Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8482
Peer-review started: March 23, 2022
First decision: April 13, 2022
Revised: April 27, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 26, 2022
Processing time: 145 Days and 4.7 Hours
There is a clear clinical need for efficient physiotherapy and rehabilitation programs during and after bone lengthening and reconstruction for gaining the optimal effect and also prevention or treatment of lengthening side effects. Pin tract infection is the most prevalent side effect during lengthening which could be prevented and treated initially via proper wound care. Muscle contractures are typically a consequence of the generated tension on the distracted muscle. It can be managed by physiotherapy initially and surgically in later severe stages. Furthermore, it is essential to avoid muscle contracture development, which is the demonstration of the imbalanced muscle appeals on the joint to inhibit the following subluxation. The knee is the furthermost affected joint by the aforementioned problem due to the inherent lack of ligamentous and bony stability. Joint stiffness is the other possible unfavorable effect of lengthening. It happens because of extensive muscle contractures or may possibly be attributed to rigidity of the joint following the amplified pressure on the joint surface during the process of lengthening. Physiotherapy and occupational therapy including endurance and strength exercise as well as stretching play an important role during the rehabilitation periods for the prevention and also the treatment of muscle contracture and the following deformity and also joint stiffness. Likewise, the effect of mental and physical rehabilitation programs should not be overlooked.
Core Tip: Difficulties that occur during limb lengthening are not avoidable. Pin tract infections are considered the most common adverse effect of lengthening which should be prevented through prophylaxis and treated as soon as possible when occurred. Muscle contractures are usually a result of the tension generated on the muscle due to distraction. It can be managed by physiotherapy initially and surgically in later severe stages. Subluxation or dislocation during lengthening may have been attributed to the preexisting joint instability or imbalanced muscle tension that developed during lengthening. It often happens in the knee joint posteriorly.
- Citation: Salimi M, Sarallah R, Javanshir S, Mirghaderi SP, Salimi A, Khanzadeh S. Complication of lengthening and the role of post-operative care, physical and psychological rehabilitation among fibula hemimelia. World J Clin Cases 2022; 10(24): 8482-8489
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8482.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8482
Fibular hemimelia (FH) is considered the most common long bones deficiency and includes an extensive spectrum of anomalies, from a slight partial fibular shortening to a whole lack of fibula, and associated defects of the foot, and ankle, tibia, femur, and even hand abnormality[1].
With respect to the numerous deformities among fibular insufficiency as well as its relationship with postaxial hypoplasia, decision-making and strategies of treatment must be personalized[2]. Treatment choices consist of non-surgical management with shoe lift and orthotic devices; limb preservation, which includes limb elongation strategies; or amputation followed by lifetime prosthetic use. The aforementioned recommended managements are principally hooked on the harshness of the amount of limb length discrepancy, the foot deformity and deficiency, and the potential for achieving the functional and plantigrade foot[3]. The optimal treatment of FH has been controversial for a long time. Amputation along with prosthetic fitting has been recommended as an effective method in the management of FH in early studies and they also use to believe that patients may be more satisfied with amputation and prosthesis with no need for multiple surgeries to correct the deformities and then lengthen the usual major limb length discrepancies[4].
Unfavorable side effects have inundated limb-lengthening procedures since the first introduction for lengthening of the lower limb in 1905[5]. High obstacle rates, mostly bone-healing related, turn into the hallmark of the conservatively accepted aforementioned technique[6]. Along with the introduction of physiological-based approaches to elongation established by Ilizarov[7] in 1988 and according to the biology and physiology of soft tissue as well as bone regeneration under the tension and stretching condition, bone healing problems and complications have developed substantially less and the treatment goals are mostly achieved[8].
It did not take long before the great revolution of Ilizarov's principles of external fixation, became the main pillar of reconstruction and lengthening. This improved the results of limb preservation and reconstruction presenting an attractive alternative to amputation[9]. Over time and as surgeons become more interested in limb preservation, lengthening, and reconstruction, several studies have been conducted on the effects of post-operative care and rehabilitation on the final outcome of reconstructive surgical approaches[10,11]. Since the Ilizarov technique is slow and gradual through daily physiologic changes in the soft tissues and bone, many potential difficulties develop during the distraction as well as fixation periods. Some of the aforementioned difficulties could be solved during the lengthening procedure[6]. In this perusal, we reviewed the literature to find the current post-operative care and rehabilitation programs during and after limb lengthening and reconstruction.
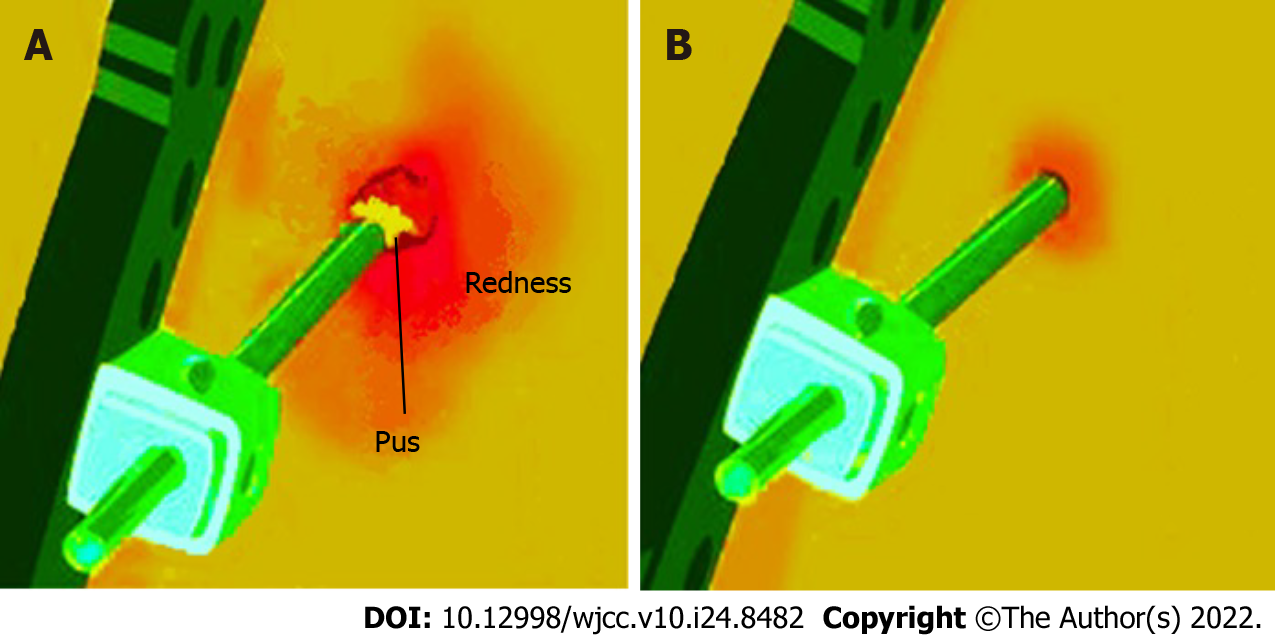
Pin tract infections are considered the most common adverse effect of lengthening or even an almost inevitable obstacle in using external apparatus with various rates of 5% to 100% which is the result of pin tract insertion[12,13] (Figure 1). It happens because the natural barrier, the skin, and residues open, providing a communication, vehiculated through the pins, between the bone and the surroundings. It can ultimately cause osteomyelitis, loosening, and fixation loss[14]. Moreover, rehabilitation may lead to motion at the pin-skin interface, aggregating the risk for pin tract infection[15].
Treatment and prophylaxis of pin track infection are influenced by different parameters[14]. Pins and holes care includes gentle softening and massage of the crust by moistening it with saline, following the use of alcohol, and the application of an antiseptic which usually consists of chlorhexidine or povidone-iodine[16,17]. Some other authors have also used tribromophenate, paraffin ointment, bismuth, silver sulfadiazine, polyhexamethylene biguanide, or hydrogen peroxide[18-21]. Protection with dry gauze finalizes the care[14]. Dry nailing makes the environment of the pining site unfavorable for germs to grow. The frequency of the aforementioned care is usually every two days, even though it varies between once a week and twice a day[14].
It has been suggested that the prophylactic prudence including the release of the skin tension at the pin-site as well as cautious pin-site overhaul and care by the parents will help in the prevention and control of the infections and their development to a complication[3,22-26]. Likewise, including the knee in the Ilizarov frame prevent moving the proximal ring to the cutaneous or subcutaneous tissue of the posterior thigh or popliteal fossa and further wound infections[27].
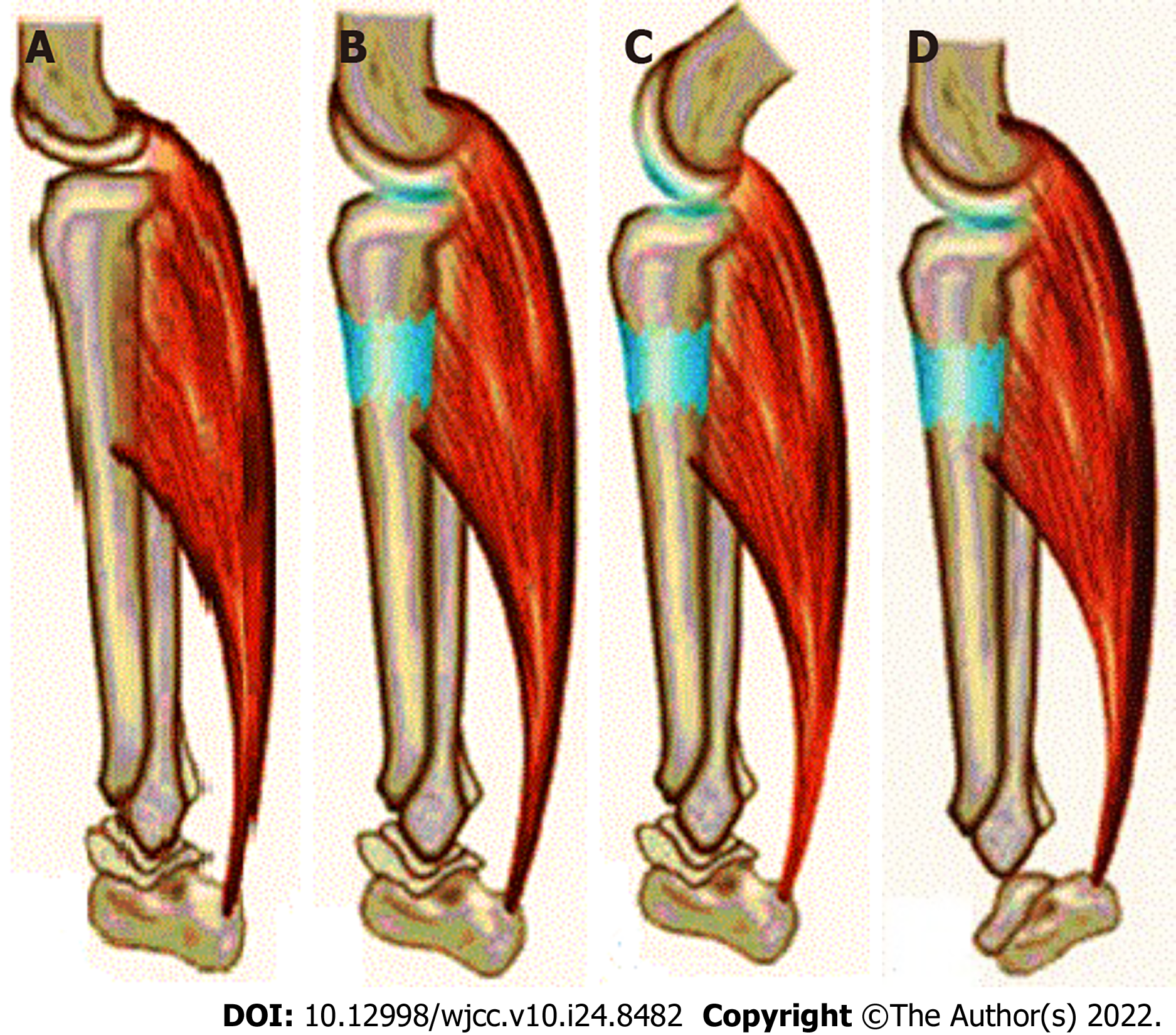
Muscle contracture is frequently a consequence of the over tension on the muscle following distraction[28]. They often have a tendency to happen in the over-powering muscle group. It goes back to the strength difference between extensors and flexors[29]. Knee flexion and ankle plantarflexion contracture during the lengthening of the tibia, the most common site of lengthening among fibula hemimelia, occurs because of the triceps surae muscle’s resistance to lengthening because of their large muscle mass and strength[30]. In some cases, who have a simultaneous proximal focal deficiency, which is accompanied by fibular hemimelia in 50% to 80%, the second stage of lengthening from femoral bone is desirable[31]. In these cases, the hamstrings are the bulkiest and largest muscle group. The hamstring contracture leads to the moving back of the leg (hip extension) and the knee to bend (knee flexion)[32].
The muscles that cross two joints are frequently involved in contractures because they contain fibers of numerous extents as opposed to muscles crossing a single joint and have fibers of the same extent[33] (Figure 2). The aforementioned statement would cause tension deviations in similar muscles. Muscle tension is a mechanism of stimulating regeneration in muscle during the lengthening procedure. Muscles that pass through two joints may contain a variance proportion of histogenesis in comparison to muscles crossing a single joint[34]. Moreover, it may be attributed to the differences in the maximum histogenesis rate and potential between bone and muscle[35].
The other etiologic concern is the muscles or tendons' transfixion by the pins of the apparatus[36]. It would be amplified via transfixed pins, the longitudinal clump of numerous pins in the single plane as well as the thick pins’ diameter. Transfixed fascia and tendons lead to joint motion restriction more than transfixed muscles[36].
Therefore, muscle contracture prevention is an inevitable portion of the elongation process. The initial preventive methods include fixation across joints, splinting, and physiotherapy[37]. Physiotherapy has been expected to motivate passive stretching movements for the most involved muscles. Moreover, it is not enough to stretch the muscle only at one end, due to the fact the aforementioned muscle typically crosses two joints. For instance, regarding the triceps surae, while the knee is flexed, the foot should be motivated to dorsiflex maximally. Afterward, the knee would be extended passively, as the ankle is dorsiflexed[38,39]. The patient must be instructed and motivated to repeat the aforementioned movements during the day[40]. Electrical stimulation, as well as active exercises, are approved to improve muscle regeneration[41]. There are several reports which have shown the positive role of continuous passive motions (CPM). Many studies have demonstrated the encouraging effect of passive motion in improving the knee flexion contracture[42,43]. CPM has also some proven hopeful effects in plantar flexion contracture of the ankle which is frequently seen following tibia lengthening[44].
The principles of contracture prevention would work if they have been maintained for at least six hours each day. It is far from the mind that most cases would exercise their muscles that much[45,46].
Trigger point dry needling is suggestive management that would reduce the pain during the physiotherapy and stretching process. This hypothesis has been supported by several investigations demonstrating that muscle damage identified by magnetic resonance imaging after the application of dry needling over the spasmed muscle was associated with post-needling induced pain[42]. They have associated the presence of post-needling with the number of local twitch responses elicited during the needling therapy. Moreover, Gattie et al[47] conducted an interesting meta-analysis that displayed low to moderate evidence suggesting that dry needling, when applied by physical therapists, is superior to each treatment solely. This may reduce the pain and so fascinate the stretching progression.
Dislocation or subluxation of the adjacent joint frequently occurs during lengthening[48]. It may have been attributed to the preexisting joint instability. For example, the anterior cruciate ligament deficiency almost always occurs in the fibula hemimelia state due to femoral notch narrowing[49,50]. The imbalanced muscle pressure that developed during elongation might conduce subluxation, even in the lack of preoperative instability; this particularly happens in the knee[51,52]. Therefore, it is fundamental to avoid muscle contracture presentation.
The knee is the most frequently affected joint because of the inherent deficiency of bony and ligamentous stability[28]. It also should be mentioned that if there is a body segment with a hypomobility (deficit of movement), the nearest segment (joint) will assume that deficit creates hypermobility (increased movement, and therefore the possibility of subluxation) thus creating a compensatory mechanism automatically and involuntarily by the patient.
The subluxated joint may be improved using stretching physiotherapy of the distorting muscle force. It is worth mentioning that physiotherapy would help in the early stages and among milder cases. Traction is another way of management[53]. For the cases of complete dislocation as well as the more severe and persistent subluxation, the apparatus should be extended across the joint to distract and then relocate it gradually or immediately. Moreover, tendon or capsular releases or reapplication of the Ilizarov may be needed[54].
Joint rigidity is usually known as a late-onset complication[55]. This happens because of long-term muscle contractures or can be attributed to rigidity of the joint following the amplified pressure on the joint surface during the elongation process[56]. If a joint is being assumed at the risk of residual rigidity while the elongation device was still on, it should be extended across the joint, and the joint can be distracted afterward. Following that the device can be used to mobilize the joint prior to its removal[57]. The severity of adverse effects can be different according to the created functional limitation. Apparently, 15° loss of ankle dorsiflexion or knee extension is much more significant in comparison to the same motion limitation in ankle plantar flexion and knee flexion[58].
Many experienced pediatric orthopaedics have stated that quality of life will increase as the child grows up[22,59]. The higher quality of life in adults may be attributed to psychological reasons and musculoskeletal development[60]. To describe more precisely, children and their parents are generally under the impression that surgery will make their appearance, daily function, and other physical aspects normal and like healthy individuals[61]. They sometimes confuse this defect with a simple bone fracture and expect it to be completely repaired with surgery. But as these patients age, they will become more realistic about their malformation and learn to adjust their lives to their disease[22]. Therefore, more involved in routine daily activity and report a higher quality of life when being surveyed. Through much literature review, we have come to the conclusion that educating parents about the fact that FH has a range of problems and that the patients who choose any management method will never be as skeletal as their peers are ultimately effective in their satisfaction[61].
Limb salvage and lengthening is a speedily growing approach to orthopaedic surgery among bone deficient cases. There are some unavoidable adverse effects. Pin Tract Infection could be extensively prevented via post-operative wound care and cleaning. Muscle contracture could be prevented and managed by physiotherapy in the early stages and surgically in later severe stages. Subluxation/ dislocation would be treated by stretching the deforming muscle force during the physiotherapy procedure. Moreover, if a joint is being assumed at the risk of residual rigidity while the elongation device was still on, it should be extended across the joint, and the joint can be distracted afterward. Following that the device can be used to mobilize the joint prior to its removal. Therefore, the aforementioned issues during or after lengthening could be prevented extensively through proper physiotherapy and occupational therapy including endurance and strength exercise as well as stretching programs. Psychological Rehabilitation would also improve the long-term quality of life and patients' satisfaction.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H, South Korea; Velázquez-Saornil J, Spain S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Hootnick DR, Vargesson N. The syndrome of proximal femur, fibula, and midline metatarsal long bone deficiencies. Birth Defects Res. 2018;110:1188-1193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Fraga CEC, Souza GJF, Martins JS, Souto MVML, Pinto RA de CC, Chaves TRT. The SUPERankle procedure in the treatment of foot and ankle deformities in fibular hemimelia. J Foot Ankle. 2021;15:217-222. [DOI] [Full Text] |
| 3. | McCarthy JJ, Glancy GL, Chnag FM, Eilert RE. Fibular hemimelia: comparison of outcome measurments after amputation and lengthening. J Bone Joint Surg Am. 2000;82:1732-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Fuller CB, Shannon CE, Paley D. Lengthening Reconstruction Surgery for Fibular Hemimelia: A Review. Children (Basel). 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Codivilla A. On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. 1904. Clin Orthop Relat Res. 1994;4-9. [PubMed] [DOI] [Full Text] |
| 6. | Hosny GA. Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol. 2020;21:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 93] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 7. | Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst. 1988;48:1-11. [PubMed] |
| 8. | Krajbich JI, Pinzuir MS, Potter BK, Stevens PM. Atlas of Amputations & Limb Deficiencies. 4thed. United States: American Academy of Orthopaedic Surgeons, 2018.. |
| 9. | Paley D. The Ilizarov technology revolution: History of the discovery, dissemination, and technology transfer of the Ilizarov method. J Limb Lengthen Reconstr. 2018;4:115-128. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Sharafat Vaziri A, Aghaghazvini L, Jahangiri S, Tahami M, Borazjani R, Tahmasebi MN, Rabie H, Mamaghani HJ, Vosoughi F, Salimi M. Determination of Normal Reference Values for Meniscal Extrusion Using Ultrasonography During the Different Range of Motion: A Pilot, Feasibility Study. J Ultrasound Med. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Hajivandi S, Dachek A, Salimi A, Mamaghani HJ, Mirghaderi SP, Dehghani J, Borazjani R, Babaniamansour A, Sarallah R, Javanshir S, Salimi M. Comparison of the Separate and Combined Effects of Physiotherapy Treatment and Corticosteroid Injection on the Range of Motion and Pain in Nontraumatic Rotator Cuff Tear: A Randomized Controlled Trial. Adv Orthop. 2021;2021:6789453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Rogers LC, Bevilacqua NJ, Frykberg RG, Armstrong DG. Predictors of postoperative complications of Ilizarov external ring fixators in the foot and ankle. J Foot Ankle Surg. 2007;46:372-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Ceroni D, Grumetz C, Desvachez O, Pusateri S, Dunand P, Samara E. From prevention of pin-tract infection to treatment of osteomyelitis during paediatric external fixation. J Child Orthop. 2016;10:605-612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Guerado E, Cano JR, Fernandez-Sanchez F. Pin tract infection prophylaxis and treatment. Injury. 2019;50 Suppl 1:S45-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Quattlebaum DG, Loker KM, Stoneback IW. External Fixation in Orthopaedic Trauma and Limb Reconstruction. JBJS J Orthop Physician Assist. 2021;9:e21.00013. [DOI] [Full Text] |
| 16. | Patterson MM. Multicenter pin care study. Orthop Nurs. 2005;24:349-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | W-Dahl A, Toksvig-Larsen S, Lindstrand A. No difference between daily and weekly pin site care: a randomized study of 50 patients with external fixation. Acta Orthop Scand. 2003;74:704-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Grant S, Kerr D, Wallis M, Pitchford D. Comparison of povidone-iodine solution and soft white paraffin ointment in the management of skeletal pin-sites: A pilot study. J Orthop Nur. 2005;9:218-225. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 19. | Egol KA, Paksima N, Puopolo S, Klugman J, Hiebert R, Koval KJ. Treatment of external fixation pins about the wrist: a prospective, randomized trial. J Bone Joint Surg Am. 2006;88:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Yuenyongviwat V, Tangtrakulwanich B. Prevalence of pin-site infection: the comparison between silver sulfadiazine and dry dressing among open tibial fracture patients. J Med Assoc Thai. 2011;94:566-569. [PubMed] |
| 21. | Lee CK, Chua YP, Saw A. Antimicrobial gauze as a dressing reduces pin site infection: a randomized controlled trial. Clin Orthop Relat Res. 2012;470:610-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Birch JG, Paley D, Herzenberg JE, Morton A, Ward S, Riddle R, Specht S, Cummings D, Tulchin-Francis K. Amputation Versus Staged Reconstruction for Severe Fibular Hemimelia: Assessment of Psychosocial and Quality-of-Life Status and Physical Functioning in Childhood. JB JS Open Access. 2019;4:e0053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Choi IH, Kumar SJ, Bowen JR. Amputation or limb-lengthening for partial or total absence of the fibula. J Bone Joint Surg Am. 1990;72:1391-1399. [PubMed] [DOI] [Full Text] |
| 24. | Naudie D, Hamdy RC, Fassier F, Morin B, Duhaime M. Management of fibular hemimelia: amputation or limb lengthening. J Bone Joint Surg Br. 1997;79:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Tomás-Gil J, Valverde Belda D, Chismol-Abad J, Valverde-Mordt C. Complete fibular hemimelia: a long-term review of four cases. Acta Orthop Belg. 2002;68:265-271. [PubMed] |
| 26. | Walker JL, Knapp D, Minter C, Boakes JL, Salazar JC, Sanders JO, Lubicky JP, Drvaric DM, Davids JR. Adult outcomes following amputation or lengthening for fibular deficiency. J Bone Joint Surg Am. 2009;91:797-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Liu K, Abulaiti A, Liu Y, Cai F, Ren P, Yusufu A. Risk factors of pin tract infection during bone transport using unilateral external fixator in the treatment of bone defects. BMC Surg. 2021;21:377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Calder PR, Faimali M, Goodier WD. The role of external fixation in paediatric limb lengthening and deformity correction. Injury. 2019;50 Suppl 1:S18-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 29. | Uysal M. The Treatment of Complications in Ilizarov Technique. In: Çakmak M, Şen C, Eralp L, Balci H, Civan M. Basic Techniques for Extremity Reconstruction. Cham: Springer, 2018: 691-699. |
| 30. | Miraj F, Nugroho A, Dalitan IM, Setyarani M. The efficacy of ilizarov method for management of long tibial bone and soft tissue defect. Ann Med Surg (Lond). 2021;68:102645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Hosny GA, Bilgili F, and Balci HI. Congenital Lower Limb Deformities. In: Çakmak M, Şen C, Eralp L, Balci H, Civan M. Basic Techniques for Extremity Reconstruction. Cham: Springer, 2018: 493-539. |
| 32. | Bakhshi AS, Kumar S, Singh J, Sood M, Jain KA. Complications of ilizarov ring fixator and their management. Int J Orthop. 2019;5:839-844. [DOI] [Full Text] |
| 33. | Maas H, Finni T. Mechanical Coupling Between Muscle-Tendon Units Reduces Peak Stresses. Exerc Sport Sci Rev. 2018;46:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Carpenter C. Paediatric Disorders. In: Agarwal S. Current Orthopaedic Practice. Cham: Springer, 2022: 425-479. |
| 35. | Kong LC, Li HA, Kang QL, Li G. An update to the advances in understanding distraction histogenesis: From biological mechanisms to novel clinical applications. J Orthop Transl. 2020;25:3-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Palazzolo A, Rosso F, Bonasia DE, Saccia F, Rossi R; Knee Committee SIGASCOT. Uncommon Complications after Anterior Cruciate Ligament Reconstruction. Joints. 2018;6:188-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 37. | DePamphilis MA, Cauley RP, Sadeq F, Lydon M, Sheridan RL, Winograd JM, Driscoll DN. Reconstruction of the Upper Extremity High-Voltage Electrical Injury: A Pediatric Burn Hospital's 13-Year Experience. J Burn Care Res. 2022;43:696-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Green SA, Dahl MT. Postoperative Management Considerations. In: Green SA, Dahl MT. Intramedullary Limb Lengthening. Cham: Springer, 2018: 125-136. |
| 39. | Jahangiri S, Mousavi SH, Hatamnejad MR, Salimi M, Bazrafshan H. Prevalence of non-steroidal anti-inflammatory drugs (NSAIDs) use in patients with hypertensive crisis. Health Sci Rep. 2022;5:e483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Iliadis AD, Palloni V, Wright J, Goodier D, Calder P. Pediatric Lower Limb Lengthening Using the PRECICE Nail: Our Experience With 50 Cases. J Pediatr Orthop. 2021;41:e44-e49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 41. | Iyer KM. The Principles of the Ilizarov apparatus. In: Iyer K, Khan W. General Principles of Orthopedics and Trauma. Cham: Springer, 2019: 607-617. |
| 42. | Fernández-de-Las-Peñas C, Nijs J. Trigger point dry needling for the treatment of myofascial pain syndrome: current perspectives within a pain neuroscience paradigm. J Pain Res. 2019;12:1899-1911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 109] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 43. | Knapik DM, Harris JD, Pangrazzi G, Griesser MJ, Siston RA, Agarwal S, Flanigan DC. The basic science of continuous passive motion in promoting knee health: a systematic review of studies in a rabbit model. Arthroscopy. 2013;29:1722-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Linan E, O'Dell MW, Pierce JM. Continuous passive motion in the management of heterotopic ossification in a brain injured patient. Am J Phys Med Rehabil. 2001;80:614-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 45. | Zhai J, Weng X, Zhang B, Peng H, Bian Y. Management of knee flexion contracture in haemophilia with the Ilizarov technique. Knee. 2019;26:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Salimi M, Dehghani J, Gerami MH. Efficacy of Elastic Intramedullary Nails in Treating Axially Unstable Femur Fracture in Children. Pak J Med Health Sci. 2021;15:572-576. |
| 47. | Gattie E, Cleland JA, Snodgrass S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. J Orthop Sports Phys Ther. 2017;47:133-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 161] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 48. | Green SA, Dahl MT. Preventing Complications During Limb Lengthening. In: Green SA, Dahl MT. Intramedullary Limb Lengthening. Cham: Springer, 2018: 93-124. |
| 49. | Beran MC, Samora WP, Klingele KE, Parikh SN. Congenital Absence of the Anterior Cruciate Ligament. In: Parikh S. The Pediatric Anterior Cruciate Ligament. Cham: Springer, 2018: 241-249. |
| 50. | Akrami M, Izadpanah P, Bazrafshan M, Hatamipour U, Nouraein N, Drissi HB, Manafi A. Effects of colchicine on major adverse cardiac events in next 6-month period after acute coronary syndrome occurrence; a randomized placebo-control trial. BMC Cardiovasc Disord. 2021;21:583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 51. | Shivji F, Kurien T, Robinson K, Ali F. Lower Limb Clinical Cases. In: Ali F, Harris N. Orthopaedic Examination Techniques: A Practical Guide. Cambridge: Cambridge University Press, 2022: 300-315. |
| 52. | Leite CBG, Grangeiro PM, Munhoz DU, Giglio PN, Camanho GL, Gobbi RG. The knee in congenital femoral deficiency and its implication in limb lengthening: a systematic review. EFORT Open Rev. 2021;6:565-571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 53. | Shende G, Deshmukh MP, Jain DK, Phansopkar P. Efficacy of Stretching vs Muscle Energy Technique in Postoperative Elbow Stiffness: A Research Protocol. Indian J Forensic Med Toxicol. 2021;15:136-138. [DOI] [Full Text] |
| 54. | Fragomen AT, Falls TD, Suh J, Khabyeh-Hasbani N, Rozbruch S R. Tibial lengthening evolution: Classic ilizarov, lengthening and then nailing, motorized internal lengthening nail. J Limb Lengthen Reconstr. 2020;6:13-19. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 55. | Angelini A, Baracco R, Dolci A, Vigo M, Mavrogenis AF, Ruggieri P. Limb lengthening for deformities in Ollier's disease: a systematic review. Eur J Orthop Surg Traumatol. 2020;30:1325-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 56. | Vogt B, Gosheger G, Wirth T, Horn J, Rödl R. Leg Length Discrepancy- Treatment Indications and Strategies. Dtsch Arztebl Int. 2020;117:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 57. | Luo S, Kong L, Wang J, Nie H, Luan B, Li G. Development of modified Ilizarov hip reconstruction surgery for hip dysfunction treatment in adolescent and young adults. J Orthop Translat. 2021;27:90-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 58. | Maior AS, Lobo E, Braz M, Campos JC Jr, Leporace G. Comparison of ankle range of motion and functional performance between practitioners of resistance exercise with free-weight vs. Machine. MOJ Sports Med. 2020;4:81-85. [DOI] [Full Text] |
| 59. | Tieland M, Trouwborst I, Clark BC. Skeletal muscle performance and ageing. J Cachexia Sarcopenia Muscle. 2018;9:3-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 461] [Cited by in RCA: 509] [Article Influence: 72.7] [Reference Citation Analysis (0)] |
| 60. | Ng JS, Chin KY. Potential mechanisms linking psychological stress to bone health. Int J Med Sci. 2021;18:604-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 61. | Cox CL, Zhu L, Kaste SC, Srivastava K, Barnes L, Nathan PC, Wells RJ, Ness KK. Modifying bone mineral density, physical function, and quality of life in children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2018;65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |