Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.8040
Peer-review started: March 8, 2022
First decision: April 13, 2022
Revised: April 28, 2022
Accepted: June 14, 2022
Article in press: June 14, 2022
Published online: August 6, 2022
Processing time: 135 Days and 14.9 Hours
Malignant tumors of the appendix are extremely rare, constituting about 1% of all gastrointestinal tumors. Generally, pathology identifies these tumors during or after appendectomy because they are difficult to detect at the preoperative stage. This case report aims to introduce the definitive diagnosis and treatment of mucinous adenocarcinoma of the appendix.
A 49-year-old female patient came to our hospital with right lower abdominal pain, nausea, and vomiting for three days. There was no change in the menstrual cycle. Gynecological ultrasound showed a cystic, solid mass in the right adnexa. Abdominal enhanced computed tomography showed a thick appendix. Cancer was found on exploration of the appendix during gynecological surgery. The right colon was removed. After surgery, the patient received chemotherapy and is recovering well.
Appendiceal carcinoma is frequently found during or after surgery, and both preoperative examination and early evaluation of clinical manifestations are extremely important.
Core Tip: Mucinous adenocarcinoma of the appendix has a low incidence rate and is relatively rare. Increased tumor markers in patients has certain guiding significance. Imaging examination can indicate that the appendix is thickened, and diagnosis depends on histopathology.
- Citation: Wang L, Dong Y, Chen YH, Wang YN, Sun L. Accidental discovery of appendiceal carcinoma during gynecological surgery: A case report. World J Clin Cases 2022; 10(22): 8040-8044
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/8040.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.8040
Malignant appendix epithelial tumors can be divided into three categories: mucinous adenocarcinoma of the appendix (MAA)[1], intestinal type of adenocarcinoma, and signet ring cell carcinoma. Of these, MAA is the most prevalent histological form. Its occurrence may be linked to chronic inflammatory infiltration of the appendix. Here, we report a case of appendiceal mucinous adenocarcinoma, accidentally found during surgery for right lower abdominal pain and a pelvic mass. We also reviewed available relevant literature.
A 49-year-old female patient came to our hospital with right lower abdominal pain, nausea, and vomiting.
The patient’s symptoms started three days ago with right lower abdominal pain, nausea, and vomiting.
There was no change in the menstrual cycle. The patient had no previous medical history.
The patient is in good health and has no family genetic diseases.
Gynecologic examination suggested normal vulvar development, a smooth vagina, little vaginal discharge, a soft cervix, an average size uterus, and no tenderness. There was no abnormality in the left accessories, and a cystic solid tumor approximately 6 cm in size was palpated in the right accessories.
Human epididymal protein 4 (HE4), carcinoembryonic antigen (CEA), and alpha- fetoprotein (AFP) levels were normal on May 14, 2021. The patient’s CA125 level was 392.9 U/mL and CA199 level was 88.27 U/mL on May 14, 2021.
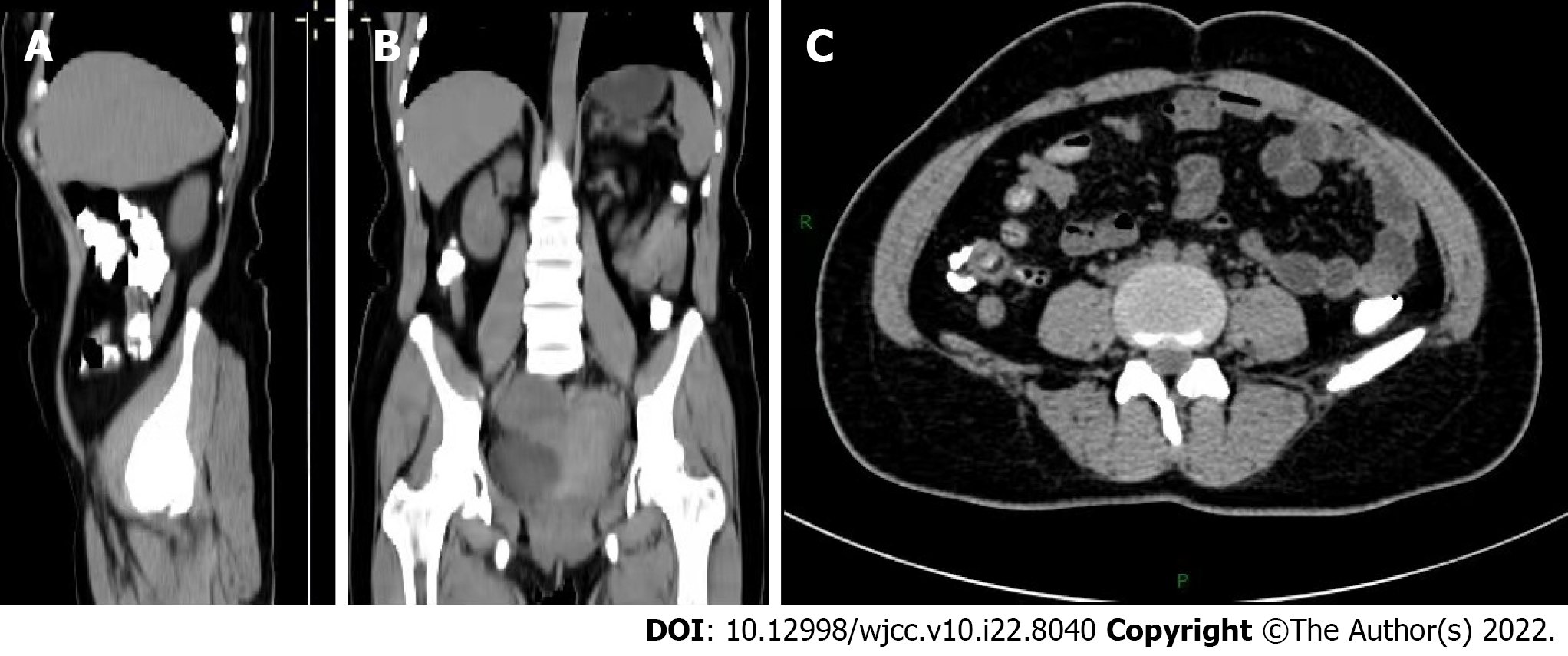
Gynecological ultrasound on May 15, 2021, showed a cystic, solid mass in the right adnexa area approximately 6.2 cm × 5.6 cm × 5.8 cm in size, with an unclear right ovary. On May 18, 2021, a complete abdominal computed tomography (CT) scan showed a hypocystic shadow in the right adnexa area with a visible compartment inside and appendiceal thickening with a maximal thickness of around 12 mm (Figure 1). The mass in the pelvic cavity was unidentified.
The patient underwent an exploratory laparotomy on May 21, 2021, during which the right accessory and cystic mass were removed, thickening of the appendix (~6 cm in length and ~1 cm in diameter) was noted, with a hard texture and edema, attached to the posterior wall of the ascending colon. Appendiceal malignancy could not be excluded, and was diagnosed following rapid intraoperative pathology. The final diagnosis of the presented case was MAA.
Gastrointestinal surgery consisting of a right hemicolectomy and peripheral lymph node dissection was performed. The residual intestine, stomach, liver, greater omentum, and peritoneum surface were examined at the end of surgery, and no abnormalities were found.
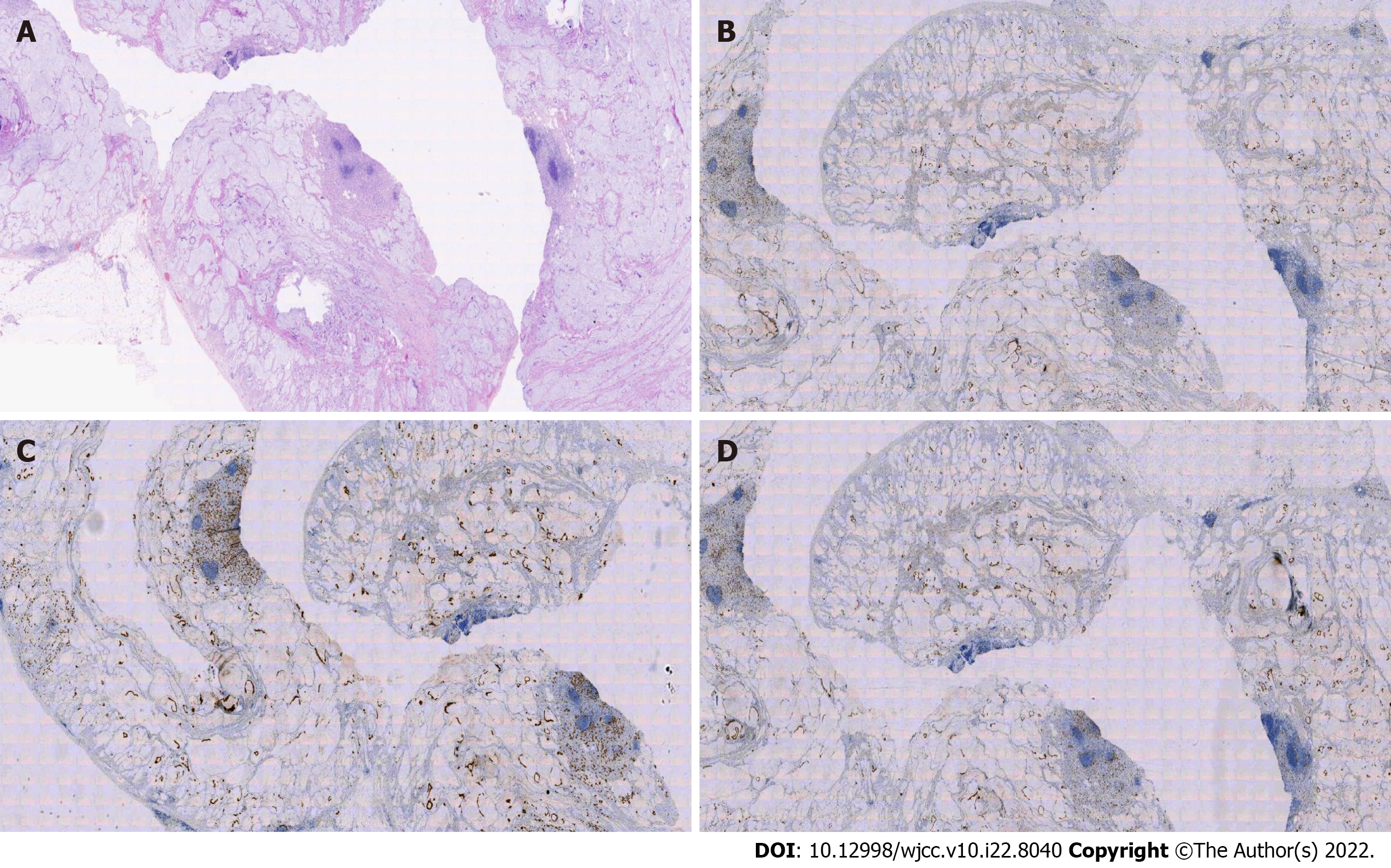
Postoperative pathology confirmed mucinous adenocarcinoma of the appendix with partial signet-ring cell carcinoma. Immunohistochemistry was performed using the following markers: CDX-2 (+), CK7 (-), CK20 (+), CA125 (-), CD56 (-), Syn (-), Pax-8 (-), WT-1 (-), and SATB2 (+) (Figure 2). The patient received chemotherapy 45 days after the operation. Six courses of XELOX chemotherapy (Oxaliplatin + Capecitabine) were completed, and there was no evidence of recurrence. MAA with signet-ring cell features is considered more invasive and has a worse prognosis. The patient requires regular follow-up every four months for three years, every six months for the next two years, and then every year for the next 15 years, following initial therapy[2].
MAA is a rare disease characterized by elevated CA199 and CEA levels. C. PABLO et al showed that tumor markers CEA and CA199 have high clinical value in diagnosing MAA[3,4]. Moreover, the increasing level of CA125 while maintaining normal HE4 helps discriminate between benign and malignant ovarian tumors. Our patient showed elevated CA199 and CA125 levels, which can help diagnose appendiceal lesions[5]. Moh M used immunohistochemistry to identify SATB (-) in ovarian mucinous tumors. The presence of SATB2 (+) and CDX-2 (+) highly suggests that the tumor originates from the colon or appendix[4]. Imaging is a useful diagnostic tool for MAA. Ultrasound observations revealed a cystic mass in the appendix, heterogeneous echogenicity, hypocystic or tubular lesions in the appendix, and irregular thickening. CT scans can rule out appendiceal inflammation and abscess, and all the above findings help diagnose mucinous cystadenoma[1,6]. MAA is difficult to diagnose due to the non-specific nature of early symptoms, including lower abdominal pain, weight loss, nausea, vomiting, a palpable mass, and acute appendicitis, and is frequently misdiagnosed as a gynecological condition such as right adnexal mass[7]. The bladder may also be affected, with symptoms of bladder irritation or the formation of hematuria, leading to a misdiagnosis of urinary tract infection or bladder cancer[8-10]. In most cases, appendiceal malignancy is detected accidentally by abdominal CT or surgery for appendicitis due to other reasons. Appendiceal cancer is difficult to identify even by preoperative colonoscopy[11]. In the case of submucosal lesions of the cecum near the mouth of the appendix, mucus flows out of the mouth of the appendix; thus, the treating physician should be highly vigilant against appendiceal lesions. Mucinous adenocarcinoma of the appendix is associated with a high risk of peritoneal seeding along with hematogenous and lymph node metastasis. As a surgical treatment for mucinous adenocarcinoma, simultaneous surgical removal of the appendix and right hemicolectomy with peripheral lymph node dissection is preferred[12]. Laparotomy is superior to laparoscopic surgery as it facilitates identification of the involvement of other organs. It is better to protect against incision, thereby avoiding mass rupture, leading to intra-peritoneal dissemination and affecting prognosis.
MAA is remarkably rare, difficult to diagnose and distinguish from other tumors. Preoperative laboratory and imaging examinations, and a well-planned diagnostic and treatment strategy are essential. In mucinous neoplasms, we believe that a right hemicolectomy should definitely be performed if required for tumor clearance because a complete cytoreduction of mucinous tumors of the appendix is associated with improved survival[12,13]. The patient described here presented with common clinical symptoms of MAA. For patients with the appearance of an abnormal appendix during preoperative examination, it is necessary to examine the appendix at the same time to avoid missed diagnosis and misdiagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jha AK, United States; Keeratibharat N, Thailand; Mechineni A, United States A-Editor: Zhu JQ, United States S-Editor: Wang LL L-Editor: Webster JR P-Editor: Wang LL
| 1. | Van Hooser A, Williams TR, Myers DT. Mucinous appendiceal neoplasms: pathologic classification, clinical implications, imaging spectrum and mimics. Abdom Radiol (NY). 2018;43:2913-2922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 2. | Delhorme JB, Villeneuve L, Bouché O, Averous G, Dohan A, Gornet JM, You B, Bibeau F, Dartigues P, Eveno C, Fontaine J, Kepenekian V, Pocard M, Rousset P, Quenet F, Mariani P, Glehen O, Goéré D. Appendiceal tumors and pseudomyxoma peritonei: French Intergroup Clinical Practice Guidelines for diagnosis, treatments and follow-up (RENAPE, RENAPATH, SNFGE, FFCD, GERCOR, UNICANCER, SFCD, SFED, SFRO, ACHBT, SFR). Dig Liver Dis. 2022;54:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 3. | Shin KH, Kim HH, Kwon BS, Suh DS, Joo JK, Kim KH. Clinical Usefulness of Cancer Antigen (CA) 125, Human Epididymis 4, and CA72-4 Levels and Risk of Ovarian Malignancy Algorithm Values for Diagnosing Ovarian Tumors in Korean Patients With and Without Endometriosis. Ann Lab Med. 2020;40:40-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Yan F, Shi F, Li X, Yu C, Lin Y, Li Y, Jin M. Clinicopathological Characteristics of Pseudomyxoma Peritonei Originated from Ovaries. Cancer Manag Res. 2020;12:7569-7578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Wang B, Yao J, Ma R, Liu D, Lu Y, Shi G, An L, Xia A, Chen F, Pang S, Zhai X, Liu G, Chen S, Xu M, Song L, Xu H. The mutational landscape and prognostic indicators of pseudomyxoma peritonei originating from the ovary. Int J Cancer. 2021;148:2036-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Tirumani SH, Fraser-Hill M, Auer R, Shabana W, Walsh C, Lee F, Ryan JG. Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging. 2013;13:14-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 7. | Ma Q, Wu J. Endometrioid Adenocarcinoma With Solitary Metastasis to the Appendix, Mimicking Primary Appendiceal Adenocarcinoma: A Case Report and Literature Review. Int J Gynecol Pathol. 2019;38:393-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Roma K, Baldwin M, Sedmak D, Silva M, Stellar W, Many G. Late stage diagnosis of mucinous adenocarcinoma of the appendix: a case report of an unusual tumor with a rare presentation. BMC Gastroenterol. 2020;20:281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Subramanya D, Grivas PD, Styler M. Appendiceal carcinoma: a diagnostic and therapeutic challenge. Postgrad Med. 2008;120:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Turaga KK, Pappas S, Gamblin TC. Right hemicolectomy for mucinous adenocarcinoma of the appendix: just right or too much? Ann Surg Oncol. 2013;20:1063-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Trivedi AN, Levine EA, Mishra G. Adenocarcinoma of the appendix is rarely detected by colonoscopy. J Gastrointest Surg. 2009;13:668-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Shaib WL, Assi R, Shamseddine A, Alese OB, Staley C 3rd, Memis B, Adsay V, Bekaii-Saab T, El-Rayes BF. Appendiceal Mucinous Neoplasms: Diagnosis and Management. Oncologist. 2017;22:1107-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 134] [Article Influence: 16.8] [Reference Citation Analysis (3)] |
| 13. | Lu P, Fields AC, Meyerhardt JA, Davids JS, Shabat G, Bleday R, Goldberg JE, Nash GM, Melnitchouk N. Systemic chemotherapy and survival in patients with metastatic low-grade appendiceal mucinous adenocarcinoma. J Surg Oncol. 2019;120:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (1)] |