, 39.9 g/L; alanine aminotransferase, 8 IU/L; aspartate aminotransferase, 12 IU/L; alpha-fetoprotein, 1.2 μg/L; HBsAb, 24.100 IU/L; HBeAb, 1.590 COI; and HBcAb, 2.360 COI.
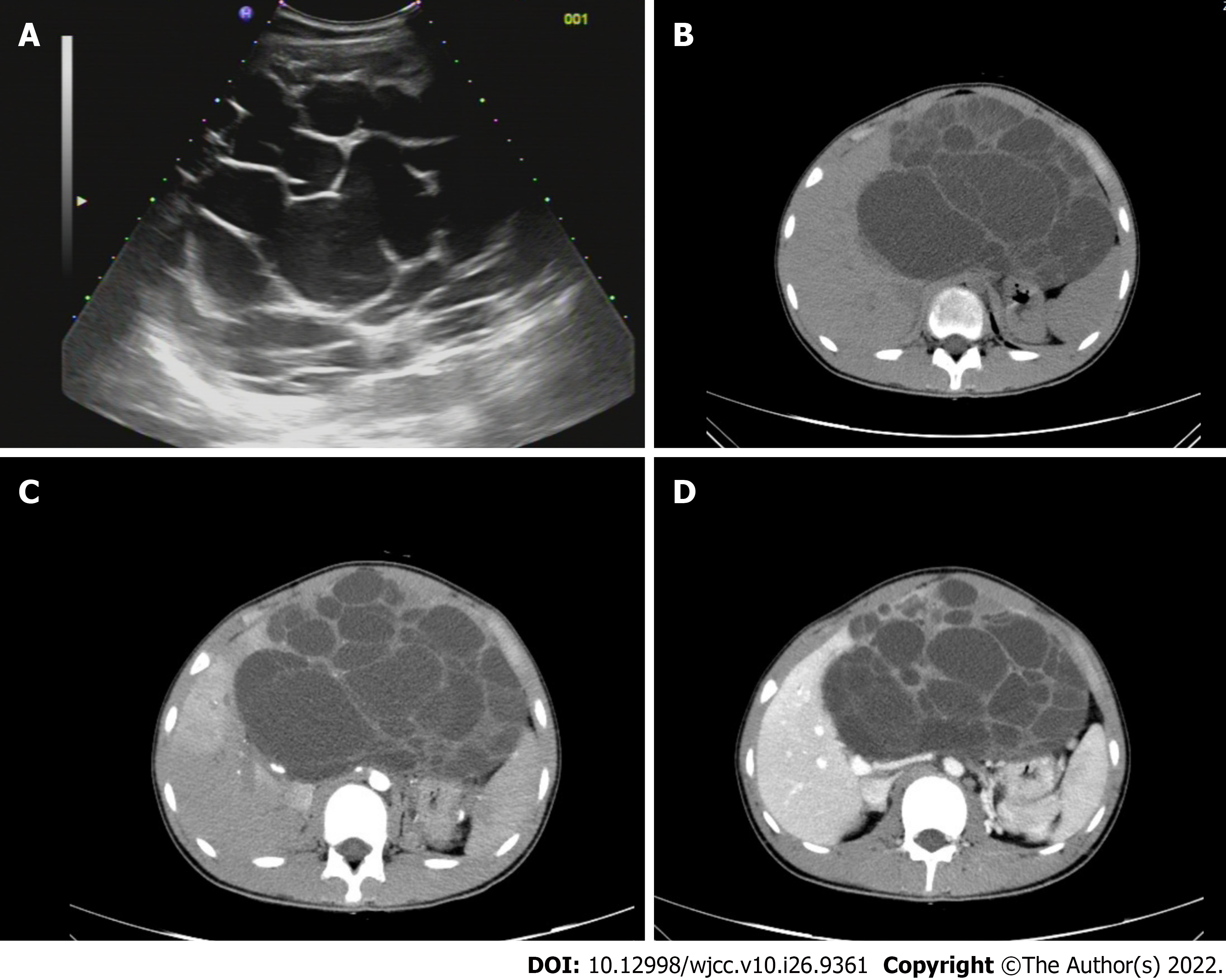
An abdominal CT (Figure 1) showed a large, cystic, space-occupying lesion, with blurred outline with respect to adjacent liver structures. Further CT imaging revealed a multicystic lesion located in the upper abdomen, suggestive of a cystadenoma or lymphangioma. Enhanced CT indicated asymmetrical intensification in the right lobe during the arterial phase, and demonstrated homogeneous enhancement in the right lobe during the portal vein phase and delayed phase, which was considered to be attributed to abnormal perfusion.
