Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8695
Peer-review started: February 23, 2022
First decision: March 24, 2022
Revised: April 4, 2022
Accepted: July 20, 2022
Article in press: July 20, 2022
Published online: August 26, 2022
Processing time: 173 Days and 10.4 Hours
Retinoblastoma (Rb) is primarily found in infants or young children. The most common primary presenting sign of Rb is leukocoria. Rb is very rare in children who are 10 years old or older. Timely and correct diagnosis as well as proper treatment are the key factors affecting the prognosis of Rb.
A 10-year-old girl with symptoms of vision loss, redness, swelling and pain in the right eye for 2 mo was admitted to our Department of Ophthalmology. The visual acuity of the right eye was graded as hand movement. The intraocular pressure of the eye was 46.9 mmHg. No substantial space-occupying lesion or characteristic calcified plaque was found in the eye. The patient underwent anterior chamber irrigation under general anesthesia on the same day of admission, and 2 mL of irrigation solution was saved for pathological examination. Histopathological examination of the anterior chamber fluid revealed cancer cells. A diagnosis of Rb with masquerade syndrome was made. The patient underwent enucleation followed by 6 rounds of systematic chemotherapy. A follow-up examination almost 9 years later found no relapse of Rb.
For older pediatric patients who have secondary glaucoma and uveitis symptoms without a clear cause of the disease and have no space-occupying lesion found by imaging examination, aqueous humor or vitreous humor examination is recommended for timely and correct diagnosis and appropriate treatment.
Core Tip: Retinoblastoma (Rb) is most commonly found in young pediatric patients, and is very rare in patients who are 10 years old or older. Here, we report a case of Rb in a 10-year-old girl with secondary glaucoma and other uveitis symptoms as clinical presenting signs. No obvious space-occupying lesions were found in the eye by imaging examination. However, anterior chamber fluid examination found cancer cells and was decisive in the diagnosis of Rb. This suggests the necessity of aqueous humor or vitreous humor examination in the diagnosis of Rb with atypical clinical symptoms.
- Citation: Zhang Y, Tang L. Retinoblastoma in an older child with secondary glaucoma as the first clinical presenting symptom: A case report. World J Clin Cases 2022; 10(24): 8695-8702
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8695.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8695
Retinoblastoma (Rb) is a type of cancer mostly found in infants or young children and can present unilaterally or bilaterally. It is the most common pediatric eye cancer and primarily originates in the eye, with an incidence of 1:16000 to 1:18000 in newborns[1,2]. It has been reported that two-thirds of Rb is found in patients younger than 3 years old. The incidence of Rb in children 5 years old or older is less than 5%, and it is very rare in children 10 years old or older[3].
Currently, the survival rate of Rb patients in developed countries has reached 95%, while it is only 50% worldwide. In addition to the difference in medical conditions and economic conditions in different countries, misdiagnosis and cancer metastasis were the main reasons for the death of patients. Therefore, timely and correct diagnosis is critical for the prognosis of patients.
The most common clinical symptom of Rb to present first is leukocoria. It represents 90% of the first clinical symptoms of Rb, followed by strabismus, redness and pain, proptosis and other signs[4]. However, in addition to the typical symptoms, Rb can also present with other atypical symptoms, such as conjunctival edema, pseudohypopyon in the anterior chamber, pseudocellulitis of the orbit and secondary intraocular hypertension, which may result in the wrong diagnosis and an inappropriate treatment plan. Current treatment of Rb includes cryotherapy, laser photocoagulation, systemic chemotherapy, enucleation, and local chemotherapy through intraocular, peribulbar and ophthalmic artery interventional approaches. In the present study, we reported a case of Rb in a 10-year-old girl with secondary glaucoma and uveitis symptoms as the presenting clinical signs. The diagnosis and treatment procedures were described and discussed.
A 10-year-old girl was admitted to the Department of Ophthalmology at West China Hospital, Sichuan University, on December 10, 2012, due to vision loss accompanied by redness, swelling, and pain in the right eye.
The patient started to suffer gradual vision loss with redness, swelling, and pain in the right eye 2 mo prior to hospital admission and was diagnosed with uveitis and secondary glaucoma in a local hospital. The prescribed treatment was dexamethasone ophthalmic, Azopt ophthalmic and atropine eye ointment. The symptoms were not relieved after treatment. The patient denied fever, headache, coughing, ulcer, skin diseases or arthropathy during the doctor visit.
There was no remarkable illness history.
There was no remarkable personal or family history.
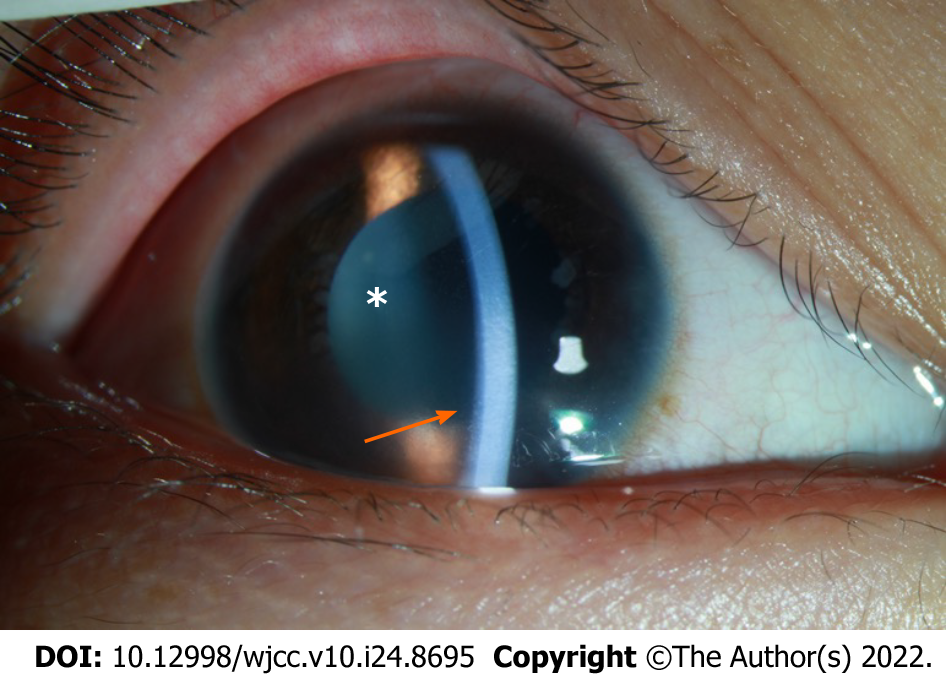
At the time of hospitalization, the visual acuity of the patient’s right eye was hand movement; the visual acuity of the left eye was 20/20. Intraocular pressure of the right eye was 46.9 mmHg, and the left eye was 19.8 mmHg (1 mmHg = 0.133 kPa). The result of the ophthalmological examination was as follows: mutton-fat KP grading: ++; anterior chamber cell grading: +++. Multiple white, round nodules were found on the right eye near the pupillary margin on the surface of the iris (Figure 1). The dilated pupil size of the right eye was 5 mm with a slower response to light. The lens was clear, and the vitreous body was opaque. The optic cup/optic disc (C/D) ratio was approximately 0.55. Retinal edema with a bluish color was found in the right eye. The superior temporal retina was pale, with a portion of the vessels being occluded and line-like (Figure 2). No abnormalities were found in the anterior segment or the fundus of the left eye.
The white blood cell count was 13.02 × 109/L, and the percentage of segmented neutrophils was 65.8%.
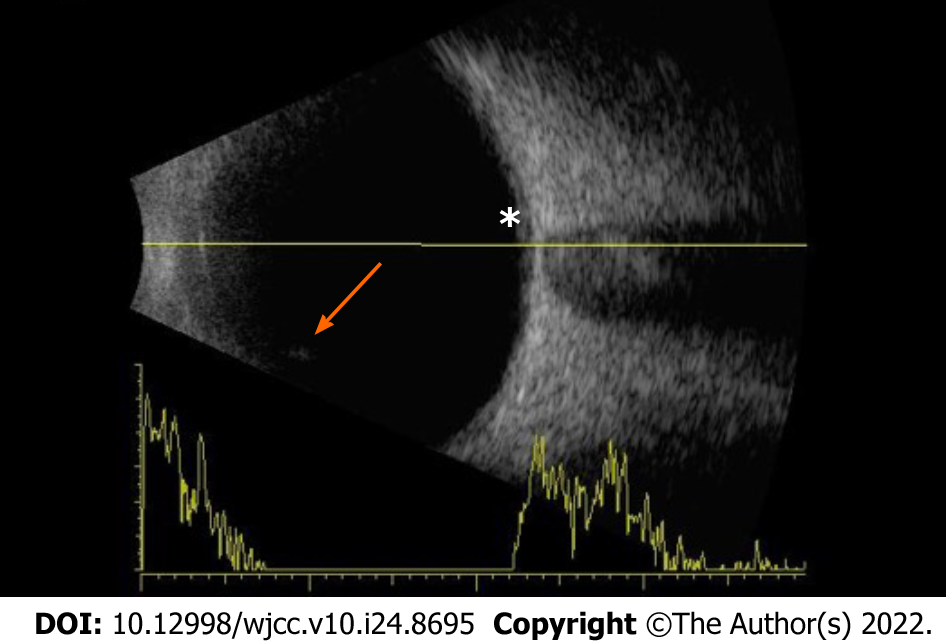
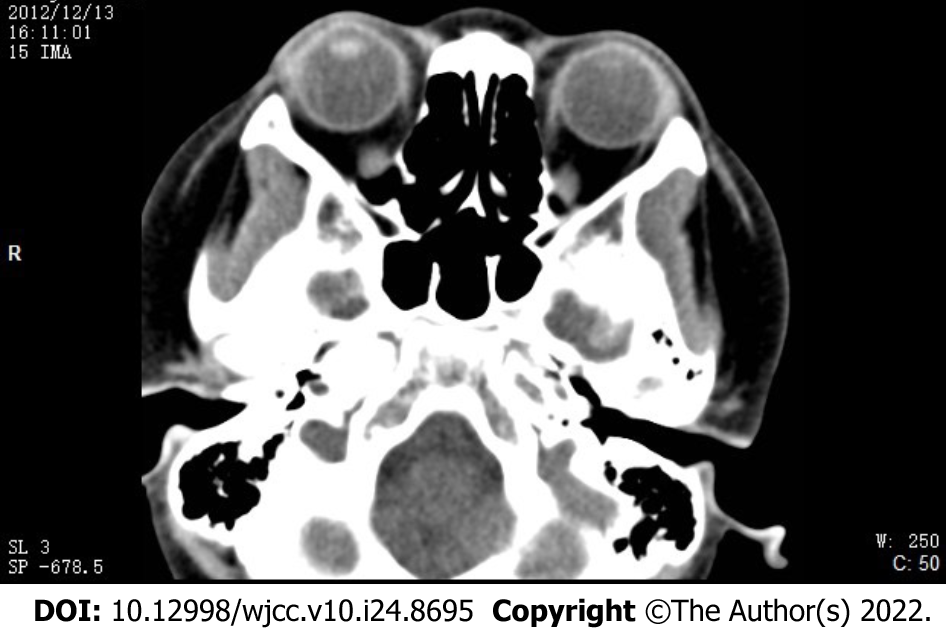
The results of the B-mode ultrasound of the eyes suggested vitreous opacity and retinal edema in the right eye. No obvious space-occupying lesion was found intraocularly in the right eye (Figure 3). Ultrasound biomicroscopy examination found multiple ciliary body cysts (Figure 4). The results of computerized tomography (CT) scanning in the axial view and coronal view suggested normal findings in terms of eyeball shape. No space-occupying, intraocular or intraorbital lesions were found (Figure 5).
The pathological examination result was as follows: Cancer cells were seen by the liquid-based smear of the aqueous humor of the right eye. Immunocytochemical staining results found CD56 (+), Syna (+), CgA (+, but sporadic), PCK (-), Des (-), LCA (-), and 70% in terms of Ki-67 positivity.
The preliminary diagnosis was secondary glaucoma with undetermined causes, conjunctiva hyperemia and corneal edema with haze in the right eye. The patient underwent an anterior chamber irrigation procedure under general anesthesia on the day of hospitalization. The immunocytochemical examination results revealed cancer cells in the anterior chamber fluid. The final diagnosis was stage E Rb in the right eye based on the histopathological examination result of the enucleated eye tissue and other findings.
The patient first underwent anterior chamber irrigation under general anesthesia on the same day as hospital admission in the Department of Emergency Medicine. Two milliliters of irrigation solution was saved for pathological examination. After cancer cells were found in the anterior chamber fluid, the patient underwent enucleation and prosthetic eye table implantation surgery in the right eye (affected eye) under general anesthesia. The patient was then transferred to the Department of Oncology for 6 rounds of systematic chemotherapy by intravenous infusion with vincristine, etoposide, and carboplatin once a week.
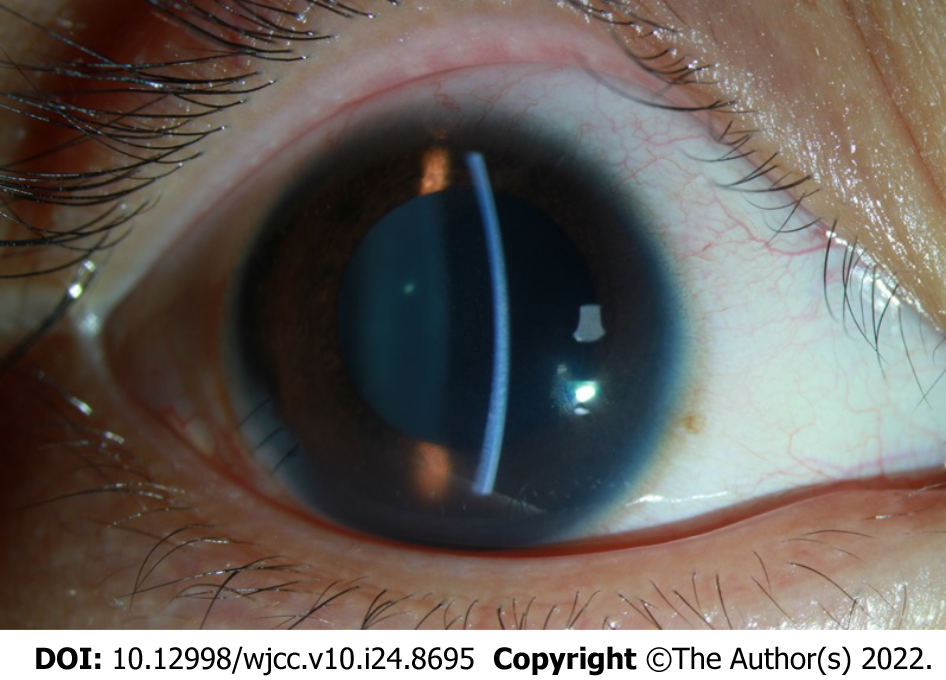
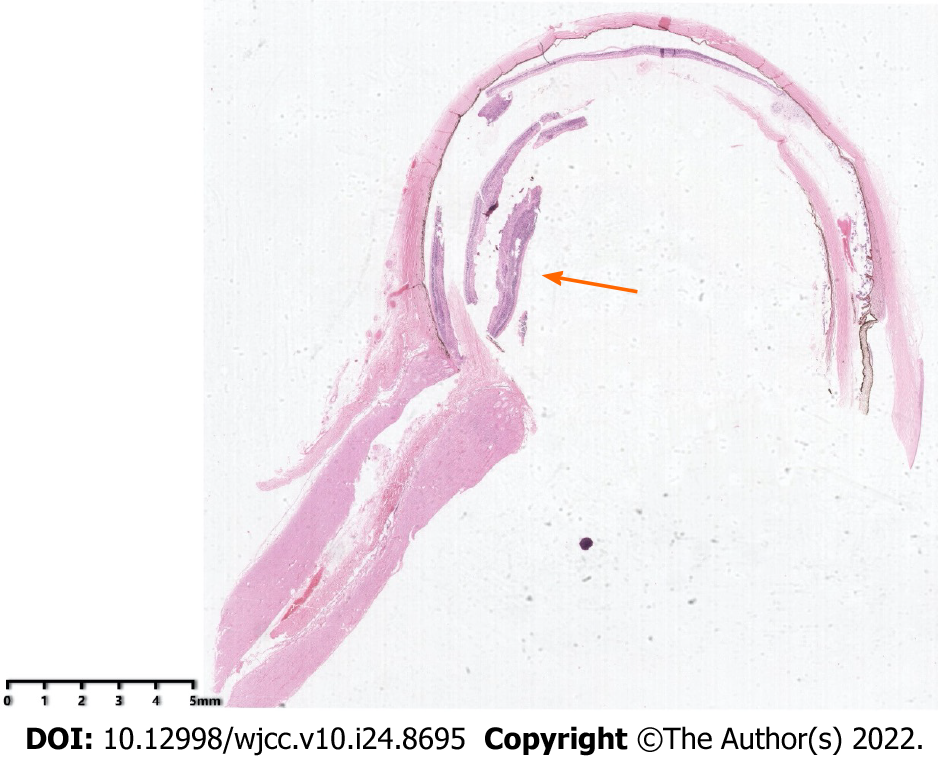
On the first day after the anterior chamber irrigation procedure, the visual acuity of the right eye (affected eye) was graded as hand movement. The intraocular pressure decreased to 13 mmHg. The cornea was clear. Anterior chamber cell grading was ++. No white nodules were found on the surface of the iris (Figure 6), and the vitreous body was opaque. Fundus examination results showed extensive retinal edema with sporadic bleeding in the macula and subretinal area (Figure 7). No abnormalities were found in the anterior segment or the fundus of the left eye. On the fourth day after the procedure, the intraocular pressure increased to 40 mmHg again. After enucleation and prosthetic eye table implantation, the histopathological examination results of the enucleated eye showed a white mass from the center of the pupil, with a size of 0.3 cm × 0.2 cm × 0.1 cm (Figure 8). No tumor cells were found in the lamina cribrosa of the optic nerve. The patient did not regularly visit the hospital for follow-up visits after chemotherapy.
In September 2021, the patient came to our department for a follow-up visit. The examination found the overall health of the right eye was as follows: a prosthetic eye was implanted into the right eye. No symptoms in the left eye were reported. Eye examination results showed that the size and morphology of both eyes were symmetric, and the position of the prosthetic eye and the eye table in the right eye was proper. The vision of the left eye was 20/63 without correction and 20/20 with correction. Examination results of the left eye were as follows: the intraocular pressure of the left eye was 14.8 mmHg; the cornea and lens were clear; the anterior chamber was clear with normal depth; and no abnormalities were found in the fundus.
In the present case, we report a case of stage E Rb with atypical symptoms in a 10-year-old girl. More than 3 dozen Rb patients older than 10 years of age have been reported in the literature. Singh et al[5] reviewed 24 cases up to 2011. Domínguez-Varela et al[6] also described one case each in 2021. All were sporadic and, similar to our patient, unilateral[5,6]. Although the cure rate of Rb is relatively high, misdiagnosis and cancer metastasis are the main obstacles for further improvement of the prognosis of Rb. At the late stage, Rb tumor cells can invade the optic nerve and orbital tissue and metastasize to the intracranial region, circulatory system or lymph nodes, thereby endangering patients’ lives[7]. The primary treatment strategy for Rb is enucleation of the affected eye(s), which results in a cure rate as high as 95%[8]. If the tumor mass breaks the sclera and spreads out of the eye or breaks the lamina cribrosa and invades the optic nerve, the tumor is considered extraocular Rb, and systematic chemotherapy and regional radiotherapy are required to treat the patient in addition to eye enucleation. At this stage, the 5-year survival rate is 55%-60%[9].
Typically, a diagnosis of Rb could be made based on the following clinical observations: the patient’s age is younger than 3 years old; the presence of typical Rb symptoms, such as leukocoria and strabismus; yellow or white lesions found in the fundus with spreading lesions in the vitreous body or retina; retina detachment; and intraocular space-occupying lesions or calcified plaques found by imaging examinations. However, in the present case, the patient was 10 years old, and the first clinical symptoms were redness and pain in the right eye caused by acute high intraocular pressure, a result of uveitis. Multiple B-mode ultrasounds or CT examinations failed to find substantial space-occupying lesions or characteristic calcified plaques in the eye, which led to misdiagnosis initially. The diagnosis of malignant tumor combined with masquerade syndrome was made 2 mo after the initial doctor visit by histopathological examination of the anterior chamber fluid. Masquerade syndromes are disorders presenting with clinical symptoms similar to those of uveitis, but the disorders are malignant eye cancers. The syndromes are often seen in Rb, choroidal malignant melanoma, intraocular non-Hodgkin's lymphoma, and cancers metastasized to the eyes[10,11]. Aqueous humor or vitreous humor examination is the primary method used to distinguish masquerade syndrome from uveitis. Vitreous humor examination is superior to aqueous humor examination in regard to cancer cell screening rate. For diffuse anterior Rb, aqueous humor examination is adequate for diagnosis[12,13].
From this case, we were able to determine several pieces of information. First, the primary cause of misdiagnosis in the present case was the diversity and non-specificity of masquerade syndrome. For patients with secondary glaucoma who do not have a clear cause of the disease and a satisfactory result from the treatment for ocular hypertension, the possibility of cancer should be considered. The key step in treating secondary glaucoma without a clear cause of the disease is to correctly identify the cause of the disease. Second, for older pediatric Rb patients, the symptoms and signs are often not typical for Rb, such as conjunctival edema, pseudohypopyon in the anterior chamber, pseudocellulitis of the orbit and secondary intraocular hypertension. Patients with these symptoms are easily misdiagnosed as uveitis or infectious endophthalmitis. However, the pseudohypopyon presented in this case is different from the hypopyon found in patients with infectious endophthalmitis, which is characterized by yellow or white, thick empyema in the anterior chamber. The manifestations of pseudohypopyon are the accumulation of gray or white, different sized, granular or sponge-like tumor cells seeded in the lower part of the anterior chamber or diffusely seeded in the anterior chamber, the surface of the iris or the surface of the lens. Sometimes snowball-like or lumpy opaque nodules can be found in the vitreous cavity due to the seeding of cancer cells in older pediatric Rb patients. Third, for highly suspected intraocular cancer patients with atypical symptoms but without confirmative imaging examination results, anterior chamber fluid or vitreous fluid examination should be performed as soon as possible to make a correct diagnosis[14]. Last, the primary goal of Rb treatment was saving the patient’s life, followed by the saving of the affected eyes and visual functions. For patients with late-stage Rb, enucleation with systematic chemotherapy and regional radiotherapy is recommended to improve the chance of survival of the patient[15,16].
We successfully diagnosed and treated a 10-year-old girl with stage E Rb with secondary glaucoma and other atypical symptoms as the first clinical manifestations. For such patients who have secondary glaucoma without a clear cause, the possibility of a malignant tumor should be considered.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Di Meglio L, Italy; Salimi M, Iran S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | AlAli A, Kletke S, Gallie B, Lam WC. Retinoblastoma for Pediatric Ophthalmologists. Asia Pac J Ophthalmol (Phila). 2018;7:160-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 2. | Broaddus E, Topham A, Singh AD. Incidence of retinoblastoma in the USA: 1975-2004. Br J Ophthalmol. 2009;93:21-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 249] [Article Influence: 14.6] [Reference Citation Analysis (1)] |
| 3. | Dimaras H, Kimani K, Dimba EA, Gronsdahl P, White A, Chan HS, Gallie BL. Retinoblastoma. Lancet. 2012;379:1436-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 473] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 4. | Fabian ID, Onadim Z, Karaa E, Duncan C, Chowdhury T, Scheimberg I, Ohnuma SI, Reddy MA, Sagoo MS. The management of retinoblastoma. Oncogene. 2018;37:1551-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 165] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 5. | Singh SK, Das D, Bhattacharjee H, Biswas J, Kuri G, Bhattacharjee K, Deka H, Deka AC. A rare case of adult onset retinoblastoma. Oman J Ophthalmol. 2011;4:25-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Domínguez-Varela IA, Aguilera-Partida JA, Dalvin LA, Garza-Garza LA, Thompson-García LM, Barbosa-Quintana Á, Ancona-Lezama D. Retinoblastoma in an older Hispanic child masquerading as pars planitis: A case report. Eur J Ophthalmol. 2022;32:NP71-NP74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Ray A, Gombos DS, Vats TS. Retinoblastoma: an overview. Indian J Pediatr. 2012;79:916-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | McDaid C, Hartley S, Bagnall AM, Ritchie G, Light K, Riemsma R. Systematic review of effectiveness of different treatments for childhood retinoblastoma. Health Technol Assess. 2005;9:iii, ix-ix, 1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Lee JH, Han JW, Hahn SM, Lyu CJ, Kim DJ, Lee SC. Combined intravitreal melphalan and intravenous/intra-arterial chemotherapy for retinoblastoma with vitreous seeds. Graefes Arch Clin Exp Ophthalmol. 2016;254:391-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Peng MY, Kersten RC. The Masquerade Syndrome. JAMA Ophthalmol. 2017;135:161-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Mehrabi Z, Salimi M, Niknam K, Mohammadi F, Mamaghani HJ, Sasani MR, Ashraf MJ, Salimi A, Zahedroozegar MH, Erfani Z. Sinoorbital Mucormycosis Associated with Corticosteroid Therapy in COVID-19 Infection. Case Rep Ophthalmol Med. 2021;2021:9745701. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Zhang MF. The diagnostic investigations should be efficient for patients with uveitis. Zhonghua Yanke Zazhi. 2017;53:721-723. |
| 13. | Yang M, Yan JH. Diagnosis and treatment of masquerade syndrome, an analysis of 14 cases. Zhongguo Shiyong Yanke Zazhi. 2012;30:994-997. |
| 14. | Brennan RC, Qaddoumi I, Billups CA, Free TL, Haik BG, Rodriguez-Galindo C, Wilson MW. Comparison of high-risk histopathological features in eyes with primary or secondary enucleation for retinoblastoma. Br J Ophthalmol. 2015;99:1366-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Wei WB, Zhou N. Attach importance to standardized treatment of retinoblastoma to improve its treatment outcome. Zhonghua Yandibing Zazhi. 2020;36:413-418. |
| 16. | Faranoush M, Mehrvar N, Tashvighi M, Fabian ID, Zloto O, Bascaran C, Ghorbani R, Ghasemi F, Naseripour M, Sedaghat A, Alebouyeh M, Mehrvar A. Retinoblastoma presentation, treatment and outcome in a large referral centre in Tehran: a 10-year retrospective analysis. Eye (Lond). 2021;35:575-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |