Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8768
Peer-review started: April 4, 2022
First decision: June 16, 2022
Revised: June 20, 2022
Accepted: July 8, 2022
Article in press: July 8, 2022
Published online: August 26, 2022
Processing time: 133 Days and 17.5 Hours
Thyroid storm is a life-threatening emergency. Reportedly, the prevalence of thyroid storm is 1%-2% among patients admitted to the hospital for thyrotoxicosis. Burch and Wartofsky (1993) introduced a scoring system using precise clinical criteria to identify thyroid storms. Only 17 cases of thyroid storm with a score > 70 points have been reported. Although thyroid storms are uncommon, their clinical findings resemble those of sepsis.
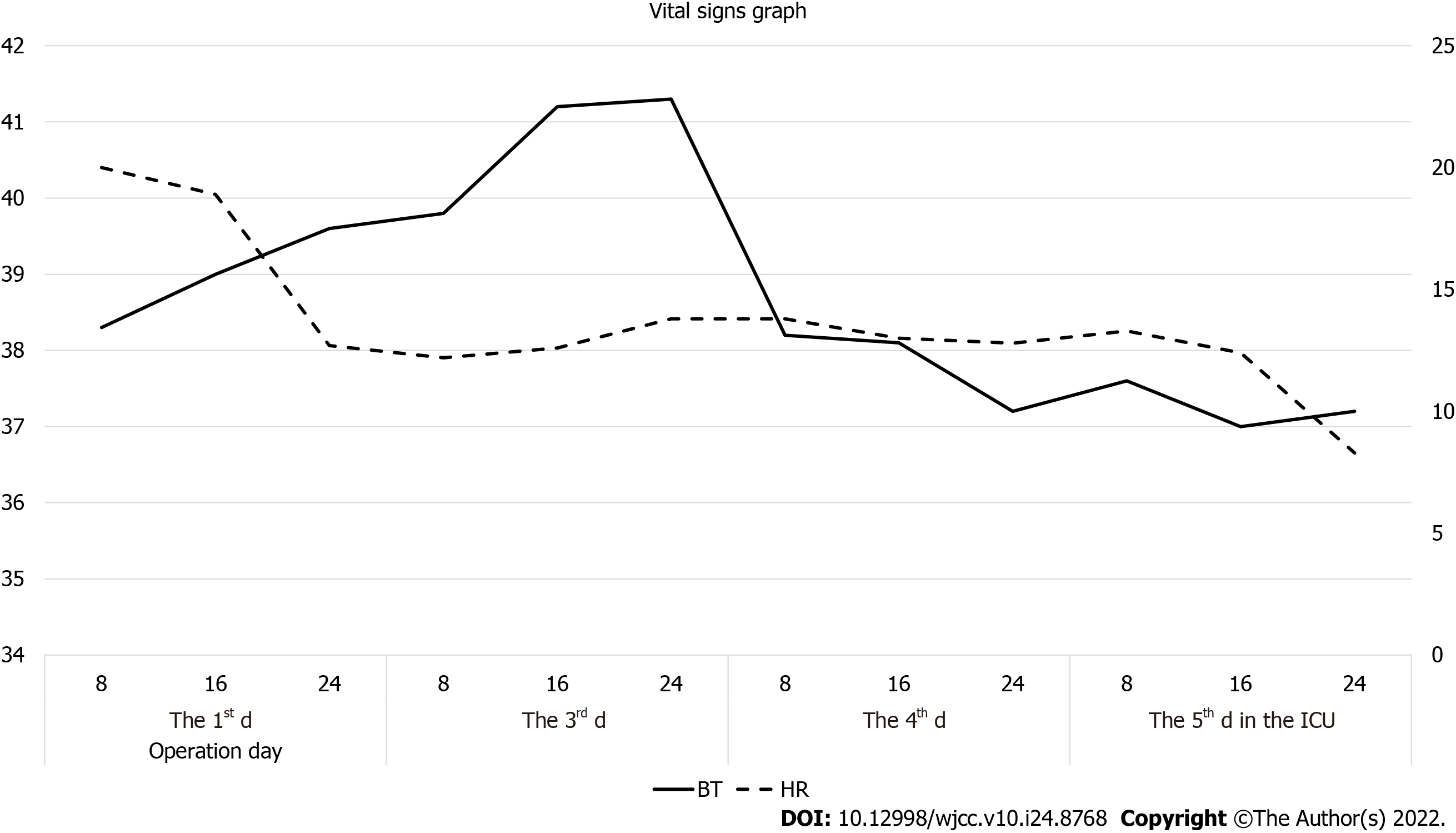
A 48-year-old man was referred to the emergency room from a local clinic owing to suspicion of gastric ulcer perforation; medications for hypertension, diabetes mellitus, and hyperthyroidism had been suspended 1 year prior to this visit. We performed an emergency distal gastrectomy with Billroth II anastomosis for gastric cardia cancer perforation, and the patient was referred to the surgical intensive care unit (ICU). On the 2nd d in the ICU, his body temperature (BT) increased to 41.3 °C at 19:00, with the thyroid storm score (90 points) peaking at 18:00 (BT; 41.2ºC, pulse rate; 138/min, irritable status). The patient was administered propylthiouracil, intravenous glucocorticoids, acetaminophen, and Lugol’s solution daily. Subsequently, we performed bladder irrigation with cold saline using a Foley catheter and applied a hypothermic blanket to decrease the patient's BT. His vital signs were stable on the 8th day in the ICU.
Thyroid storms are uncommon, with few reports in the literature; however, their clinical findings resemble those of sepsis and require further investigation. Since an untreated thyroid storm results in a high mortality rate, it should be investigated when managing sepsis.
Core Tip: Since thyroid storm is a life-threatening emergency and mortality is high when treatment is delayed, thyroid function evaluation should not be overlooked when managing sepsis.
- Citation: Baik SM, Pae Y, Lee JM. High scored thyroid storm after stomach cancer perforation: A case report. World J Clin Cases 2022; 10(24): 8768-8774
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8768.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8768
Thyroid storm is a life-threatening emergency. Reportedly, the prevalence of thyroid storm 1%-2% among patients admitted to the hospital for thyrotoxicosis[1]. In a nationwide survey of hospitals in Japan, the incidence of thyroid storm in hospitalized patients was 0.22% among all patients with thyrotoxicosis and 5.4% of patients admitted to the hospital for thyrotoxicosis[2,3]. Thyroid storm can develop in patients with long-standing untreated hyperthyroidism and can be precipitated by an acute event such as thyroid or non-thyroidal surgery, trauma, infection, an acute iodine load, or parturition[4].
Recent data suggest that the mortality rate of thyroid storms is approximately 10%-30%[1,2]. Multiple organ failure is the most common cause of death, followed by congestive heart failure, respiratory failure, arrhythmia, disseminated intravascular coagulation, gastrointestinal perforation, hypoxic brain syndrome, and sepsis[2,3].
Thyroid storm is diagnosed by clinical findings. Burch and Wartofsky (1993) introduced a scoring system using precise clinical criteria for the identification of thyroid storms[5]. Based on these criteria, a score of < 25 points indicates that a thyroid storm is unlikely; 25-44 points an impending thyroid storm; and ≥ 45 points, thyroid storm. There is no concept of a “severe” thyroid storm. However, to the best of our knowledge, only 17 cases of thyroid storm with a score > 70 points have been reported. Among these 17 cases, only four cases had a score of 90 points. Although thyroid storms are uncommon, their clinical findings resemble those of sepsis.
Here, we report a case of thyroid storm with a score of 90 points after gastric perforation surgery, and we analyze the “severe” form of thyroid storm (with a score > 70 points) in the 17 cases reported in the literature.
In the emergency room (ER), he complained of nausea, diffuse abdominal pain, general weakness, anorexia, and indigestion, which had started 4 d prior to admission.
A 48-year-old male patient was referred to the ER from a local clinic owing to suspicion of gastric ulcer perforation. We performed an emergent distal gastrectomy with Billroth II anastomosis for gastric cardia cancer perforation, a palliative surgery performed owing to peritoneal tumor seeding. The total operating time was 3 h and 55 min, and the patient's vital signs were stable during surgery. Postoperatively, the patient was referred to the surgical intensive care unit (ICU), and his vital signs were checked every hour.
He had a medical history of hypertension, type II diabetes mellitus (DM), and hyperthyroidism. One year ago, he had stopped taking medications for hypertension, DM, and hyperthyroidism.
The patient's personal and family history information could not be obtained.
On physical examination, he presented with hypoactive bowel sounds and direct tenderness in the epigastric area.
Laboratory examination in the ER showed the following results: white blood cell counts 12.5 × 103/µL, erythrocyte sedimentation rate 38 mm/h, and C-reactive protein 16.93 mg/dL.
The results of thyroid function tests are shown in Table 1. The free T4, T3, and T4 Levels exceeded the normal range, while thyroid stimulating hormone levels were below the normal range. The other laboratory results were non-specific.
| Hormone (normal range, unit) | At ER (preoperation) | Postop. day 6 | Postop. day 11 |
| T3 (60.0-181.0, ng/dL) | 625.4 | 79.9 | 94.1 |
| T4 (4.50-10.90, ng/dL) | 27.27 | 5.80 | 12.45 |
| fT4 (0.89-1.76, ng/dL) | 7.02 | 1.90 | 3.58 |
| TSH (0.55-4.78, uIU/mL) | < 0.008 | < 0.008 | < 0.008 |
Computed tomography in the ER revealed peritonitis due to gastric ulcer perforation and gastric malignancy with suspected peritoneal carcinomatosis.
On the 2nd d in the ICU, the patient’s body temperature (BT) increased to 41.3 °C at 19:00, and the thyroid storm score peaked at 18:00 (BT 41.2 °C; pulse rate: 138/min); furthermore, he was irritable; had a Glasgow Coma Scale score of E3V1M5, with eye opening to speech, no verbal response, and localized motor response to pain; and complained of severe pain (Table 2). The patient's highest score for a thyroid storm was 90.
| Case No. | Age/Gender | BT | CNS effect | GI-hepatic dysfx. | CV dysfx. | HF | Pre. Hx. | Total | Mortality | Ref. |
| 1 | 40/Male | 20 | 30 | 20 | 35 | 10 | 0 | 115 | No | Shimoda et al[8], 2014 |
| 2 | 50/Female | 0 | 20 | 0 | 35 | 5 | 10 | 90 | No | Izumi et al[9], 2009 |
| 3 | 48/Male | 10 | 10 | 20 | 25 | 10 | 10 | 85 | No | Sasaki et al[10], 2011 |
| 4 | 30/Female | 15 | 30 | 0 | 25 | 0 | 10 | 80 | Yes | Yamaji et al[11], 1991 |
| 5 | 43/Male | 10 | 20 | 10 | 25 | 5 | 10 | 80 | No | Diaz et al[12], 2009 |
| 6 | 62/Female | 20 | 0 | 10 | 25 | 15 | 0 | 70 | No | Jha et al[13], 2012 |
| 7 | 55/Female | 0 | 20 | 10 | 25 | 5 | 10 | 70 | No | Ogiso et al[14], 2008 |
| 8 | 56/Female | 0 | 20 | 20 | 20 | 10 | 0 | 70 | No | Yoshino et al[15], 2010 |
| 9 | 50/Male | 15 | 10 | 10 | 25 | 0 | 10 | 70 | Yes | Hosojima et al[16], 1992 |
| 10 | 51/Female | 15 | 10 | 0 | 25 | 15 | 10 | 75 | No | Nai et al[17], 2018 |
| 11 | 52/Male | 5 | 20 | 10 | 30 | 10 | 0 | 75 | No | Andrade et al[18], 2018 |
| 12 | 36/Female | 20 | 10 | 0 | 20 | 15 | 10 | 75 | No | Sugiyama et al[19], 2017 |
| 13 | 24/Female | 30 | 10 | 10 | 25 | 0 | 10 | 85 | No | McMillen et al[20], 2016 |
| 14 | 63/Male | 20 | 10 | 0 | 35 | 5 | 0 | 70 | No | Snyder et al[21], 2020 |
| 15 | 59/Female | 10 | 20 | 10 | 25 | 0 | 10 | 75 | No | Osada et al[22], 2011 |
| 16 | 50/Female | 15 | 20 | 10 | 35 | 10 | 0 | 90 | No | Umezu et al[23], 2013 |
| 17 | 41/Female | 10 | 10 | 10 | 35 | 15 | 10 | 90 | No | Kulaksizoglu et al[24], 2012 |
| 18 | 48/Male | 30 | 10 | 20 | 20 | 0 | 10 | 90 | No | Present case |
The patient was administered a daily dose of oral propylthiouracil (PTU) 800 mg, PTU enema 400 mg, intravenous glucocorticoids 40 mg, oral acetaminophen 650 mg, and oral Lugol’s solution 1.5 mL. Subsequently, we performed bladder irrigation with cold saline using a Foley catheter and applied a hypothermic blanket to decrease the patient's BT.
On the 3rd d in the ICU, the PTU dose was increased to 1200 mg/d, while the doses of the other drugs were maintained. From the 4th day, the oral PTU dose was fixed at 200 mg, q6hd; Lugol’s solution (0.5 mL; q8hd) was also delivered. On the 9th d, the patient was referred to the general ward, with the administration of oral PTU 200 mg four times daily and tapering of glucocorticoid therapy.
The patient’s vital signs were stable from the 8th postoperative day, and he showed clear mental status on the 4th postoperative day (Figure 1). In the general ward, on the 15th day, the oral PTU dose was decreased to 200 mg three times daily. On the 29th hospital day, he was discharged with an asymptomatic status, stable vital signs, and a prescribed dose of oral PTU 200 mg three times daily.
We report a case of thyroid storm with extremely high fever (41.3 °C), typically associated with patient mortality. Indeed, high fever alone increases mortality in ICU patients[6].
While this patient’s BT was < 40 °C in the ER, it increased to > 40ºC postoperatively. Later, the patient presented with tachycardia (peaked at 138/min), irritability, and abdominal pain; he also had a history of hyperthyroidism, with a high score of 90 points in the thyroid storm scoring system, which reflects disease severity. Based on the scoring system, thyroid storms are considered unlikely for scores of < 25 points, while 25-45 points suggest impending storms; a score of > 45 points is highly associated with thyroid storms[5] (Table 2). Therefore, when the score approaches 45 points, the patient needs more intensive monitoring and re-evaluation for thyroid storm. The mortality risk associated with thyroid storm is estimated to be 8%-25%, despite modern advancements in treatment and supportive measures[7].
In this case, the extremely high BT (41.3 °C), elevated pulse rate (PR) (138/min), and altered Glasgow Coma Scale score (E3V1M5) observed on the 2nd day in the ICU were immediately considered to indicate thyroid storm, and treatment was initiated. Severity was assessed at the same time as the diagnosis using the scoring system. The patient was diagnosed with gastric ulcer perforation. Therefore, these symptoms may be considered as signs of sepsis.
To the best of our knowledge, there are some reports of cases with scores of < 70 points; however, there are only 17 reported cases with scores of ≥ 70 points[8-24] (Table 2). Among the 17 cases with scores of ≥ 70 points, two involved mortality. Case 1 involved the highest severity score, with 115 points. In case 1, the patient had no previous medical or family history of thyroid disease (0 points). Laboratory findings showed liver dysfunction with jaundice (20 points), while physical examination revealed the following: atrial flutter with a PR of 162/min (35 points), high fever (39.3 °C) (20 points), impaired consciousness (30 points), and reduced ejection fraction (43%) with moderate bilateral pleural effusion (10 points). The patient in case 1 was discharged from the hospital on day 94. In the two mortality cases, the severity scores were 80 and 70. In the mortality case with a severity score of 80 points, the central nervous system dysfunction score was very high (30 points). Meanwhile, in the mortality case with a severity score of 70 points, the cardiovascular dysfunction score was 25 points, which was relatively high compared to other scores. However, the total severity scores in the mortality cases were not relatively high compared to those of other thyroid storm cases. In all 18 cases, including our case, no correlation was found between the severity score and mortality; nevertheless, the number of cases is insufficient to draw a valid conclusion.
Comparing our case to the other 17 cases reported in the literature, we found that our patient presented with extremely high fever and a high severity score. In cases with the same score (cases 2, 16, 17, and 18 [present case]), the highest-scored factor differed between cases. Meanwhile, cases 2, 16, and 17 had high scores for cardiovascular dysfunction (PR > 140/min with atrial fibrillation), and the present case involved a high BT (41.3 °C).
High fever and tachycardia are the main parameters of systemic inflammatory response syndrome, as per the criteria established in 1991[25]. In the Sepsis-3 criteria, newly established in 2016, PR and BT were not included[26]. Although PR and BT were excluded from the diagnostic criteria for sepsis, they are still important in managing sepsis. On the other hand, thyroid storm is not a major consideration in ICU. Therefore, when uncontrolled fever or tachycardia is observed, it may be useful for the physician to consider evaluation of thyroid function. The reason is that sepsis-induced tachycardia and high fever are improved by appropriate sepsis management, but the signs induced by thyroid storm are different in treatment guidelines such as antithyroid agents, Lugol’s solution and steroid etc.
In general, thyroid function tests are not performed before emergency surgery for bowel perforation. Tachycardia and high fever are commonly observed postoperatively. However, since thyroid storm is a life-threatening emergency and mortality is high when treatment is delayed, thyroid function evaluation should not be overlooked when managing sepsis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Bains L, India; Chang YY, Taiwan; Kurniawati EM, Indonesia; Yang L, China S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Nayak B, Burman K. Thyrotoxicosis and thyroid storm. Endocrinol Metab Clin North Am. 2006;35:663-686, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 180] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, Monden T, Kouki T, Otani H, Teramukai S, Uehara R, Nakamura Y, Nagai M, Mori M; Japan Thyroid Association. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid. 2012;22:661-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 237] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 3. | Feldt-Rasmussen U, Emerson CH. Further thoughts on the diagnosis and diagnostic criteria for thyroid storm. Thyroid. 2012;22:1094-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Sherman SI, Simonson L, Ladenson PW. Clinical and socioeconomic predispositions to complicated thyrotoxicosis: a predictable and preventable syndrome? Am J Med. 1996;101:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am. 1993;22:263-277. [PubMed] |
| 6. | Erkens R, Wernly B, Masyuk M, Muessig JM, Franz M, Schulze PC, Lichtenauer M, Kelm M, Jung C. Admission Body Temperature in Critically Ill Patients as an Independent Risk Predictor for Overall Outcome. Med Princ Pract. 2020;29:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, Rivkees SA, Samuels M, Sosa JA, Stan MN, Walter MA. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016;26:1343-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2006] [Cited by in RCA: 1506] [Article Influence: 167.3] [Reference Citation Analysis (0)] |
| 8. | Shimoda Y, Satoh T, Takahashi H, Katano-Toki A, Ozawa A, Tomaru T, Horiguchi N, Kaira K, Nishioka M, Shibusawa N, Hashimoto K, Wakino S, Mori M, Yamada M. A case of thyroid storm with a markedly elevated level of circulating soluble interleukin-2 receptor complicated by multiple organ failure and disseminated intravascular coagulation syndrome. Endocr J. 2014;61:691-696. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Izumi K, Kondo S, Okada T. A case of atypical thyroid storm with hypoglycemia and lactic acidosis. Endocr J. 2009;56:747-752. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Sasaki K, Yoshida A, Nakata Y, Mizote I, Sakata Y, Komuro I. A case of thyroid storm with multiple organ failure effectively treated with plasma exchange. Intern Med. 2011;50:2801-2805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Yamaji Y, Hayashi M, Suzuki Y, Noya K, Yamamoto O. Thyroid crisis associated with severe hypocalcemia. Jpn J Med. 1991;30:179-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Diaz R, Blakey MD, Murphy PB, Cryar AK, Cmelak AJ. Thyroid storm after intensity-modulated radiation therapy: a case report and discussion. Oncologist. 2009;14:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Jha S, Waghdhare S, Reddi R, Bhattacharya P. Thyroid storm due to inappropriate administration of a compounded thyroid hormone preparation successfully treated with plasmapheresis. Thyroid. 2012;22:1283-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ogiso S, Inamoto S, Hata H, Yamaguchi T, Otani T, Koizumi K. Successful treatment of gastric perforation with thyrotoxic crisis. Am J Emerg Med. 2008;26:1065.e3-1065.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Yoshino T, Kawano D, Azuhata T, Kuwana T, Kogawa R, Sakurai A, Tanjoh K, Yanagawa T. A patient with Graves' disease who survived despite developing thyroid storm and lactic acidosis. Ups J Med Sci. 2010;115:282-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Hosojima H, Iwasaki R, Miyauchi E, Okada H, Morimoto S. Rhabdomyolysis accompanying thyroid crisis: an autopsy case report. Intern Med. 1992;31:1233-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Nai Q, Ansari M, Pak S, Tian Y, Amzad-Hossain M, Zhang Y, Lou Y, Sen S, Islam M. Cardiorespiratory Failure in Thyroid Storm: Case Report and Literature Review. J Clin Med Res. 2018;10:351-357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Andrade Luz I, Pereira T, Catorze N. Thyroid storm: a case of haemodynamic failure promptly reversed by aggressive medical therapy with antithyroid agents and steroid pulse. BMJ Case Rep. 2018;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Sugiyama Y, Tanaka R, Yoshiyama Y, Ichino T, Hishinuma N, Shimizu S, Imai N, Mitsuzawa K, Kawamata M. A case of sudden onset of thyroid storm just before cesarean section manifesting congestive heart failure and pulmonary edema. JA Clin Rep. 2017;3:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | McMillen B, Dhillon MS, Yong-Yow S. A rare case of thyroid storm. BMJ Case Rep. 2016;2016:10.1136/bcr-2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Snyder S, Joseph M. The Perfect Storm: A Case of Ischemic Stroke in the Setting of Thyroid Storm. Cureus. 2020;12:e7992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Osada E, Hiroi N, Sue M, Masai N, Iga R, Shigemitsu R, Oka R, Miyagi M, Iso K, Kuboki K, Yoshino G. Thyroid storm associated with Graves' disease covered by diabetic ketoacidosis: A case report. Thyroid Res. 2011;4:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Umezu T, Ashitani K, Toda T, Yanagawa T. A patient who experienced thyroid storm complicated by rhabdomyolysis, deep vein thrombosis, and a silent pulmonary embolism: a case report. BMC Res Notes. 2013;6:198. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Kulaksizoglu M, Gonen MS, Kebapcilar L, Sahin F, Acikgoz B, Demir T, Dincturk E. Multiorgan dysfunction accompanied with metimazole and thyroid storm. Transfus Apher Sci. 2012;46:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6211] [Cited by in RCA: 6522] [Article Influence: 197.6] [Reference Citation Analysis (0)] |
| 26. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17171] [Article Influence: 1907.9] [Reference Citation Analysis (2)] |