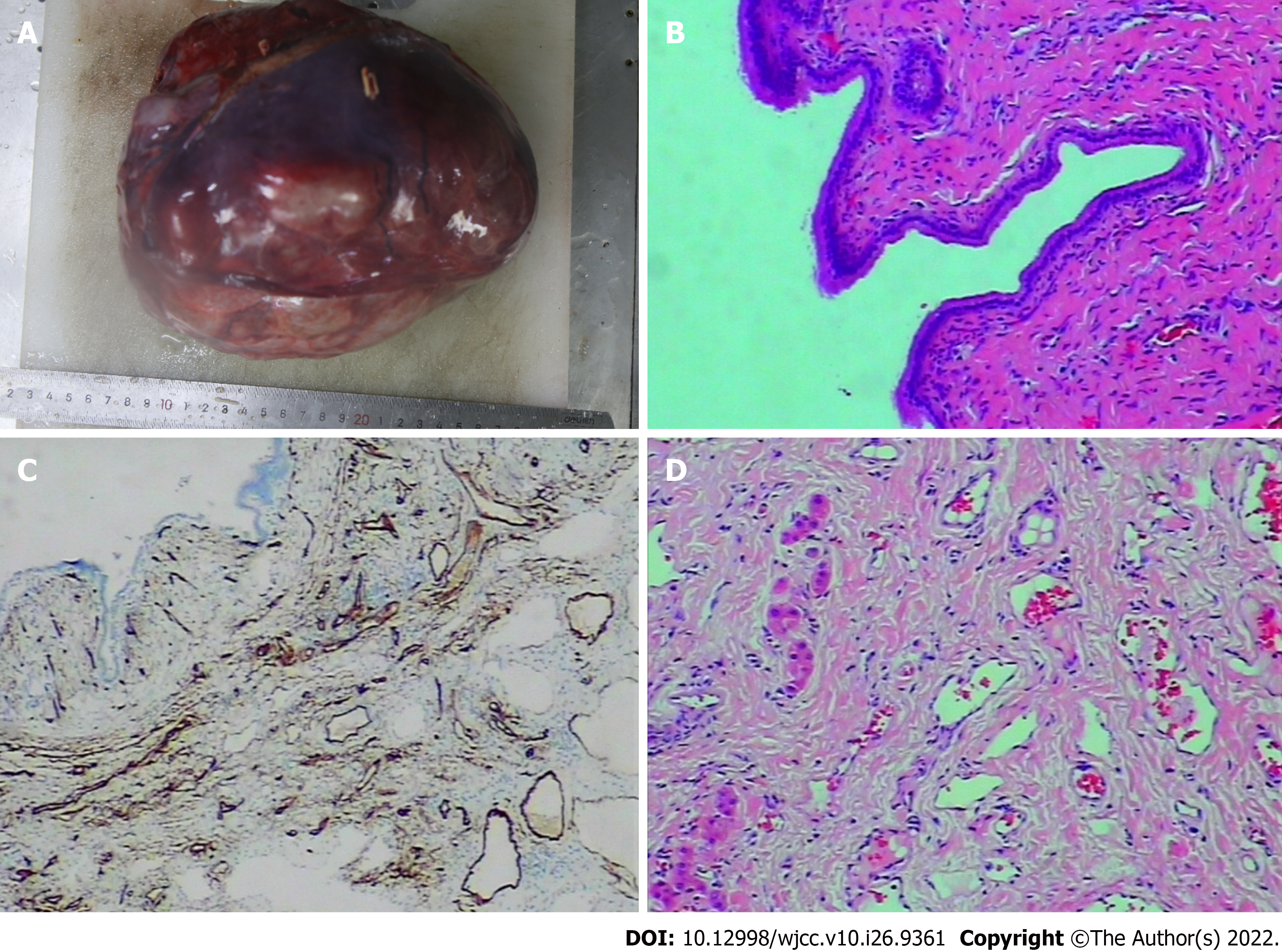
Intrahepatic multicystic biliary hamartoma (Figures 2 and 3).
Laparoscopic partial resection.
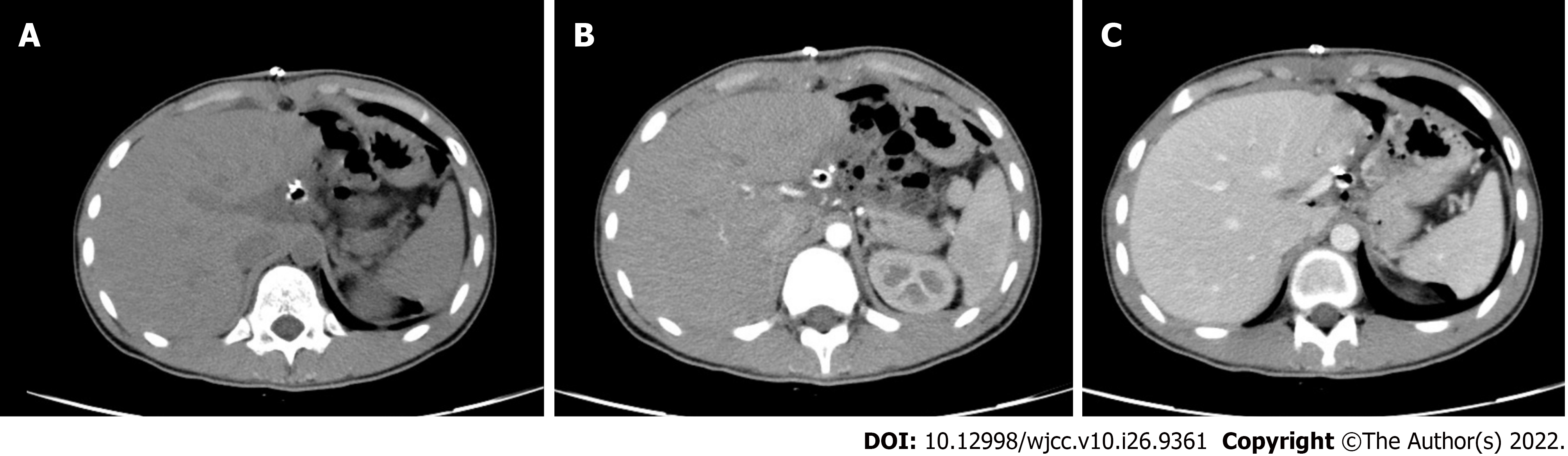
The patient received postoperative antibiotic, hepatoprotective, and analgesic therapy. The postoperative recovery was good, and the CT reexamination showed good prognosis.
MCBH is a rare benign fibrocystic liver disease, which may be related to the malformations of the bile duct plate[3]. Currently, there are very limited published reports of MCBH worldwide. Since the first description of MCBHs in 2005, there have only been 16 published cases worldwide (Table 1)[2,4-14]. MCBHs can occur at any age, although it is more common in patients aged 30–70 years, and is two times as likely to affect men than women, with a male-to-female ratio of 10:6. Of note, compared with the former cases, the age is younger and the size is larger of the patients with MCBH in this report, revealing the importance of considering diagnosis of MCBH in suspected cases in lower age groups. Most of the patients come to see a doctor complain of abdominal pain, while some of them have no obvious clinical manifestations, and their cysts are usually discovered by accident. Also, some may suffer from obstructive jaundice and abdominal discomfort. The patient in this case came to our hospital because of abdominal distension, without any specific symptom. Consequently, patients should be diagnosed after auxiliary examination, especially pathological examination.
| Case No. | Ref. | Patients ’age (years)/Sex | Location | Size (cm) | Imaging or histological features | Treatment |
| 1 | Kobayashi et al[4], 2005 | 30/M | Seg VI | 3.6 | Embedded in a fibrous stroma and lined by low columnar or cuboidal epithelium | Partial resection |
| 2 | Zen et al[5], 2006 | 59/M | Seg IV | 4.2 | A relatively well-circumscribed nodule was enhanced on CT by contrast medium and sustained until the delayed phase | Left hepatectomy |
| 3 | 70/F | Seg III | 1.8 | A relatively well-circumscribed nodule | Segmentectomy | |
| 4 | 69/F | Seg III | 2.8 | Showed a multilocular cystic lesion containing many small cystic spaces | Segmentectomy | |
| 5 | Kai et al[6], 2008 | 55/M | Seg VI | 5.0 | Abdominal magnetic resonance imaging revealed as a low density area on T1-weighted images and a multiple bulboid high intensity area on T2-weighted images, respectively | Partial resection |
| 6 | Ryu et al[7], 2010 | 45/M | Seg VII | 2.0-3.5 (case nos. 6-8) | CT during arterial portography (CTAP) also shows that normal liver parenchyma can be found around the cystic lesions | Partial resection |
| 7 | 58/M | Seg III | CT (precontrast) shows multiple cysts and a small calcification | Partial resection | ||
| 8 | 55/F | Seg VI,VII | Partial resection | |||
| 9 | Song et al[2], 2013 | 52/M | Seg III | 2.7 | On T2-weighted MRI, conglomerated multiple cystic nodules with a high signal intensity were seen. Thin septae and the wall of the lesion were enhanced on contrast-enhanced, T1-weighted MRI | Partial resection |
| 10 | Beard et al[8], 2014 | 48/F | Seg VII | 4.7 | Microscopic exam demonstrated thick, dense fibrous tissue containing cytologically bland, large caliber bile ducts with intermingled benign hepatocytes | Extended right hepatectomy |
| 11 | Yoh et al[9], 2014 | 69/M | Seg III | 3.0 | The peripheral site of this lesion is slightly enhanced on the arterial phase. On the portal phase, the ring-enhancement of the lesion is clearer and shows honeycomb-like dilated bile duct | Left hepatectomy |
| 12 | Fernández-Carrión et al[10], 2014 | 60/F | Seg VI | 5.0 | Partial resection | |
| 13 | Tominaga et al[11], 2015 | 26/M | Seg V,VI | 10.0 | Histologically, these cystic lesions were composed of variably and irregularly dilated duct structures lined by columnar epithelium resembling bile duct lining. There were no atypical cells and no papillary growth of the epithelial cells | Right hepatectomy |
| 14 | Morinaga et al[12], 2017 | 53/M | left lobe of the liver | 12.0 | Enhanced abdominal computed tomography and magnetic resonance imaging (MRI) revealed a multicystic tumor with a calcified wall in the left lobe of the liver | Left hepatectomy |
| 15 | Ogura et al[13], 2018 | 77/F | Seg III | 12.0 | CT demonstrates a huge, low-density lesion with strong enhancement at the periphery | Partial resection |
| 16 | Mu et al[14], 2021 | 37/M | Seg VI | 8.0 | Calcification was observed in dilated ducts; The enhancement of the septa and peripheral wall within the cystic lesion (arterial phase); The lesion showed a low-density honeycomb-like appearance (venous phase) | Laparoscopic partial resection |
| Presentcase | 14/M | Seg III | 17.0 | A large, cystic, space-occupying lesion, with blurred outline with respect to adjacent liver structures | Laparoscopic partial resection |
According to the current published reports, the cysts are usually large and often larger than 2 cm (17 cm × 16 cm × 15 cm in our case), which can be differentiated from biliary microhamartomas; Further, MCBH is prone to develop in segment 3 in the left lobe and in segment 6 in the right lobe underneath the hepatic capsule[2]. In our case, MCBH was characterized by a space-occupying lesion with unclear boundary in the right lobe. Consistent with the features of the present case, the cystic wall of MCBHs are generally smooth without solid protrusions, and can be distinguished from cystic lesions with solid protrusions, for example, intraductal papillary neoplasm of the bile duct. MCBHs are mostly benign, and there is no report yet of distant metastases occurring in MCBH[11]. The cancer tissue is mainly composed of fibrous connective tissue, and not only in the glands that surround the biliary ducts but also in the areas between the dilated bile ducts[2]. Moreover, MCBHs are made up of bile ducts, peribiliary glands, and fibrous connective tissue that are rich in blood vessels histologically, but they are typically not connected to the hepatic ducts or biliary tree[7], consistent with the presently discussed cases. This is a distinguishing feature of MCBHs, which is different from Caroli’s disease, multiple hepatic cysts, and polycystic livers.
After MCBH was first described by von Meyenburg in the pathologic literature, the diagnostic standard for MCBHs remains contentious. Considering that the imaging features of MCBH are similar to those of other hepatic cystic diseases, making a differential diagnosis very challenging, we faced difficulties in establishing a preoperative diagnosis. However, MCBHs are characterized by the following distinctive features: Caroli’s disease often gives rise to atrophy of the relevant liver lobes and compensative hypertrophy of the rest of the hepatic lobes, but MCBHs will not cause such changes. Multiple hepatic cysts and polycystic livers are distributed randomly, with uneven distribution in the liver; whereas, MCBHs are distributed diffusely, mostly characterized by a distribution along the biliary tree. On magnetic resonance imaging, MCBHs are hyperintense on T2-weighted imaging with multicystic and honeycomb-like nodules, while they are hypointense on T1-weighted imaging. On ultrasound, the most concordant findings in MCBHs are a combination of uneven hypoechoic masses with hyperechoic cystic walls, which are usually revealed as low density with septate enhancement on CT.
In the case, spiral CT showed that the original upper abdominal mass disappeared after excision of the tumor. A dense linear image was seen in the left edge of the liver, and scattered pneumatosis was found in the abdomen, with mild effusion in the perihepatic and surgical area. An indwelling drainage tube was placed in the patient’s abdominal cavity after the surgery. Neither abnormal density lesions nor abnormal enhancing lesions were found in the liver parenchyma. Choledoch and bile ducts, both intrahepatic and extrahepatic, were not found to be dilated, with clear structures around the hepatic portap. The gallbladder was depicted clearly, within which there was no calculi showing high-density imaging; further, the gallbladder wall thickening and enhancement could be noticed. The patient showed good intervention adherence, surgical tolerance, and postoperative therapy. From the patient’s point of view, perceived physical discomfort was significantly eased, after treatment. The overall prognosis was satisfactory, and reexamination was recommended.
When the patients have MCBH, the symptoms may not very typical, and they require a combination of imaging and pathology for diagnosis. Under normal circumstances, the prognosis of MCBH is good. However, in patients with MCBH, more cases need to be observed for verification.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Augustin G, Croatia; Bessone F, Argentina; Gálvez Salazar P, Ecuador; Zharikov YO, Russia S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Martin DR, Kalb B, Sarmiento JM, Heffron TG, Coban I, Adsay NV. Giant and complicated variants of cystic bile duct hamartomas of the liver: MRI findings and pathological correlations. J Magn Reson Imaging. 2010;31:903-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Song JS, Noh SJ, Cho BH, Moon WS. Multicystic biliary hamartoma of the liver. Korean J Pathol. 2013;47:275-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Venkatanarasimha N, Thomas R, Armstrong EM, Shirley JF, Fox BM, Jackson SA. Imaging features of ductal plate malformations in adults. Clin Radiol. 2011;66:1086-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Kobayashi A, Takahashi S, Hasebe T, Konishi M, Nakagohri T, Gotohda N, Kinoshita T. Solitary bile duct hamartoma of the liver. Scand J Gastroenterol. 2005;40:1378-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Ryu Y, Matsui O, Zen Y, Ueda K, Abo H, Nakanuma Y, Gabata T. Multicystic biliary hamartoma: imaging findings in four cases. Abdom Imaging. 2010;35:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Kai K, Takahashi T, Miyoshi A, Yasui T, Tokunaga O, Miyazaki K. Intrahepatic multicystic biliary hamartoma: report of a case. Hepatol Res. 2008;38:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Zen Y, Terahata S, Miyayama S, Mitsui T, Takehara A, Miura S, Nobata K, Kitao A, Kakuda K, Kiyohara K, Nakanuma Y. Multicystic biliary hamartoma: a hitherto undescribed lesion. Hum Pathol. 2006;37:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Beard RE, Yee EU, Mortele KJ, Khwaja K. Multicystic biliary hamartoma: A report of a rare entity and a review of the literature. Int J Surg Case Rep. 2014;5:919-923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Fernández-Carrión MJ, Robles Campos R, López Conesa A, Brusadín R, Parrilla Paricio P. Intrahepatic Multicystic Biliary Hamartoma: Presentation of a case report. Cir Esp. 2015;93:e103-e105. [PubMed] [DOI] [Full Text] |
| 10. | Yoh T, Okamura R, Nakayama H, Lin X, Nakamura Y, Kato T. Multicystic biliary hamartoma mimicking intrahepatic cholangiocarcinoma: report of a case. Clin J Gastroenterol. 2014;7:418-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Tominaga T, Abo T, Kinoshita N, Murakami T, Sato Y, Nakanuma Y, Harada K, Masuda J, Nagayasu T, Nanashima A. A variant of multicystic biliary hamartoma presenting as an intrahepatic cystic neoplasm. Clin J Gastroenterol. 2015;8:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Morinaga T, Imai K, Yamashita YI, Yamao T, Kaida T, Nakagawa S, Hashimoto D, Chikamoto A, Sumiyoshi S, Mikami Y, Baba H. Multicystic biliary hamartoma with extremely elevated CA19-9: a case report. Scand J Gastroenterol. 2017;52:916-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Ogura T, Kurisu Y, Miyano A, Higuchi K. A huge rapidly-enlarging multicystic biliary hamartoma. Dig Liver Dis. 2018;50:723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Mu W, Su P, Ning S. Case Report: Incidentally Discovered a Rare Cystic Lesion of Liver: Multicystic Biliary Hamartoma. Pathol Oncol Res. 2021;27:628323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |