Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8662
Peer-review started: March 2, 2022
First decision: April 19, 2022
Revised: June 6, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: August 26, 2022
Processing time: 166 Days and 23.2 Hours
Giant cell tumor (GCT) of the anterior rib origin is extremely rare. We report the first case of trauma-induced GCT of the rib.
A 22-year-old female developed a mass over the right anterior chest wall with pain 3 mo after a falling injury with blunt trauma of the right chest wall. Chest computed tomography (CT) showed a tumor originating from the right 6th rib with bony destruction, and a CT-guided needle biopsy revealed a GCT. We completely resected the tumor with chest wall and performed reconstruction. The pathological diagnosis was GCT of the bone. Twelve months after surgery, no signs of recurrence were observed.
GCT of the rib after trauma has not been reported. Meticulous history-taking and image evaluation are essential for the differential diagnosis of unusual chest wall tumors.
Core Tip: We report the first case of trauma-induced giant cell tumor of the anterior rib.
- Citation: Chen YS, Kao HW, Huang HY, Huang TW. Traumatic giant cell tumor of rib: A case report. World J Clin Cases 2022; 10(24): 8662-8666
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8662.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8662
Giant cell tumor (GCT) of the bone accounts for approximately 3%-5% of all primary bone tumors. Occurrence in the ribs, especially the anterior rib, is extremely rare[1]. GCT is generally a benign tumor; however, it can progress locally, underscoring the need for a long-term resolution. Risk factors are generally unknown, although Paget disease and Noonan syndrome as risk factors have been reported[2,3]. GCT of the rib after trauma has not been reported. Herein, we report the first case of trauma-induced rib GCT with rapid progression in a young female patient. We aim to raise awareness among clinicians about this pathology and possible risk factor of GCT.
A 22-year-old woman, complaining of right chest pain that had persisted for about 3 mo, was referred from the thoracic surgery clinic to the inpatient department.
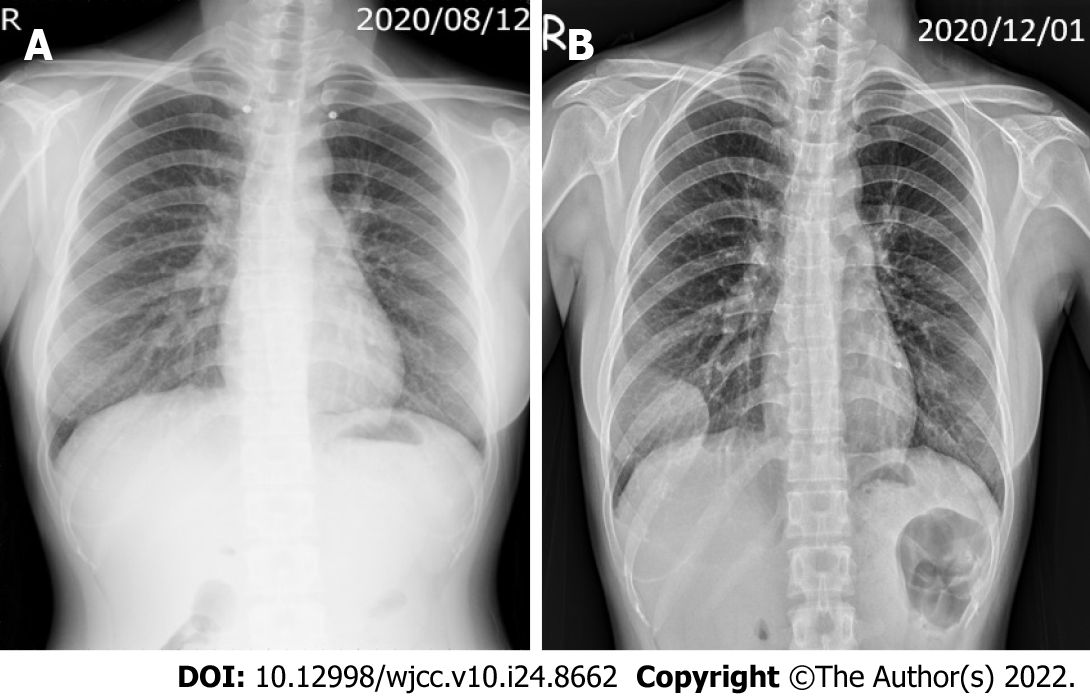
A 22-year-old female patient complained of right chest pain, which began after a fall injury (3 mo before admission). Chest radiography after the trauma showed no remarkable abnormality (Figure 1A). Despite appropriate analgesia, no sufficient pain relief had been achieved.
The patient had no significant prior medical history.
The patient had no relevant personal or family history.
A palpable mass was detected over the inframammary line. The mass was 5 cm in size, hard in consistency, tender, and adherent to profound planes (unmovable).
Findings from laboratory examinations were unremarkable.
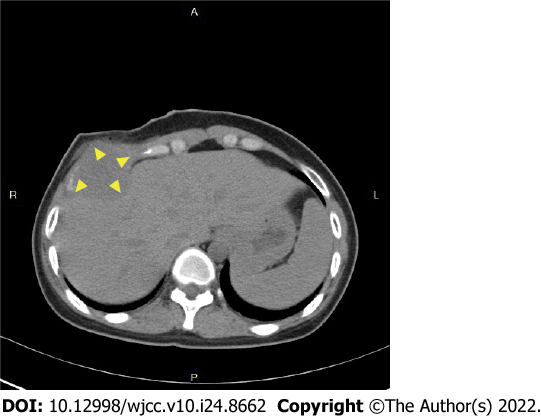
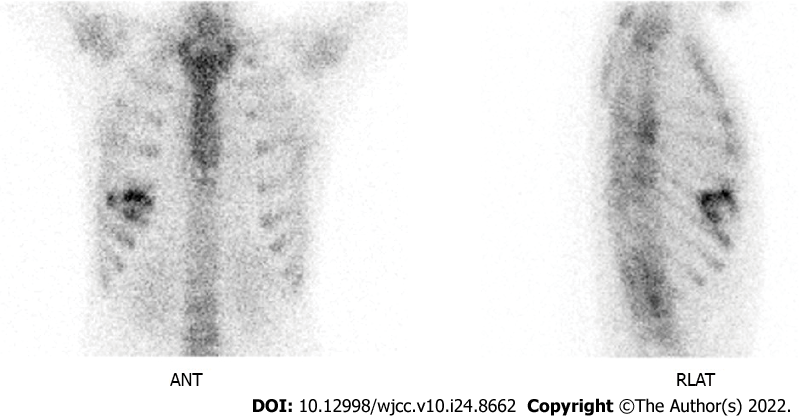
Chest radiography revealed an opacity in the right lower chest wall, with bony destruction (Figure 1B). Computed tomography (CT) indicated a 5-cm tumor in the right anterior chest wall, with destruction of the right 6th rib (Figure 2). Whole-body bone scan revealed increased uptake in the 5th-7th ribs (Figure 3).
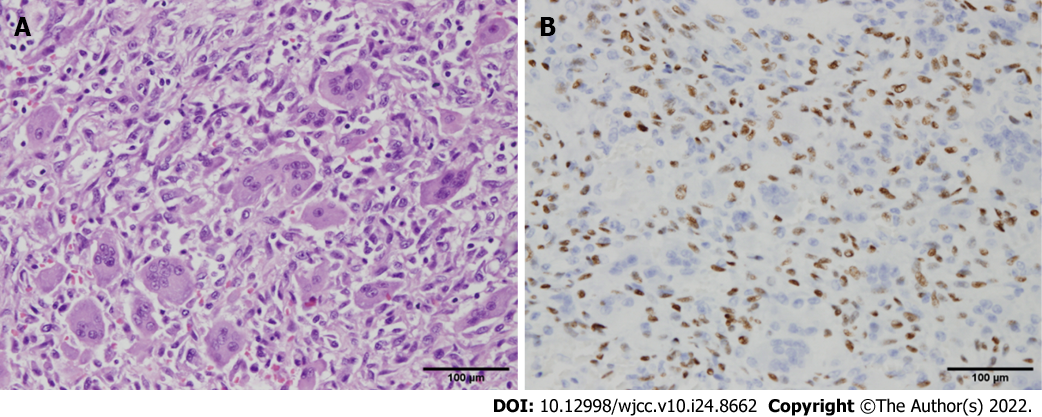
Histopathology indicated scattered multinucleated giant cells, intermixed with hypercellular spindle to ovoid tumor cells with moderate pleomorphism and extension to the skeletal muscle and bone tissue (Figure 4), consistent with a GCT.
The patient underwent surgery with excision of the chest wall tumor. Grossly, the tumor was located at the 6th rib without invasion to the adjacent structure. The tumor was a soft mass lesion, intermingled with a yellow and black area of 5.5 cm3 × 5.5 cm3 × 5 cm3 in size (Figure 5). The tumor was excised from the 5th-7th ribs, with a free margin. The defect was reconstructed primarily.
The surgery was successful, without complications. No signs of recurrence were observed at the 12-mo follow-up.
GCT of the bone is a benign but locally aggressive tumor. The meta-epiphyses of the long bones are most affected. Moreover, the most common locations, in decreasing order, are the distal femur, proximal tibia, distal radius, and sacrum[4]. This type of tumor rarely involves the ribs, accounting for only 1% of all cases reported. When located in the rib, most tumors involve the posterior arc of the rib, having an epiphyseal location[5]. Although the histogenesis and pathogenesis of GCT remain incompletely clarified, mononuclear stromal cells are believed to be the neoplastic component of GCT. These cells produce substances that can prevent or regulate osteoclastogenesis, including osteoprotegerin ligands, which function as a secreted natural negative regulator of the receptor activator of nuclear factor-kappa B[6].
For the case presented herein, GCT developed in 3 mo in the anterior ribs following trauma. Although no fracture or bony destruction was initially detected, we assume that the physical damage had induced the stromal cells to produce certain substances. Of note, few cases in the literature have a trauma history. In one such case, GCT developed in the distal ulna 1 year after a scaphoid fracture[7]. Another case had GCT located in the first metacarpal bone following a traumatic event[8]. In the present case, rapid progression with pain symptom mimicked bony malignancy.
The therapeutic strategy for GCT in most patients with potentially completely resectable tumors is surgery. Although GCT of the anterior ribs is rare, the location is relatively excisable, potentially increasing the rate of complete resection which will result in a favorable prognosis. Preoperative tissue evidence from needle biopsy may be helpful but is optional, as surgical resection is indicated regardless of whether the tumor is malignant. Intra-operative pathological consultation may be sufficient to guide the surgical management of each case.
Traumatic GCT of the ribs is rare. The manifestation of GCT mimics a malignant bone tumor. Differential diagnoses include metastasis to bone, chondroblastoma, clear cell chondrosarcoma, aneurysmal bone cysts, and lymphoma. Meticulous history-taking, image evaluation, and histological confirmation are essential for the differential diagnosis of unusual chest wall tumors.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Isac S, Romania; Malekzadegan A, Iran S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Dehghan A, Moaddab AH, Eskandarlou M, Moeeni A. Anterior chest wall giant cell tumor. Gen Thorac Cardiovasc Surg. 2010;58:39-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Cosso R. Giant cell tumor in a case of Paget's disease of bone: an aggressive benign tumor exhibiting a quick response to an innovative therapeutic agent. Clinical cases in mineral and bone metabolism: the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases 2010. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Bufalino A, Carrera M, Carlos R, Coletta RD. Giant cell lesions in noonan syndrome: case report and review of the literature. Head Neck Pathol. 2010;4:174-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Sobti A, Agrawal P, Agarwala S, Agarwal M. Giant Cell Tumor of Bone - An Overview. Arch Bone Jt Surg. 2016;4:2-9. [PubMed] |
| 5. | Heo W, Kang DK, Min HK, Jun HJ, Hwang YH. Giant cell tumor arising from anterior arc of the rib. Korean J Thorac Cardiovasc Surg. 2013;46:377-379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Salerno M, Avnet S, Alberghini M, Giunti A, Baldini N. Histogenetic characterization of giant cell tumor of bone. Clin Orthop Relat Res. 2008;466:2081-2091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Langer F. Giant cell tumor associated with trauma. Clin Orthop Relat Res. 1982;164:245-248. [DOI] [Full Text] |
| 8. | Al-Kindi H, George M, Malhotra G, Al-Muzahmi K. An uncommon presentation of giant cell tumor. Oman Med J. 2011;26:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |