Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8463
Peer-review started: March 21, 2022
First decision: June 7, 2022
Revised: June 26, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: August 26, 2022
Processing time: 147 Days and 3.7 Hours
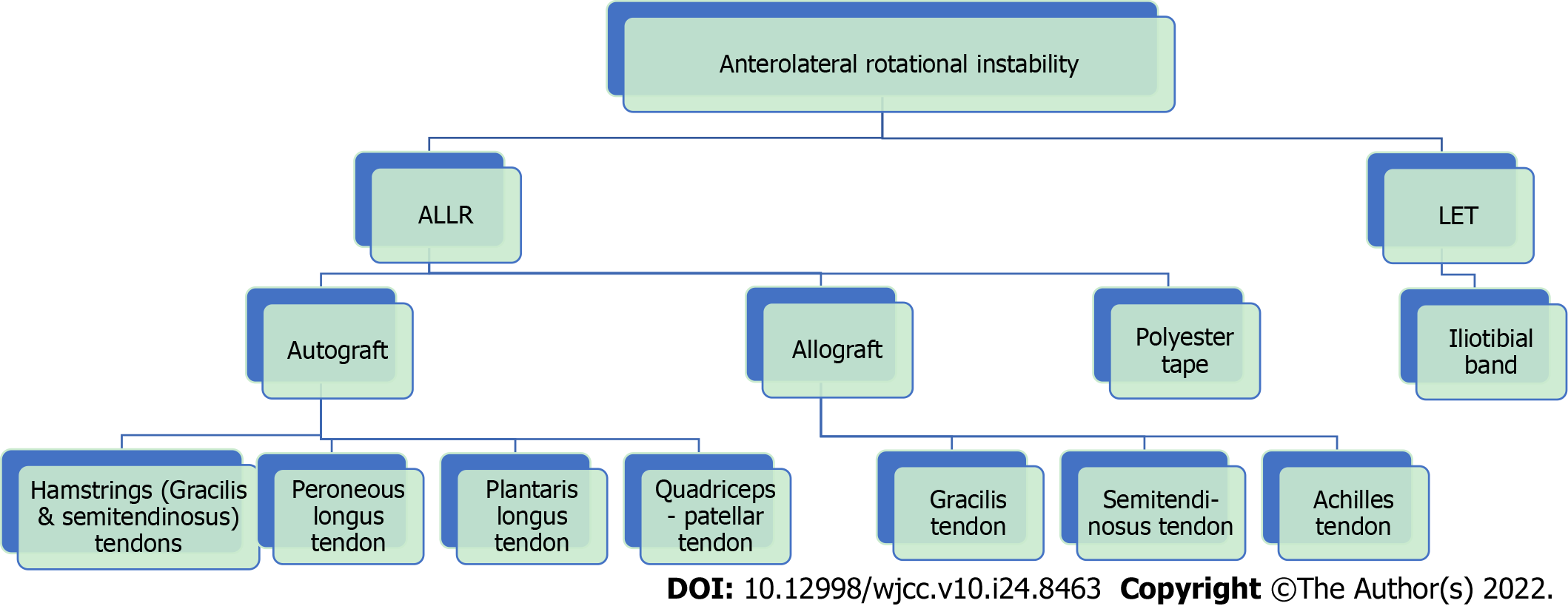
The anterolateral ligament (ALL) is a primary structure of the anterolateral complex of the knee that contributes to internal rotational stability of the joint. Injury of the ALL is commonly associated with rupture of the anterior cruciate ligament. If left untreated, ALL lesions may lead to residual anterolateral rotational instability of the knee after anterior cruciate ligament reconstruction, which is a common cause of anterior cruciate ligament graft failure. The function of the ALL can be restored by lateral extraarticular tenodesis or anterolateral ligament reconstruction (ALLR). In the lateral extraarticular tenodesis procedure, a strip of the iliotibial band is placed in a non-anatomical position to restrain the internal rotation of the tibia, while in ALLR, a free graft is fixed at the insertion points of the native ALL. Gracilis and semitendinosus grafts have mainly been utilized for ALLR, but other autografts have also been suggested. Furthermore, allografts and synthetic grafts have been applied to minimize donor-site morbidity and maximize the size and strength of the graft. Nevertheless, there has been no strong evidence to fully support one method over another thus far. The present review presents a detailed description of the graft choices for ALLR and the current literature available in regard to the effectiveness and outcomes of published surgical techniques.
Core Tip: There is no convincing evidence regarding the biomechanical and functional superiority of either lateral extraarticular tenodesis or anterolateral ligament reconstruction procedures during anterior cruciate ligament reconstruction. Although hamstrings remain the most common graft choice for anterolateral ligament reconstruction, other autografts as well as allografts and synthetic grafts have been applied. Further research and comparative studies should be carried out to identify the most effective graft material and technique for the restoration of rotational knee stability in the presence of residual instability after anterior cruciate ligament reconstruction.
- Citation: Chalidis B, Pitsilos C, Kitridis D, Givissis P. Graft choices for anterolateral ligament knee reconstruction surgery: Current concepts. World J Clin Cases 2022; 10(24): 8463-8473
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8463.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8463
The anterolateral ligament (ALL) is an independent structure of the anterolateral complex of the knee along with the lateral collateral ligament (LCL), the iliotibial band (ITB) and the anterolateral joint capsule[1,2]. There is no consensus so far on whether ALL bony attachment is located posterior and proximal or anterior and distal to the lateral femoral epicondyle or just on the lateral epicondylar together with the LCL attachment[3-7]. Its course is anterodistal and superficial to the LCL and its distal insertion midway between the anterior border of the fibular head and the Gerdy’s tubercle of the tibia[8]. The ALL is a nonisometric structure that tenses during knee flexion and internal tibial rotation and shows the greatest length change at 90° of flexion[9]. As a distinct structure of the anterolateral complex of the knee, the ALL seems to contribute to internal rotational stability of the joint, but its role in resisting rotational as well as anteroposterior instability in an anterior cruciate ligament (ACL) deficient knee is still controversial[10-13].
An ALL lesion is presented as a midsubstance strain and tear or avulsion of its bony insertion on the tibia, which is known as a Segond fracture[14]. The injury is most commonly associated with ACL rupture[5]. Concomitant ACL and ALL deficiency may result in increased knee rotational instability, which may not be restored by isolated anterior cruciate ligament reconstruction (ACLR)[15]. The incidence of positive pivot shift after ACLR could rise to 34% of operated cases, and many studies have demonstrated that additional ALL reconstruction (ALLR) decreases knee laxity and ACL graft failure rate and improves patient-reported outcomes[16-20]. On the other hand, simultaneous ALLR has been associated with overconstrained internal rotation and subsequent knee joint stiffness[21,22]. Furthermore, there is some evidence that ALLR does not decrease the rotational laxity of the knee to a desirable degree and its role in improving the postoperative function is limited[23,24]. Thus, simultaneous ACLR and ALLR have been suggested mainly in cases of grossly unstable pivot-shift and revision ACL surgery[25,26]. Moreover, indications for ALLR may include young patients who participate in pivoting activities as well as knees with chronic ACL deficiency or concomitant meniscal tears requiring surgical repair[27].
We conducted a narrative review using the MEDLINE online database regarding ALLR. The initial search applying the keywords “Anterolateral Ligament Reconstruction” led to 807 results. After abstract and full-text screening, 22 studies describing the results of ALLR in ACLR surgery were enrolled for further assessment (Figure 1). The extracted data were analyzed and organized to present the different reported methods of ALLR during ACLR in respect to graft choice, proximal and distal attachment location, stabilization technique and knee fixation angle (Table 1).
| Ref. | ACL graft type | ALL graft type | Femoral fixation point | Tibial fixation point | Fixation Technique | Knee flexion/rotation |
| Lemaire and Combelles[36], 1980 | BTB (hole for ITB graft) | ITB | Above the lateral epicondyle, proximal to the LCL insertion | Maintain attachment to Gerdy’s tubercle | Two bone tunnels, suture on itself | 30º flexion/external rotation |
| Andrews and Sanders[41], 1983 | ITB (two strips) | Lateral femoral epicondyle | Maintain attachment to Gerdy‘s tubercle | Suture strips together at medial femoral condyle after passing through two parallel lateral-to-medial tunnels | 90º flexion/external rotation | |
| Amirault et al[40], 1988 | ITB | Above the lateral epicondyle, proximal to the LCL insertion | Maintain attachment to Gerdy’s tubercle | Suture fixation to ITB after passing through the lateral intermuscular septum | 90º flexion/external rotation | |
| Christel and Djian[37], 2002 | ITB | Above the lateral epicondyle, proximal to the LCL insertion | Maintain attachment to Gerdy’s tubercle | Interference screw | 30º flexion | |
| Mathew et al[38], 2018 | ITB | Anterior and proximal to the lateral gastrocnemius tendon | Maintain attachment to Gerdy’s tubercle | Richards staple and sutures to itself | 60º flexion/neutral rotation | |
| Abusleme et al[39], 2021 | ITB | Above the lateral epicondyle, proximal to the LCL insertion | Maintain attachment to Gerdy’s tubercle | Suture fixation to ITB after passing through the lateral intermuscular septum | 30º flexion/neutral rotation | |
| Colombet[49], 2010 | Quadruple (Semitendinosus double-bundle and gracilis double-bundle) or Double (single-bundle each) | Gracilis -semitendinosus (one bundle each) | Proximal to lateral epicondyle | Gerdy’s tubercule | Absorbable screws at each fixation point | 90º flexion/neutral rotation |
| Helito et al[29], 2015 | Quadruple (semitendinosus triple-bundle and gracilis single-bundle) | Gracilis (single-bundle) | 3-4 mm below the halfway point on the Blumensaat’s line in the AP direction | 5-10 mm below the lateral tibial plateau, between fibular head and Gerdy’s tubercle | One 5 mm metal anchors at each fixation point | 60-90° of flexion/nm |
| Smith et al[45], 2015 | Semitendinosus graft | Gracilis (double-bundle) | Anterior to lateral femoral epicondyle | Midway between fibular head and the Gerdy’s tubercle, 11 mm distal to joint line | 4.75 or 5.5 mm bioabsorbable knotless suture anchor at each fixation point | 30° of flexion/neutral rotation |
| Ferreira et al[48], 2016 | Semitendinosus triple-bundle | Gracilis (double-bundle) | 8 mm posterosuperiorly from lateral epicondyle | 9-13 mm distal to lateral joint line, between fibular head and the Gerdy’s tubercle | Interference screw 2 mm larger than tunnel | 45-60° flexion/nm |
| Sonnery-Cottet et al[44], 2016 | Semitendinosus SAMBBA | Gracilis (double-bundle) | Proximal and posterior to lateral epicondyle | One superolateral margin of the Gerdy’s tubercle and one midway between fibular head and the Gerdy’s tubercle | 4.75 or 5.5 mm bioabsorbable knotless suture anchor at each fixation point | Full extension/neutral rotation |
| Delaloye et al[47], 2018 | Internal brace | Gracilis (double-bundle) | Proximal and posterior to lateral epicondyle | Bone tunnel: One point just anterior to the fibular head and second posterior to Gerdy’s tubercle | 4.75 bioabsorbable knotless suture anchor at femoral fixation point | Full extension/neutral rotation |
| Saithna et al[18], 2018 | Quadruple (Semitendinosus triple-bundle and gracilis single-bundle) | Gracilis (single-bundle) | Proximal and posterior to lateral epicondyle | Bone tunnel: One point just anterior to the fibular head and second posterior to Gerdy’s tubercle | Ethibond suture around the graft | Full extension/neutral rotation |
| Goncharov et al[46], 2019 | BTB autograft | Gracilis or semitendinosus tendon autograft | Proximal to lateral epicondyle | 10 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Interference screws | Full extension/nm |
| Kim et al[50], 2020 | Semitendinosus autograft | Proximal and posterior to lateral epicondyle | Midway between fibular head and the Gerdy’s tubercle | Interference screw at femur, adjustable length loop button at tibia | 30° flexion/neutral rotation | |
| Escudeiro de Oliveira et al[52], 2021 | Quintuple, Semitendinosus double-bundle, gracilis double-bundle and peroneous longus single-bundle | Peroneous longus | Proximal and posterior to lateral epicondyle | 15 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Interference screws | 30° flexion/nm |
| Josipovic et al[53], 2020 | Quintuple, Semitendinosus triple-bundle, plantaris longus double-bundle | Plantaris longus | Proximal and posterior to lateral epicondyle | 10 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Interference screw at tibia | Full extension/nm |
| Wagih and Elguindy[59], 2016 | Polyester tape | Distal and anterior to lateral femoral condyle | Midpoint between the Gerdy’s tubercle and the fibular head | Cortical suspension button proximally, tie on a bone bridge of two bone tunnels distally | 30° flexion/nm | |
| Lee et al[25], 2019 | Tibialis anterior tendon allograft | Gracilis tendon allograft | Proximal and posterior to lateral epicondyle | 10 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Interference screws | 30° flexion/neutral rotation |
| Chahla et al[57], 2016 | Semitendinosus allograft | 4.7 mm proximal and posterior to LCL insertion site | 9.5 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Interference screws | 30° flexion/nm | |
| Fernández et al[58], 2020 | Achilles tendon allograft | Achilles tendon allograft | Proximal and posterior to lateral epicondyle | 15 mm distal to joint line, between fibular head and the Gerdy’s tubercle | Staple at distal site | 30° flexion/neutral rotation |
| Benum[42], 1982 | Patellar tendon (lateral one-third with proximal bone block) | Femoral origin of LCL | Maintain attachment to tibial tubercle | Staple at femoral side | 45º flexion/external rotation |
So far, many grafts have been applied for the restoration of ALL function, but no consensus exists regarding the ideal graft type and fixation technique. Controversies are based on the anatomic parameters of ALL regarding its bony origin and its length changes during knee motion. They are referred to graft material choice as well as graft insertion site location and fixation angle[6,8,23,28-33]. All the applied procedures aim to restore the knee kinematics in case of ALL deficiency and include either the lateral extraarticular tenodesis (LET) or ALLR techniques. The main principle of the LET procedure is the use of a strip of ITB that is stabilized proximally above the knee joint while its tibial insertion to Gerdy’s tubercle remains intact[34]. On the other hand, the ALLR aims to restore the ALL native features by fixing a free tendon graft between the anatomical femoral and tibial insertion points of the ALL[35].
The ITB is exclusively used for the LET procedure. Lemaire[36] was the first who described the LET technique in cases of chronic ACL injuries. In the original procedure, the ITB was identified and a strip of 1 cm wide and 18 cm long was harvested, leaving the attachment to Gerdy’s tubercle intact. The graft was first passed in a distal to proximal direction under the LCL. Then, it was introduced to the distal femur through a bone tunnel above the lateral epicondyle and proximal to the LCL insertion. Consequently, it was passed again under the LCL in a proximal to distal direction and finally fixed to the tibia through a bone tunnel at Gerdy’s tubercle and sutured on itself. Fixation was completed in 30º of knee flexion and some tibial external rotation. In cases of combination with ACLR, LET allows for independent ACL graft choice. The authors also proposed a variation of the original technique by fixing the strip of ITB into the femoral tunnel that was created for bone-patellar tendon-bone graft ACLR.
Many modifications of the Lemaire procedure have been described referring to harvesting a shorter strip of tendon[37,38]. In addition, the graft may be stabilized proximally with sutures to the ITB after passing through the lateral intermuscular septum or with either a staple or an interference screw[37-40]. Andrews and Sanders[41] described a technique where two strips of ITB were harvested and passed through two parallel lateral-to-medial femoral tunnels and sutured together.
Moreover, variable knee flexion angles have been recommended during fixation, including 30º, 60º and 90º[38,39,42]. In respect to tibial rotation, older studies suggested that the tibia should be maintained in external rotation, but no specific angle was defined[40,41]. However, that position has been related to excessive restriction of internally rotatory movement and abnormal knee kinematics[34,43]. This overconstraint along with the non-anatomic nature of the LET procedure may lead to gradual elongation of the graft and subsequent recurrent rotational instability[43]. As a result, most recent studies have advocated a neutral rotation position for ITB graft fixation[38,39].
Gracilis tendon (GT) is a commonly used autograft for ALLR. The free tendon graft is fixed proximally on the lateral femoral epicondyle and distally between the fibular head and Gerdy’s tubercle after passing between the ITB and LCL[19]. Most frequently, the graft is introduced proximal and posterior to lateral femoral, but a more anterior position has also been described[44,45]. Femoral fixation can be performed with an interference screw or an anchor[45,46]. The same principles are followed when concomitant ACLR is performed with either hamstrings graft, bone-patellar tendon-bone graft or internal brace[44-47].
The tibial attachment of the graft is placed between the fibular head and Gerdy’s tubercle approximately 5 to 13 cm distal to the lateral joint line[29,48]. Fixation is accomplished using an interference screw or an anchor[29,49]. Some authors have described ALLR in an inverted V-shaped fashion. Specifically, the graft is introduced in a tibial bone tunnel extending anterior to the fibular head and posterior to Gerdy’s tubercle and then is fixed at the femoral side with an anchor or with sutures around the graft[18,47]. Sonnery-Cottet et al[44] completed tibial fixation of the graft with two suture anchors. The first one was placed on the superolateral margin of the Gerdy’s tubercle and the other one midway between the fibular head and Gerdy’s tubercle.
During combined ALLR and ACLR using hamstring tendon autograft, a single graft is usually used for both procedures. After ACLR, the remaining graft is passed through a bone tunnel to the lateral surface of the distal femur, proximally and posteriorly to the lateral epicondyle[18,48]. Helito et al[29] identified the ALLR femoral tunnel location using fluoroscopy, aiming approximately 3-4 mm below the halfway point of the Blumensaat’s line in the anteroposterior direction. Furthermore, Ferreira et al[48] used a triple semitendinosus tendon (ST) graft for ACLR and a double GT graft for ALLR. Another combination is a four-strand ACL graft formed by a triple ST bundle and a single GT bundle, while the remaining GT is used for ALLR[29]. Colombet[49] also described the use of a quadruple ACL graft composed of two ST and two GT bundles. A double-bundle graft for ALLR was created from the excess tendon tissue of the bundles.
There is no consensus regarding the ideal fixation angle of a GT graft. Several different knee angles have been reported so far including full extension, 30º, 45º to 60º,60º to 90º and 90º[29,45,47-49]. In contrast, it has been generally accepted that the tibia should be maintained in neutral rotation at the time of graft stabilization[18,44,45].
Apart from GT, the ST has been also widely used for ALLR[46]. Kim et al[50] harvested the contralateral ST for ALLR, as the ipsilateral ST had been already used for ACLR during the same or previous procedure. The double-bundle graft was first attached on the tibia (midway between the fibular head and Gerdy’s tubercle) using an adjustable length loop button, then passed deep to ITB and finally fixed posterior and proximal to the lateral femoral epicondyle with an interference screw, while the knee was positioned in 30º of flexion and neutral rotation. Additionally, Zarins and Rowe[51] proposed simultaneous ACLR and ALLR using only the ipsilateral ST. After proximal release, the ST was passed through the knee joint for ACLR, then exerted through a lateral femoral bone tunnel and tied to the ITB keeping the knee in 60º of flexion and tibial external rotation.
Escudeiro de Oliveira et al[52] reconstructed the ALL with an ipsilateral peroneus longus (PL) tendon graft and the ACL with a quintuple graft composed of a double-bundle ST, a double-bundle GT and a single-bundle PL. Specifically, the quintuple graft was initially used for ACLR, and the excess PL material was passed through a femoral tunnel, proximal and posterior to the lateral epicondyle, and was attached distally between the fibular head and Gerdy’s tubercle at 15 mm from the joint line. An interference screw was used in each attachment site, and during fixation the knee was kept at mild valgus and 30º of flexion. The authors supported the option of PL graft for ALLR as it could be easily harvested with minimal invasiveness. It was associated with low donor site morbidity and allowed adequate concomitant ACLR in combination with hamstring tendon autograft.
Josipovic et al[53] presented a technique of ALLR using the ipsilateral plantaris longus tendon. A quintuple graft composed of a three-strand ST and a two-strand GT was used for ACLR and a two-strand plantaris longus graft, which substituted the ALL, sutured to the quintuple graft. After the ACL graft fixation, the plantaris longus tendon was passed through a bone tunnel posterior and proximal to the lateral femoral epicondyle and fixed with an interference screw 10 mm distally from the joint line and midway between the fibular head and Gerdy’s tubercle, while the knee was fully extended. Although the authors reported good short-term results, there was a lack of data regarding the effectiveness of the technique.
Historically, Marshall et al[54] presented the Marshall-MacIntosh procedure using an autograft of quadriceps tendon-prepatellar retinaculum-patellar tendon for concomitant ACL and ALL recon
Some authors have recommended the application of allografts for ALLR, even in primary surgery, emphasizing the advantages of no donor site morbidity and availability of larger and longer grafts[56]. However, the use of allografts has been mainly suggested in revision surgery, where autografts may be not available in sufficient quantity[57]. Lee et al[25] used a GT allograft for ALLR in combination with tibialis anterior allograft for ACLR in the setting of revision surgery. Comparing ACLR with and without ALLR, they reported better outcomes after at least 3 years in terms of residual pivot shift, subjective IKDC score and Tegner score, return to the preinjury level of sports activity and possibility of revision surgery when ALLR was additionally performed. Chahla et al[57] underwent ALLR using an ST allograft mainly in cases requiring revision ACL surgery. However, they did not present any postoperative outcomes. Fernández et al[58] used an Achilles tendon allograft for both ACLR and ALLR in patients with previously failed ACLR and significant bone loss. They performed a two-stage procedure to fill the bone defect with a bone graft and to subsequently reconstruct the ACL and ALL. Still, no postsurgical outcome was reported.
Wagih and Elguindy[59] reported an ALLR technique using polyester tape. The synthetic ligament was attached proximally anterior and distal to the lateral femoral condyle with a cortical suspensory button. Distally, the graft was inserted between the Gerdy’s tubercle and the fibular head and stabilized via sutures that tied on the medial side of the tibia through two bone tunnels. During fixation, the knee was placed in 30º of flexion. The authors suggested that polyester tape ALLR might be worth further investigation as it was a minimally invasive technique without donor site morbidity. Furthermore, the material could offer adequate strength with minimal possibility of laxity and postoperative failure. However, no details about the postoperative outcome were provided.
The combination of ACLR with LET or ALLR can restore residual rotational laxity after isolated ACLR[60]. However, the LET procedure has been related to postoperative overconstraint of the internal rotation of the knee[34]. In a cadaveric study, Smith et al[34] reported similar results and equivalent restoration of knee kinematics between ALLR and LET after ACLR. Regarding knee position during graft fixation, Inderhaug et al[61] in a controlled ACLR laboratory study found that knee laxity was equally restored when ITB graft tenodesis was performed at 0º, 30º or 60º of knee flexion. On the other hand, ALLR using a GT graft achieved normal kinematics only when fixation was performed in full extension. Conversely, in another cadaveric study, Geeslin et al[62] found that both LET and ALLR were effective in reducing internal tibial rotation independently of the knee fixation angle or graft tension.
Additionally, Monaco et al[63] noticed that ALLR with GT showed superior biomechanical properties than LET, while the native ALL had lower failure load and stiffness compared to both grafts. Ra et al[64] found that LET resulted in similar rotational stability but worse anterior instability compared to ALLR. On the contrary, Spencer et al[65] reported that ALLR was less effective in reducing anterolateral rotational laxity than the LET procedure. Deviandri and van der Veen[66] used LET in four patients with residual rotational instability after ACLR and reported a significant improvement of knee kinematics.
In a recent meta-analysis, Yin et al[67] reported superior knee kinematics after combined ACLR and ALLR or LET compared to isolated ACLR in ACL deficient knees. Similarly, Littlefield et al[19] in a systematic review identified that supplementary ALLR during ACLR improved anterior tibial translation and internal knee rotation and resulted in a lower incidence of graft failure.
Current literature suggests that combined ACLR with ALLR or LET can improve clinical outcomes and decrease the possibility of ACL graft failure compared to isolated ACLR[43]. Beckers et al[68] observed that both LET and ALLR during ACLR provided superior Lysholm Score and reduced ACL re-rupture rate. Na et al[69] in a systematic review found that ALLR or LET along with ACLR were related to superior subjective IKDC, Tegner and Lysholm scores than isolated ACLR. However, the LET was associated with higher postoperative stiffness and complications than ALLR. Sonnery-Cottet et al[70] using data from 270 patients noticed that combined ACLR with ALLR led to a lower reoperation rate and better long-term graft survivorship but similar overall complication risk compared to isolated ACLR. The authors reported a 5-fold increase in the risk of ACL graft failure after a mean of 104 mo in cases of isolated ACLR. Similarly, in a systematic review of de Lima et al[71] the simultaneous ALLR and ACLR were related to better clinical outcomes than single ACLR, including higher success in return to sport and lower ACL graft rupture rate. The advantages and disadvantages of each technique are summarized in Table 2.
| Advantages | Disadvantages |
| 1. Lateral extraarticular tenodesis | |
| Improvement of rotational knee stability | Non-anatomic procedure |
| Reduction of ACL graft failure rate | Possible over-constraining |
| Reproducible, easy-to-learn technique | May add pain to postoperative rehabilitation |
| Inexpensive procedure, especially when using high-resistance suture | Muscle herniation, if ITB closure is not performed in proper way |
| No risk of tunnel coalition when fixed with sutures proximally | |
| 2. Anterolateral ligament reconstruction | |
| Improvement of rotational knee stability | Need ability to identify anatomic landmarks |
| Reduction of ACL graft failure rate | Use of allograft or synthetic results in increased cost |
| Preserves iliotibial band | Use of autograft requires additional surgery for graft harvest and possible donor site morbidity |
| Avoids lateral collateral ligament attachment | |
| Secure graft fixation allows for early motion and accelerated anterior cruciate ligament rehabilitation | |
Restoration of rotational stability is of paramount importance in the ACL injured knee. Apart from intraarticular ACLR, additional extraarticular procedures may be required to improve knee function and stability and minimize the risk for ACL graft failure. These include the LET and the ALLR with variable modifications of each procedure regarding the graft choice and fixation technique. Semitendinosus and gracilis are the main tendon grafts for ALLR, but other autografts such as peroneus longus, plantaris longus and quadriceps-patellar tendons have also been applied. Allografts and synthetic grafts are usually preferred in revision ACLR procedures where there is limited availability of autograft material for both ACLR and ALLR. Although all the available grafts for LET and ALLR may improve knee rotational stability, few studies with a relatively short follow-up and a small number of patients have been published so far. Therefore, there is inconclusive evidence to favor one method over the others in terms of biomechanical properties and clinical outcomes. Further large-scale studies are required to clarify the benefit of ALLR during primary or revision ACLR procedures. Particularly, future randomized control trials should compare ACLR with or without ALLR in young, active and high-demand patients by using different graft types. The research should focus on the subgroup of patients with large pivot-shift and operated meniscal tears aiming to find a potential correlation between ALLR and failure of ACLR under these conditions.
According to the current review and existing literature, there is no convincing evidence regarding the biomechanical and functional superiority of either LET or ALLR procedures during ACLR. Although hamstrings remain the most common graft choice for ALLR, other autografts as well as allografts and synthetic grafts have been applied with satisfactory results and low complication rate. However, a pooled analysis of all published raw data would further improve the quality of the review and related evidence despite the heterogeneity of the studies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Nambi G, Saudi Arabia; Zhou S, China S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2015;23:3186-3195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 226] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 2. | Musahl V, Herbst E, Burnham JM, Fu FH. The Anterolateral Complex and Anterolateral Ligament of the Knee. J Am Acad Orthop Surg. 2018;26:261-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Daggett M, Ockuly AC, Cullen M, Busch K, Lutz C, Imbert P, Sonnery-Cottet B. Femoral Origin of the Anterolateral Ligament: An Anatomic Analysis. Arthroscopy. 2016;32:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 4. | Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF. The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. Am J Sports Med. 2015;43:1606-1615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 274] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 5. | Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg. 2014;80:45-49. [PubMed] |
| 6. | Kosy JD, Soni A, Venkatesh R, Mandalia VI. The anterolateral ligament of the knee: unwrapping the enigma. Anatomical study and comparison to previous reports. J Orthop Traumatol. 2016;17:303-308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Runer A, Birkmaier S, Pamminger M, Reider S, Herbst E, Künzel KH, Brenner E, Fink C. The anterolateral ligament of the knee: A dissection study. Knee. 2016;23:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 8. | Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96-B:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 310] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 9. | Zens M, Niemeyer P, Ruhhammer J, Bernstein A, Woias P, Mayr HO, Südkamp NP, Feucht MJ. Length Changes of the Anterolateral Ligament During Passive Knee Motion: A Human Cadaveric Study. Am J Sports Med. 2015;43:2545-2552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 251] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 11. | Vundelinckx B, Herman B, Getgood A, Litchfield R. Surgical Indications and Technique for Anterior Cruciate Ligament Reconstruction Combined with Lateral Extra-articular Tenodesis or Anterolateral Ligament Reconstruction. Clin Sports Med. 2017;36:135-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA. The Role of the Anterolateral Structures and the ACL in Controlling Laxity of the Intact and ACL-Deficient Knee. Am J Sports Med. 2016;44:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 13. | Huser LE, Noyes FR, Jurgensmeier D, Levy MS. Anterolateral Ligament and Iliotibial Band Control of Rotational Stability in the Anterior Cruciate Ligament-Intact Knee: Defined by Tibiofemoral Compartment Translations and Rotations. Arthroscopy. 2017;33:595-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A. Prevalence and Classification of Injuries of Anterolateral Complex in Acute Anterior Cruciate Ligament Tears. Arthroscopy. 2017;33:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 142] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 15. | Tavlo M, Eljaja S, Jensen JT, Siersma VD, Krogsgaard MR. The role of the anterolateral ligament in ACL insufficient and reconstructed knees on rotatory stability: A biomechanical study on human cadavers. Scand J Med Sci Sports. 2016;26:960-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Prodromos CC, Joyce BT, Shi K, Keller BL. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21:1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44:593-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 18. | Saithna A, Thaunat M, Delaloye JR, Ouanezar H, Fayard JM, Sonnery-Cottet B. Combined ACL and Anterolateral Ligament Reconstruction. JBJS Essent Surg Tech. 2018;8:e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 19. | Littlefield CP, Belk JW, Houck DA, Kraeutler MJ, LaPrade RF, Chahla J, McCarty EC. The Anterolateral Ligament of the Knee: An Updated Systematic Review of Anatomy, Biomechanics, and Clinical Outcomes. Arthroscopy. 2021;37:1654-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Rosenstiel N, Praz C, Ouanezar H, Saithna A, Fournier Y, Hager JP, Thaunat M, Sonnery-Cottet B. Combined Anterior Cruciate and Anterolateral Ligament Reconstruction in the Professional Athlete: Clinical Outcomes From the Scientific Anterior Cruciate Ligament Network International Study Group in a Series of 70 Patients With a Minimum Follow-Up of 2 Years. Arthroscopy. 2019;35:885-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 21. | Patel RM, Brophy RH. Anterolateral Ligament of the Knee: Anatomy, Function, Imaging, and Treatment. Am J Sports Med. 2018;46:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 22. | Schon JM, Moatshe G, Brady AW, Serra Cruz R, Chahla J, Dornan GJ, Turnbull TL, Engebretsen L, LaPrade RF. Anatomic Anterolateral Ligament Reconstruction of the Knee Leads to Overconstraint at Any Fixation Angle. Am J Sports Med. 2016;44:2546-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 152] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 23. | Drews BH, Kessler O, Franz W, Dürselen L, Freutel M. Function and strain of the anterolateral ligament part I: biomechanical analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25:1132-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Stentz-Olesen K, Nielsen ET, de Raedt S, Jørgensen PB, Sørensen OG, Kaptein B, Søballe K, Stilling M. Reconstructing the anterolateral ligament does not decrease rotational knee laxity in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2017;25:1125-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Lee DW, Kim JG, Cho SI, Kim DH. Clinical Outcomes of Isolated Revision Anterior Cruciate Ligament Reconstruction or in Combination With Anatomic Anterolateral Ligament Reconstruction. Am J Sports Med. 2019;47:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 26. | Noyes FR, Huser LE, Jurgensmeier D, Walsh J, Levy MS. Is an Anterolateral Ligament Reconstruction Required in ACL-Reconstructed Knees With Associated Injury to the Anterolateral Structures? Am J Sports Med. 2017;45:1018-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 27. | Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P. The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am J Sports Med. 2016;44:1209-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 175] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 28. | Imbert P, Lutz C, Daggett M, Niglis L, Freychet B, Dalmay F, Sonnery-Cottet B. Isometric Characteristics of the Anterolateral Ligament of the Knee: A Cadaveric Navigation Study. Arthroscopy. 2016;32:2017-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 29. | Helito CP, Bonadio MB, Gobbi RG, da Mota E Albuquerque RF, Pécora JR, Camanho GL, Demange MK. Combined Intra- and Extra-articular Reconstruction of the Anterior Cruciate Ligament: The Reconstruction of the Knee Anterolateral Ligament. Arthrosc Tech. 2015;4:e239-e244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 30. | Wytrykowski K, Swider P, Reina N, Murgier J, Laffosse JM, Chiron P, Cavaignac E. Cadaveric Study Comparing the Biomechanical Properties of Grafts Used for Knee Anterolateral Ligament Reconstruction. Arthroscopy. 2016;32:2288-2294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Ahn JH, Patel NA, Lin CC, Lee TQ. The anterolateral ligament of the knee joint: a review of the anatomy, biomechanics, and anterolateral ligament surgery. Knee Surg Relat Res. 2019;31:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical Comparison of Anterolateral Procedures Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017;45:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 204] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 33. | Kraeutler MJ, Welton KL, Chahla J, LaPrade RF, McCarty EC. Current Concepts of the Anterolateral Ligament of the Knee: Anatomy, Biomechanics, and Reconstruction. Am J Sports Med. 2018;46:1235-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 34. | Slette EL, Mikula JD, Schon JM, Marchetti DC, Kheir MM, Turnbull TL, LaPrade RF. Biomechanical Results of Lateral Extra-articular Tenodesis Procedures of the Knee: A Systematic Review. Arthroscopy. 2016;32:2592-2611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 134] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 35. | Sonnery-Cottet B, Daggett M, Fayard JM, Ferretti A, Helito CP, Lind M, Monaco E, de Pádua VBC, Thaunat M, Wilson A, Zaffagnini S, Zijl J, Claes S. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee. J Orthop Traumatol. 2017;18:91-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 189] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 36. | Lemaire M, Combelles F. Plastic repair with fascia lata for old tears of the anterior cruciate ligament (author's transl). Rev Chir Orthop Reparatrice Appar Mot. 1980;66:523-525. [PubMed] |
| 37. | Christel P, Djian P. [Anterio-lateral extra-articular tenodesis of the knee using a short strip of fascia lata]. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:508-513. [PubMed] |
| 38. | Mathew M, Dhollander A, Getgood A. Anterolateral Ligament Reconstruction or Extra-Articular Tenodesis: Why and When? Clin Sports Med. 2018;37:75-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 39. | Abusleme S, Strömbäck L, Caracciolo G, Zamorano H, Cheyre J, Vergara F, Yañez R. Lateral Extra-articular Tenodesis: A Technique With an Iliotibial Band Strand Without Implants. Arthrosc Tech. 2021;10:e85-e89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Amirault JD, Cameron JC, MacIntosh DL, Marks P. Chronic anterior cruciate ligament deficiency. Long-term results of MacIntosh's lateral substitution reconstruction. J Bone Joint Surg Br. 1988;70:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 71] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Andrews JR, Sanders R. A "mini-reconstruction" technique in treating anterolateral rotatory instability (ALRI). Clin Orthop Relat Res. 1983;93-96. [PubMed] |
| 42. | Benum P. Anterolateral rotary instability of the knee joint. Results after stabilization by extraarticular transposition of the lateral part of the patellar ligament. A preliminary report. Acta Orthop Scand. 1982;53:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 181] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 44. | Sonnery-Cottet B, Barbosa NC, Tuteja S, Daggett M, Kajetanek C, Thaunat M. Minimally Invasive Anterolateral Ligament Reconstruction in the Setting of Anterior Cruciate Ligament Injury. Arthrosc Tech. 2016;5:e211-e215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 45. | Smith JO, Yasen SK, Lord B, Wilson AJ. Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3151-3156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 46. | Goncharov EN, Koval OA, Dubrov VE, Bezuglov EN, Filimonova AM, Goncharov NG. Clinical experience with combined reconstruction of the anterior cruciate and anterolateral ligaments of the knee in sportsmen. Int Orthop. 2019;43:2781-2788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Delaloye JR, Murar J, Vieira TD, Saithna A, Barth J, Ouanezar H, Sonnery-Cottet B. Combined Anterior Cruciate Ligament Repair and Anterolateral Ligament Reconstruction. Arthrosc Tech. 2019;8:e23-e29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 48. | Ferreira Mde C, Zidan FF, Miduati FB, Fortuna CC, Mizutani BM, Abdalla RJ. Reconstruction of anterior cruciate ligament and anterolateral ligament using interlinked hamstrings - technical note. Rev Bras Ortop. 2016;51:466-470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 49. | Colombet PD. Navigated intra-articular ACL reconstruction with additional extra-articular tenodesis using the same hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2011;19:384-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Kim MS, Koh IJ, In Y. Isometric Anterolateral Ligament Reconstruction Using the Semitendinosus Tendon With Suspensory Tibial Fixation. Arthrosc Tech. 2020;9:e941-e945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Zarins B, Rowe CR. Combined anterior cruciate-ligament reconstruction using semitendinosus tendon and iliotibial tract. J Bone Joint Surg Am. 1986;68:160-177. [PubMed] |
| 52. | Escudeiro de Oliveira D, Picchi Zaccharias V, Mayumi Horita M, Gabriel Betoni Guglielmetti L, Duarte Junior A, Baches Jorge P. Anterior Cruciate and Anterolateral Ligament Reconstruction Using Hamstring and Peroneus Longus Tendons: Surgical Technique Description. Arthrosc Tech. 2021;10:e397-e402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 53. | Josipović M, Vlaić J, Serdar J, Šimunović M, Nizić D, Schauperl Z, Bojanić I, Jelić M. Plantaris tendon: a novel graft for anterolateral ligament reconstruction and additional reinforcement for anterior cruciate ligament autografts in combined reconstructive procedures. Knee Surg Sports Traumatol Arthrosc. 2020;28:2604-2608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 54. | Marshall JL, Warren RF, Wickiewicz TL, Reider B. The anterior cruciate ligament: a technique of repair and reconstruction. Clin Orthop Relat Res. 1979;97-106. [PubMed] |
| 55. | Dupont JY, Bellier G, O'Brien WR. Modified Marshall-MacIntosh technique for anterior cruciate ligament substitution with early knee rehabilitation. Techniques in Orthopaedics. 1988;2:28-35. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 56. | McGuire DA, Wolchok JC. Extra-articular lateral reconstruction technique. Arthroscopy. 2000;16:553-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 57. | Chahla J, Menge TJ, Mitchell JJ, Dean CS, LaPrade RF. Anterolateral Ligament Reconstruction Technique: An Anatomic-Based Approach. Arthrosc Tech. 2016;5:e453-e457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 58. | Maestro Fernández A, Pipa Muñiz I, Rodríguez García N. Two-Stage Anterior Cruciate Ligament Reconstruction Revision Surgery for Severe Bone Defects With Anterolateral Ligament Reconstruction Technique. Arthrosc Tech. 2020;9:e327-e337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Wagih AM, Elguindy AM. Percutaneous Reconstruction of the Anterolateral Ligament of the Knee With a Polyester Tape. Arthrosc Tech. 2016;5:e691-e697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 60. | Jette C, Gutierrez D, Sastre S, Llusa M, Combalia A. Biomechanical comparison of anterolateral ligament anatomical reconstruction with a semi-anatomical lateral extra-articular tenodesis. A cadaveric study. Knee. 2019;26:1003-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 61. | Inderhaug E, Stephen JM, Williams A, Amis AA. Anterolateral Tenodesis or Anterolateral Ligament Complex Reconstruction: Effect of Flexion Angle at Graft Fixation When Combined With ACL Reconstruction. Am J Sports Med. 2017;45:3089-3097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 62. | Geeslin AG, Moatshe G, Chahla J, Kruckeberg BM, Muckenhirn KJ, Dornan GJ, Coggins A, Brady AW, Getgood AM, Godin JA, LaPrade RF. Anterolateral Knee Extra-articular Stabilizers: A Robotic Study Comparing Anterolateral Ligament Reconstruction and Modified Lemaire Lateral Extra-articular Tenodesis. Am J Sports Med. 2018;46:607-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 144] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 63. | Monaco E, Lanzetti RM, Fabbri M, Redler A, De Carli A, Ferretti A. Anterolateral ligament reconstruction with autologous grafting: A biomechanical study. Clin Biomech (Bristol, Avon). 2017;44:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 64. | Ra HJ, Kim JH, Lee DH. Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: systematic review and meta-analysis. Arch Orthop Trauma Surg. 2020;140:923-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 65. | Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, Getgood AM. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:2189-2197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 187] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 66. | Deviandri R, van der Veen HC. Isolated lateral extra-articular tenodesis enhance better rotatory knee joint stability post-primary ACL repair: Four cases report and literature review. Int J Surg Case Rep. 2021;84:106167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 67. | Yin J, Yang K, Zheng D, Xu N. Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: A meta-analysis. J Orthop Surg (Hong Kong). 2021;29:2309499020985195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 68. | Beckers L, Vivacqua T, Firth AD, Getgood AMJ. Clinical outcomes of contemporary lateral augmentation techniques in primary ACL reconstruction: a systematic review and meta-analysis. J Exp Orthop. 2021;8:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 69. | Na BR, Kwak WK, Seo HY, Seon JK. Clinical Outcomes of Anterolateral Ligament Reconstruction or Lateral Extra-articular Tenodesis Combined With Primary ACL Reconstruction: A Systematic Review With Meta-analysis. Orthop J Sports Med. 2021;9:23259671211023099. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 70. | Sonnery-Cottet B, Haidar I, Rayes J, Fradin T, Ngbilo C, Vieira TD, Freychet B, Ouanezar H, Saithna A. Long-term Graft Rupture Rates After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction: A Matched-Pair Analysis From the SANTI Study Group. Am J Sports Med. 2021;49:2889-2897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 71. | Ariel de Lima D, de Lima LL, de Souza NGR, de Moraes Perez RA, Sobrado MF, Guimarães TM, Helito CP. Clinical outcomes of combined anterior cruciate ligament and anterolateral ligament reconstruction: a systematic review and meta-analysis. Knee Surg Relat Res. 2021;33:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 72. | Guenther D, Irarrázaval S, Bell KM, Rahnemai-Azar AA, Fu FH, Debski RE, Musahl V. The Role of Extra-Articular Tenodesis in Combined ACL and Anterolateral Capsular Injury. J Bone Joint Surg Am. 2017;99:1654-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 73. | Smith PA, Bley JA. Minimally Invasive Anterolateral Ligament Reconstruction of the Knee. Arthrosc Tech. 2016;5:e1449-e1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |