Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8679
Peer-review started: February 14, 2022
First decision: March 24, 2022
Revised: April 3, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 26, 2022
Processing time: 182 Days and 1.7 Hours
Lichen planus (LP) with distribution of lesions along Blaschko’s lines is a rare entity, accounting for 0.24%-0.62% of all patients. Unilateral distribution of lesions in arm, leg, trunk, and waist is even less common. Approximately 10% of patients with LP manifest nail lesions.
A 20-year-old woman presented to our department with polygonal, purpuric, flat-topped papules over the right arm, right leg, and right side of trunk and waist for the last 5 mo. The patient initially developed nail deformation in the left middle finger with no obvious cause, followed by development of blue-purple and red maculopapular rash with pruritus. During the disease course, the skin lesions aggravated and spread to several segments due to scratching. The lesions showed unilateral distribution along the Blaschko’s lines. The diagnosis of LP along Blaschko’s lines was established based on dermoscopy and skin biopsy. Her cutaneous lesions considerably improved after 4-wk treatment with intramuscular glucocorticoid, oral acitretin, topical glucocorticoid, and retinoids.
Cases of LP involving multiple segments of the body along the Blaschko’s lines with nail damage are rare.
Core Tip: Lichen planus (LP) with lesion distribution along the Blaschko’s lines can be differentiated from other skin lesions with linear distribution by dermoscopy and pathological biopsy. The isotopic response can occur in patients with LP, which may be an important cause for rapid spread of lesions and involvement of multiple segments. Therefore, early diagnosis and treatment are of great significance. Treatment strategy should be individualized based on the lesion characteristics and patient acceptance. Our patient showed considerable improvement of cutaneous lesions after 4-wk treatment with intramuscular glucocorticoid, oral acitretin, topical glucocorticoid and retinoids.
- Citation: Dong S, Zhu WJ, Xu M, Zhao XQ, Mou Y. Unilateral lichen planus with Blaschko line distribution: A case report. World J Clin Cases 2022; 10(24): 8679-8685
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8679.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8679
Although cases of lichen planus (LP) are not uncommon, LP with lesion distribution along the Blaschko’s lines is a rare entity, accounting for only 0.24%-0.62% of all patients with LP[1]. Cases with unilateral involvement of upper and lower limbs, chest, back, and waist are even rarer. Approximately 10% of patients with LP have nail lesions[2]. We report a rare case of LP with unilateral distribution of cutaneous lesions along the Blaschko’s lines along with nail lesions. Our experience with this case may provide insights into this rare disease and facilitate timely diagnosis and treatment of this disease.
On September 24, 2021, a 20-year-old woman presented to our department with polygonal, purpuric, flat-topped papules over her right arm, right leg, and right side of trunk and waist since the last 5 mo.
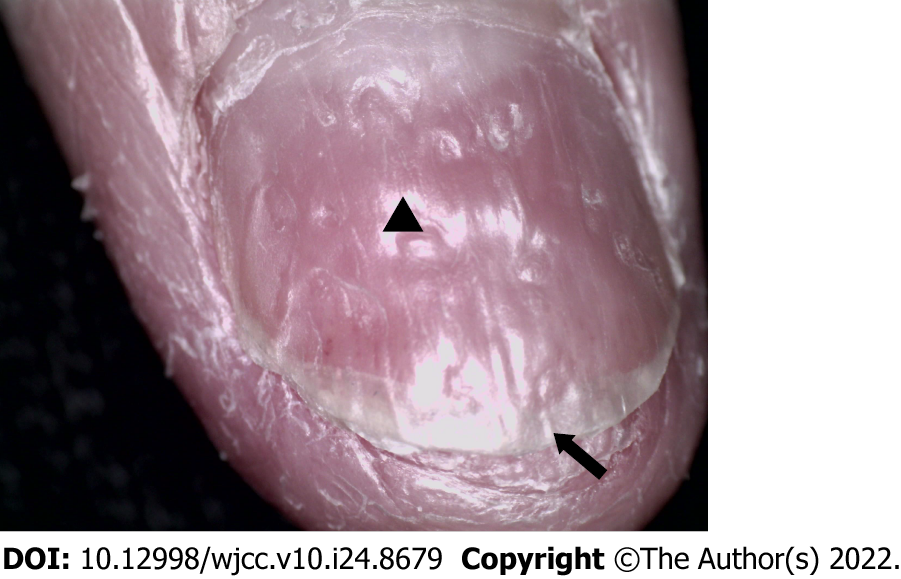
In January 2021, the patient noted asymptomatic deformation of her left middle finger nail with no obvious cause along with splitting of the distal nail plate. In April 2021, due to exposure to cherry blossom, she developed red miliary size papules on the inner aspect of right upper arm with severe itching, and was diagnosed with allergic dermatitis at a local hospital. Her symptoms improved after treatment with loratadine and topical compound dexamethasone acetate cream. In May 2021, she had symptoms of hyperhidrosis followed by development of a red polygonal flat papule (size: 5 mm) with pruritus in her right lower limb. Her symptoms were not relieved after topical application of desonide cream. One week later, a similar lesion appeared on the right side of waist. In June, her symptoms were alleviated, and she had black discoloration of some lesions. In July, the patient had recurrence of pruritus on the same site with no obvious triggering factor. After scratching, the eruption on the right upper extremity and right lower extremity spread to distal sites along the longitudinal axis, which brought the patient to our department.
Her past history was unremarkable.
There was no family history of similar disease.
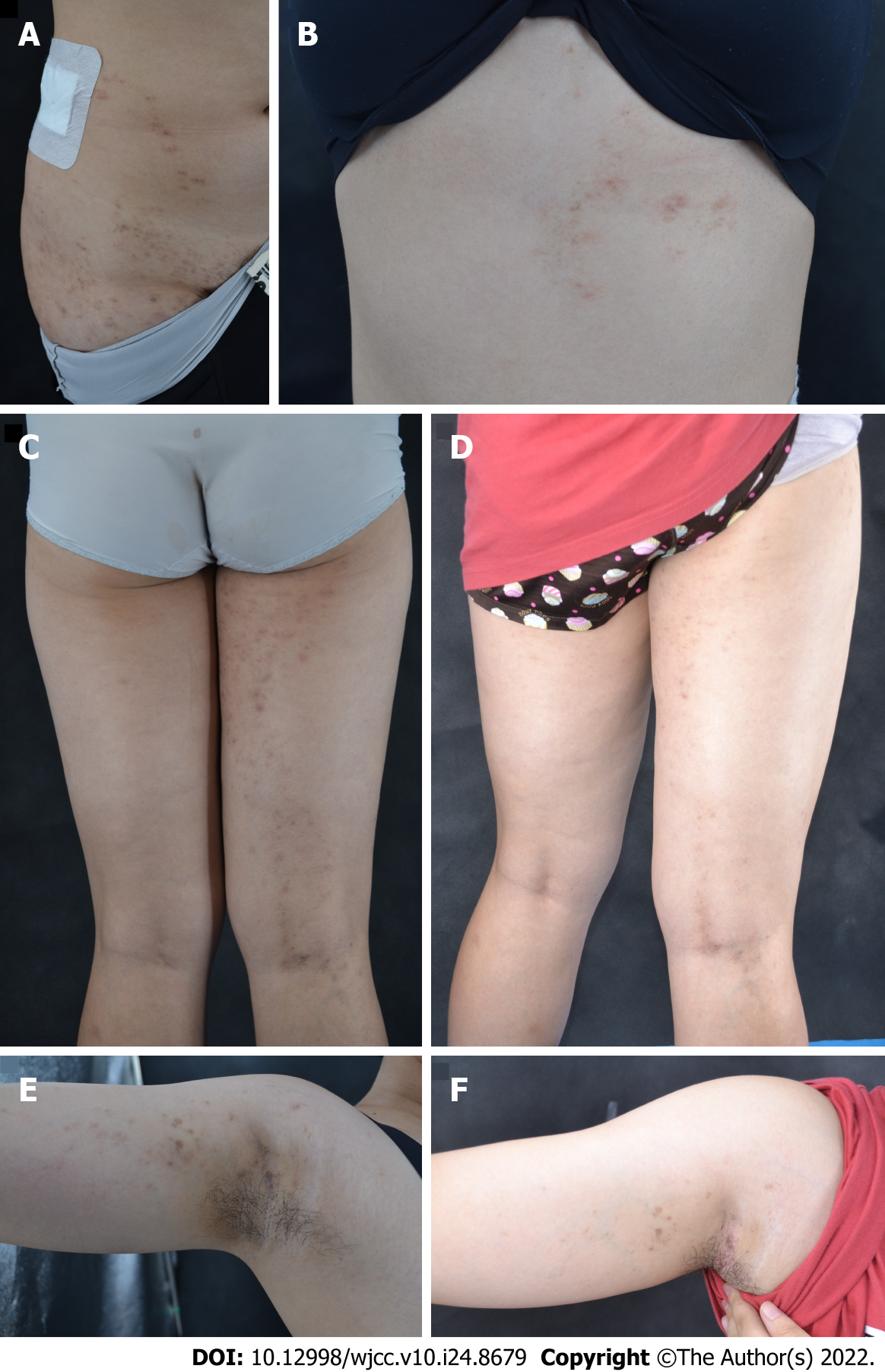
Systemic examination revealed no obvious abnormalities. Cutaneous examination showed violaceous, erythematous macules and maculopapules sized 1-5 mm on the right upper and lower limbs and on the right side of chest, back and waist. Some of the lesions had coalesced into flaky plaques with no obvious scale formation. The lesions were distributed unilaterally without crossing the midline, along the Blaschko’s lines (Figure 1A-C and E). There was no abnormality in oral mucosa. Splitting in the distal plate of the left middle finger was present and nail pit was also seen (Figure 2).
Due to the financial constraints of the patient, relevant laboratory examinations were not conducted.
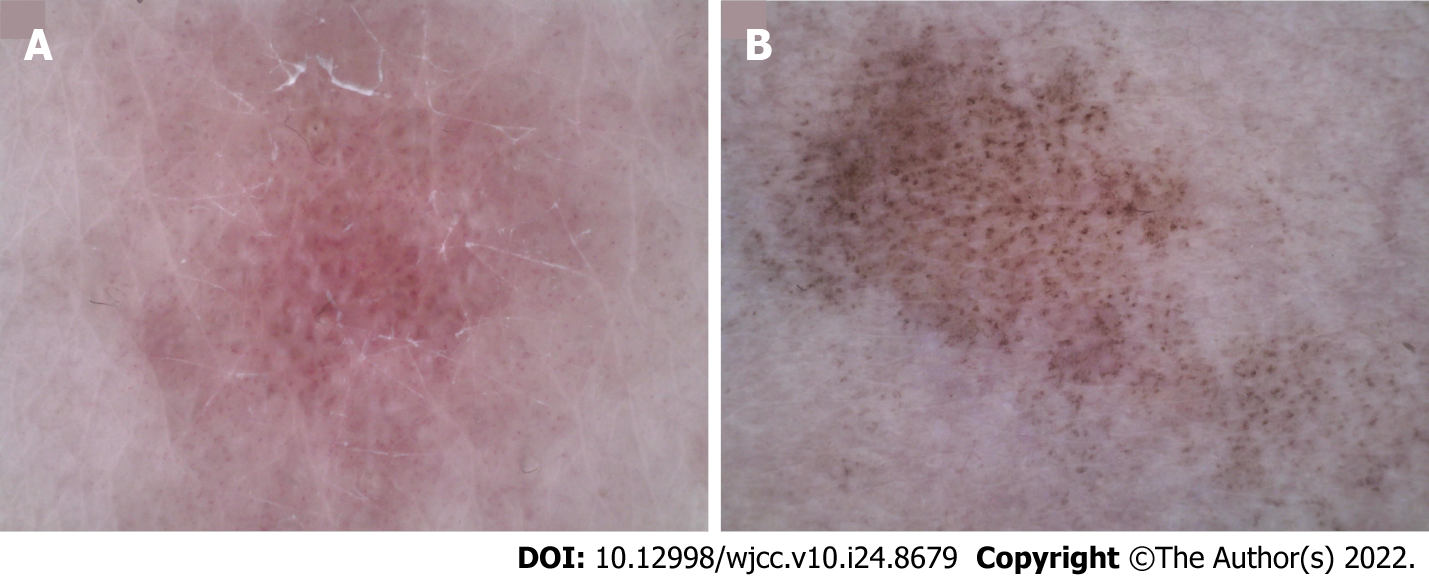
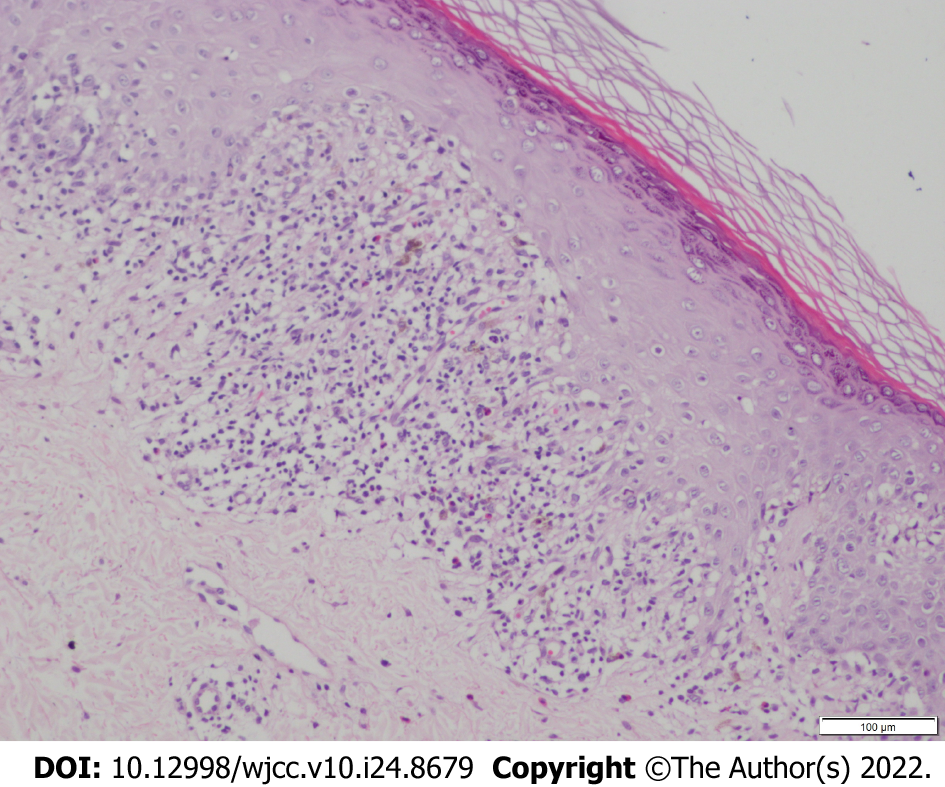
Dermoscopy examination showed linear and punctate blood vessels in the lesions. The vascular structure was radially arranged, and white reticular stripes were seen (Figure 3A). Histopathological examination showed reticular hyperkeratosis of the stratum corneum, wedge-shaped thickening of the granular layer, irregular thickening of spinous layer, basal cell vacuolization and liquefaction, compact bandlike lymphocytic infiltration in superficial dermis, and sporadic infiltration of chromatophilic cells. These were typical features of LP (Figure 4).
LP along the lines of Blaschko’s.
The patient was prescribed compound betamethasone (glucocorticoid) 5 mg by intramuscular injection; capsule acitretin 10 mg (oral) once daily; topical fluticasone propionate (glucocorticoid) cream, twice daily; and topical adapalene gel, once daily. The patient’s symptoms showed considerable improvement after 4-wk treatment with the above regime.
Follow-up examination after 4 wk revealed no new cutaneous lesion, while the old cutaneous lesions were resolved or had become pigmented patches with no pruritus (Figure 1D and F). Dermoscopy revealed disappearance of the vascular structure with residual blue-gray spots and faint white reticular stripes (Figure 3B). There was no significant improvement in nail deformation. At 16 wk, the cutaneous lesions had disappeared, but there was still no significant improvement in nail damage.
The concept of Blaschko’s lines was first proposed by Alfred Blaschko in 1901. It does not follow the distribution of blood vessels, lymph nodes, or nerves, but rather reflects the direction of spread of cell cloning and differentiation during embryonic development[3]. It is believed that LP along the Blaschko’s lines is found in 0.24%-0.62% of all LP patients[1], and nail LP affects approximately 10% of all patients with cutaneous LP[2]. In the published literature, cases of LP with unilateral distribution of lesions along the Blaschko’s lines mostly showed involvement of the trunk and limbs[1,4-6]. Our patient had extensive lesions involving the right upper and lower limb and right side of chest, back and waist.
The development of Koebner phenomenon in LP is well documented. It refers to the appearance of new skin lesions on areas of cutaneous injury or trauma in otherwise healthy skin[7,8]. In the present case, the cutaneous lesions may have resulted from allergic dermatitis or due to the spread of lesion caused by scratching. Patients with LP should be advised to avoid trauma and seek medical treatment as early as possible to avert further aggravation of symptoms.
The diagnosis of LP relies on the typical morphology of lesions at the affected site with histopathological correlation[9,10]. The histological features of LP with lesion distribution along Blaschko’s lines is identical to those of generalized LP[11]. Laboratory investigations can help rule out other systemic diseases or infectious diseases. Unfortunately, our patient did not undergo laboratory investigations due to financial constraints. The differential diagnoses in the present case included inflammatory linear verrucous epidermal nevus (ILVEN), lichen striatus, and linear porokeratosis[3]. ILVEN typically occurs in children aged < 5 years and generally involves the legs with intense pruritus. Lichen striatus predominantly occurs in children below the age of 15 years. It typically manifests as asymptomatic linear papules arranged in the form of band with slight scaling and hypopigmentation over proximal parts of limbs with spontaneous resolution in 3-6 mo[12]. Linear porokeratosis typically occurs in infants[13], and it can be type I lichen striatus or an isotopic response triggered by trauma. Differential diagnosis can be done based on the history, characteristics of cutaneous lesions, and findings of dermoscopy and histopathological examination. In addition, our case was consistent with type I nail LP, i.e., typical cutaneous lesion with nail damage[14]. After the diagnosis of LP, the diagnosis of nail LP is straightforward.
The majority of cases of cutaneous LP show spontaneous resolution within 1 or 2 years[15]. However, in a study, LP patients rated their disease on the Dermatology Life Quality Index as equivalent to that of psoriasis. The resulting decrease in the quality of life places increased emphasis on the need for effective, lasting treatments for LP[16]. The first-line treatment for cutaneous LP includes topical steroids, intralesional injection of triamcinolone acetonide, systemic corticosteroid therapy (oral or intramuscular injection), oral acitretin or isotretinoin[10,17]. Intramuscular corticosteroids show similar efficacy and improved safety in comparison to oral steroids, since the former allows for stable release of corticosteroids over a relatively long time. Intramuscular corticosteroids are considered the most reliable treatment for refractory LP with an overall success rate of 79%. Besides, topical retinoids also have a good therapeutic effect[18]. Similar cases reported previously were predominantly treated with topical steroids or oral prednisone[1,4-6]. Considering the advantages of intramuscular injection and the patient’s condition (extensive cutaneous lesions and failure of topical injection), we opted for the following treatment regime and achieved good outcome: compound betamethasone (glucocorticoid) 5 mg (intramuscular injection); oral acitretin 10 mg once daily; topical fluticasone propionate cream, twice daily; and topical adapalene gel, once daily.
Compared with the treatment of cutaneous LP, treatment of nail LP is challenging due to limited treatment options and the tendency for frequent relapse[19]. Systemic application of glucocorticoids is more effective than topical agents alone, thus systemic administration should be used as early as possible for the treatment of nail LP[2,20]. The nail condition of our patient showed no significant improvement after treatment. A previous case report described considerable improvement in nail lesions after treatment with topical methoxypsoralen and UV A for 4 mo[21]. We could not implement this treatment because of the study schedule of the patient. The patient is currently being followed up.
In summary, there is a paucity of reports on LP with lesion distribution along the Blaschko’s lines. The condition is liable to be misdiagnosed as other skin lesions with linear distribution. Few previous reports have described pre- and post-treatment clinical images and dermoscopic photographs. In this report, we present the detailed pre- and post-treatment images, which may facilitate the recognition of this condition.
LP with unilateral distribution of lesions along the Blaschko’s lines is a rare entity that needs to be differentiated from other cutaneous lesions with linear distribution. Isomorphism can occur in patients with LP, which may be an important cause for rapid spread of lesions and involvement of multiple segments. Therefore, early diagnosis and treatment are important. Our patient showed considerable improvement in skin lesions with intramuscular glucocorticoid, oral acitretin, topical glucocorticoid, and tretinoin for 4 wk, with no significant side effects. However, no improvement was observed in nail lesion. Long-term follow up is required to assess the treatment efficacy.
We thank the patient and their family members for their support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Park HK, South Korea; Vyshka G, Albania; Zhang Y, China S-Editor: Chang KL L-Editor: Kerr C P-Editor: Chang KL
| 1. | Criscito MC, Brinster NK, Skopicki DL, Seidenberg R, Cohen JM. Blaschkoid lichen planus: Throwing a “curve” in the nomenclature of linear lichen planus. JAAD Case Rep. 2020;6:237-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Solimani F, Forchhammer S, Schloegl A, Ghoreschi K, Meier K. Lichen planus - a clinical guide. J Dtsch Dermatol Ges. 2021;19:864-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (2)] |
| 3. | Yayla D, Külcü Çakmak S, Oğuz ID, Gönül M, Ozhamam E, Colak A, Gül U. Two cases of unilateral lichen planus following the lines of blaschko. Ann Dermatol. 2014;26:636-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Kapoor P, Kumar S, Batrani M. Unilateral Linear Lichen Planus Hypertrophicus Along Blaschko’s Lines. Indian Dermatol Online J. 2021;12:185-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Chuamanochan M, Onoufriadis A, Farnood S, Hsu CK, Simpson MA, Mahanupab P, Tovanabutra N, Chiewchanvit S, McGrath JA. Blaschko-linear lichen planus: Clinicopathological and genetic analysis. J Dermatol. 2020;47:e384-e385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Dayal S, Sahu P, Verma P, Amrani A, Khare R. Unilateral Blaschkoian Lichen Planus: A Series of Cases with Review of literature. J Clin Diagn Res. 2017;11:WR01-WR04. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Conforti C, Vezzoni R, Moret A, Retrosi C, Corneli P, Magaton-Rizzi G, Zalaudek I, di Meo N. Dermatoscopic features of Koebner phenomenon in lichen planus on light and dark skin. Acta Dermatovenerol Alp Pannonica Adriat. 2019;28:93-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Sagi L, Trau H. The Koebner phenomenon. Clin Dermatol. 2011;29:231-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 9. | Tziotzios C, Lee JYW, Brier T, Saito R, Hsu CK, Bhargava K, Stefanato CM, Fenton DA, McGrath JA. Lichen planus and lichenoid dermatoses: Clinical overview and molecular basis. J Am Acad Dermatol. 2018;79:789-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 115] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 10. | Ioannides D, Vakirlis E, Kemeny L, Marinovic B, Massone C, Murphy R, Nast A, Ronnevig J, Ruzicka T, Cooper SM, Trüeb RM, Pujol Vallverdú RM, Wolf R, Neumann M. European S1 guidelines on the management of lichen planus: a cooperation of the European Dermatology Forum with the European Academy of Dermatology and Venereology. J Eur Acad Dermatol Venereol. 2020;34:1403-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 11. | Kabbash C, Laude TA, Weinberg JM, Silverberg NB. Lichen planus in the lines of Blaschko. Pediatr Dermatol. 2002;19:541-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Kumavat S. Unilateral Blaschkoid Lichen Planus. Indian Dermatol Online J. 2019;10:606-607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Blue E, Abbott J, Bowen A, Cipriano SD. Linear porokeratosis with bone abnormalities treated with compounded topical 2% cholesterol/2% lovastatin ointment. Pediatr Dermatol. 2021;38:242-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Yokozeki H, Niiyama S, Nishioka K. Twenty-nail dystrophy (trachyonychia) caused by lichen planus in a patient with gold allergy. Br J Dermatol. 2005;152:1087-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Beck PB, Goksel M, Kraleti S. Eruptive Lichen Planus Associated With Chronic Hepatitis C Infection Presenting as a Diffuse, Pruritic Rash. Cureus. 2020;12:e9732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Hunt KM, Klager S, Kwak YJ, Sami N. Successful systemic treatment outcomes of lichen planus: A single-center retrospective review. Dermatol Ther. 2021;34:e14903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Böer-Auer A, Lütgerath C. [Lichen planus: fundamentals, clinical variants, histological features, and differential diagnosis]. Hautarzt. 2020;71:1007-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Husein-ElAhmed H, Gieler U, Steinhoff M. Lichen planus: a comprehensive evidence-based analysis of medical treatment. J Eur Acad Dermatol Venereol. 2019;33:1847-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Gupta MK, Lipner SR. Review of Nail Lichen Planus: Epidemiology, Pathogenesis, Diagnosis, and Treatment. Dermatol Clin. 2021;39:221-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 20. | Wechsuruk P, Bunyaratavej S, Kiratiwongwan R, Suphatsathienkul P, Wongdama S, Leeyaphan C. Clinical features and treatment outcomes of nail lichen planus: A retrospective study. JAAD Case Rep. 2021;17:43-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Pita da Veiga G, Pérez-Feal P, Moreiras-Arias N, Peteiro-García C, Suárez-Peñaranda JM, Vázquez-Veiga H, Rodríguez-Granados MT. Treatment of nail lichen planus with localized bath-PUVA. Photodermatol Photoimmunol Photomed. 2020;36:241-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |