Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7960
Peer-review started: December 21, 2021
First decision: May 11, 2022
Revised: May 31, 2022
Accepted: June 21, 2022
Article in press: June 21, 2022
Published online: August 6, 2022
Processing time: 212 Days and 22 Hours
Ewing’s sarcoma is a highly malignant primary bone tumor that commonly affects children. For young patients, multidisciplinary treatment and limb salvage are recommended, and surgical plans considering the growth potential and bone activity after tumor resection are essential.
An 11-year-old Asian boy had a 1-mo history of a right-sided limping gait. Imaging revealed a proximal tumor with bone destruction and physeal involvement over the right femoral neck. He was diagnosed with stage IV (T1N0M1aG3) Ewing’s sarcoma with bilateral lung metastases. Neoadjuvant chemotherapy decreased the tumor size and confined it to the metaphyseal region. The patient underwent four stages of surgery: wide tumor excision plus reconstruction with vascular fibular bone graft plus internal fixation; repeat open reduction and internal fixation; femoral lengthening with orthosis after physeal maturity; and orthosis removal and bone elongation (approximately 6 cm). Following surgery, he could walk without discomfort and had almost equal-sized bilateral femoral heads, indicating physis preservation. The surgery was successful, and normal femoral head growth was achieved after complete remission. The patient was able to resume normal activities with equal length of the bilateral lower limbs.
Tumor treatment and reconstruction following resection are important in skeletally immature patients with Ewing’s sarcoma to improve quality of life.
Core Tip: Ewing’s sarcoma is an uncommon primary malignant bone tumor, and its treatment is a challenge to the orthopedic surgeon. Beyond survival, current treatment also focuses on functional preservation and cosmetic appearance. This 9-year follow-up case illustrates the complete treatment course from resection to reconstruction and rehabilitation for Ewing’s sarcoma, which demonstrates a complete clinical picture for pediatric specialist and pediatric surgeons dealing with complex tumor surgery. The patient not only achieved complete remission, but also had good functional outcomes with limb salvage.
- Citation: Lai CY, Chen KJ, Ho TY, Li LY, Kuo CC, Chen HT, Fong YC. Resection with limb salvage in an Asian male adolescent with Ewing’s sarcoma: A case report. World J Clin Cases 2022; 10(22): 7960-7967
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7960.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7960
Ewing’s sarcoma is a primary malignant tumor that usually occurs in children. It was first described in 1921 by Ewing J. Ewing’s sarcoma constitutes 17.2% of primary malignant bone tumors in the Caucasian population. In a previous study, the ratio of Ewing’s sarcoma to osteosarcoma was 0.1 in the Chinese group and 0.31 in the American group[1].
A previous study of primary bone cancer in Taiwan conducted between 2003 and 2010 showed that Ewing’s sarcoma accounted for only approximately 8% of all cases[2]. The tumor most commonly occurs in the long bone diaphysis, and the most common site is the femur (22%), followed by the long bones of the lower extremities, including the femur (30%) and the pelvis (19%)[3-5].
Ewing’s sarcoma generally has a favorable prognosis. The Cooperative Ewing’s Sarcoma Study Group reported a 10-year event-free survival rate of approximately 53% in 301 patients with a median age of 15 years. This predilection for the pediatric population and good prognosis underlines the importance of quality of life in addition to survival[6]. However, the Enneking staging system, the most popular surgical staging system for musculoskeletal sarcomas, is not applicable to Ewing’s sarcoma, probably because it does not originate from the mesenchymal connective tissue of the musculoskeletal system, indicating the uniqueness of this tumor[7].
With respect to treatment, a multidisciplinary approach involving neoadjuvant chemotherapy, followed by tumor resection and adjuvant chemotherapy, is required. Non-metastatic, non-recurrent cases have an expected survival rate of 60%-80%[4]. Postoperative radiotherapy has no survival benefit in patients with metastases but improves survival for those with positive surgical margins[8]. Physical function and cosmetic appearance have also become more important in recent years. However, reconstruction after wide resection is difficult in adolescents because of the growth potential and activity.
An 11-year-old boy presented with a 1-mo history of a right-sided limping gait.
The patient fell approximately 1 mo prior to admission. Since this accident, he had persistent pain in his right hip and a right-sided limping gait.
He had a known diagnosis of bilateral pes planus.
The patient’s mother was G2P2A0; he was born via normal spontaneous delivery at a gestational age of 39 wk. His birth weight was 3300 gm. His parents did not have any specific medical or cancer history.
Physical examination revealed swelling of the right proximal femur and hip, tenderness over the right hip and lateral thigh, right hip pain with passive range of motion, and a right-sided limping gait due to weight-bearing pain. He had no loss of muscle power and sensation in the right lower limb.
Blood tests revealed the following: lactate dehydrogenase, 401 IU/L; alkaline phosphatase, 158 IU/L; and C-reactive protein, 0.93 mg/dL. Chromosome analysis reported normal male 46,XY karyotype.
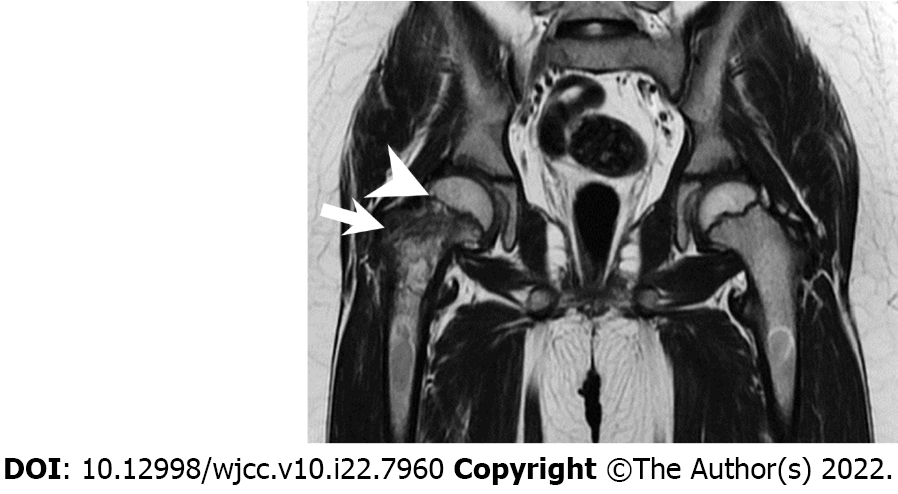
Radiography showed focal bone destruction and osteolytic change over the right femoral neck (Figure 1A). Magnetic resonance imaging showed an intra-skeletal mass in the metaphyseal region with physeal involvement (Figure 1B). Chest computed tomography also indicated bilateral lung metastases (Figure 2).
We discussed the case with an expert pediatric hematologist (Wu KH, MD, Chief Doctor, Professor, at the China Medical University Hospital) after tumor biopsy reported Ewing’s sarcoma. Neoadjuvant chemotherapy was recommended, and adjuvant chemotherapy was also needed after tumor resection.
Based on these findings, the patient was diagnosed with stage IV Ewing’s sarcoma (T1N0M1aG3). Histological examination of an incisional biopsy specimen confirmed the diagnosis of Ewing’s sarcoma/primitive neuroectodermal tumor, and the tumor was positive for CD-99 and periodic acid-Schiff staining.
Neoadjuvant chemotherapy with cisplatin, cyclophosphamide, doxorubicin, etoposide, ifosfamide, and vincristine sulfate decreased the tumor size, with the tumor confined to the metaphyseal region (Figure 3). The patient then underwent four stages of surgery.
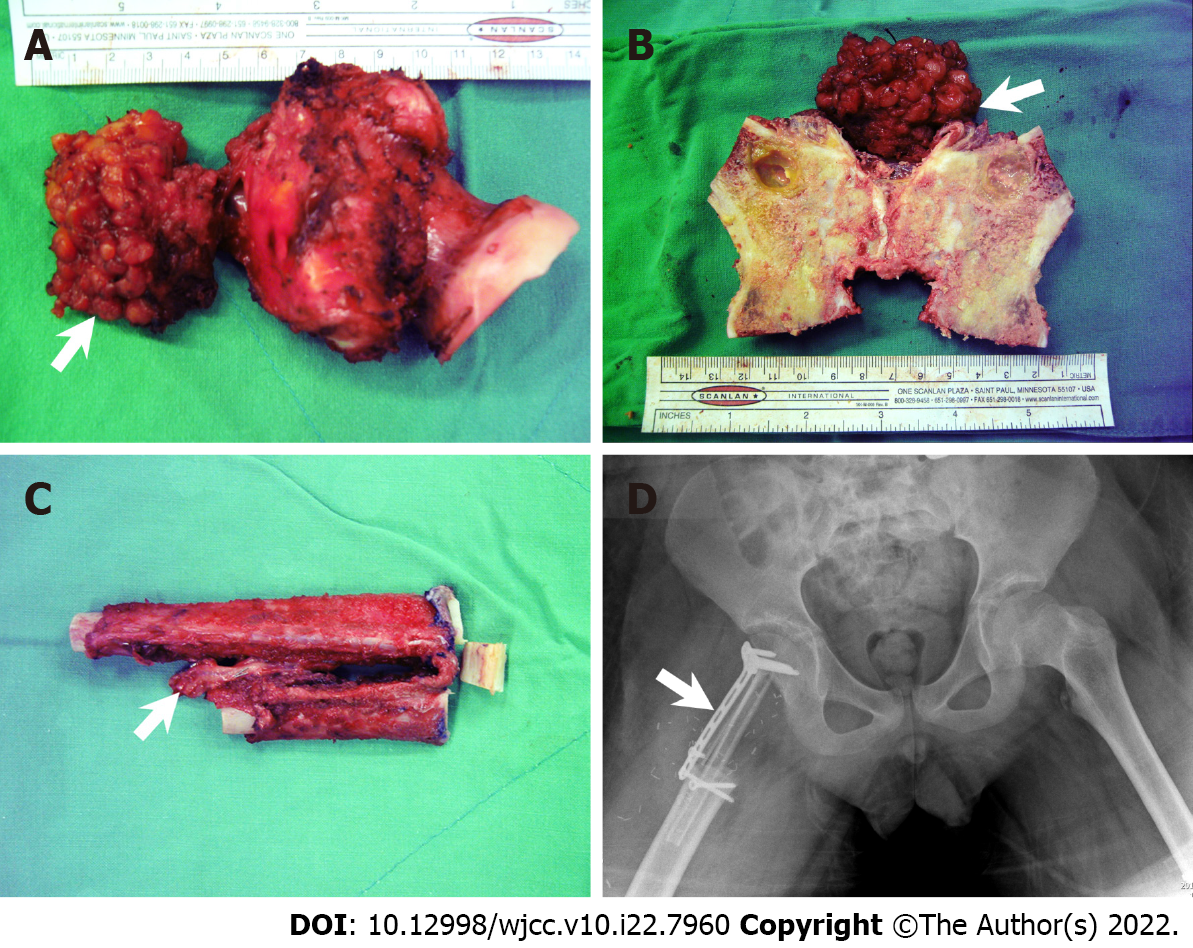
Wide excision of the tumor (physeal preservation) plus reconstruction with a vascular fibular bone graft plus fixation with a locking T-plate (Figure 4). The patient was placed in the supine position, and an incision from the lateral aspect of the thigh was made via the standard lateral approach. The tumor was then dissected and subjected to intra-operative frozen section pathology. After complete margin resection was confirmed, the femur and proximal femur were removed to harvest the vascular bone graft from the right fibula via the standard lateral approach. The distal ends of the peroneal artery and vein were divided, and the dissection was carried on toward the cephalic end. The vessel branches were ligated, and the flap was harvested based on the right peroneal artery and vein. The total length of the fibula flap was 17 cm, leaving 5 cm distally and 5 cm proximally. The graft was divided into two parts: proximal (10 cm with main blood supply) and distal (6 cm for augmentation of contact with the femoral head). The vascular fibular graft was transferred to the femur, and a vascular anastomosis of the branch of the lateral femoral circumflex artery and vein was performed. Then, the vascular fibular graft was fixed with an Arbeitsgemeinschaft für Osteosynthesefragen (AO) locking plate at the right hip and the distal tibial and fibular with a screw to ensure ankle stability.
The resected mass obtained after performing stage 1 surgery showed a tumor in the metaphysis and adjacent periosteal soft tissue with patchy myelofibrosis and avascular necrosis, but no residual malignant cells, lymphovascular permeation, or perineural invasion. A bone-destructive lesion measuring 3.5 cm × 1.6 cm was found over the distal metaphyseal site of the femur.
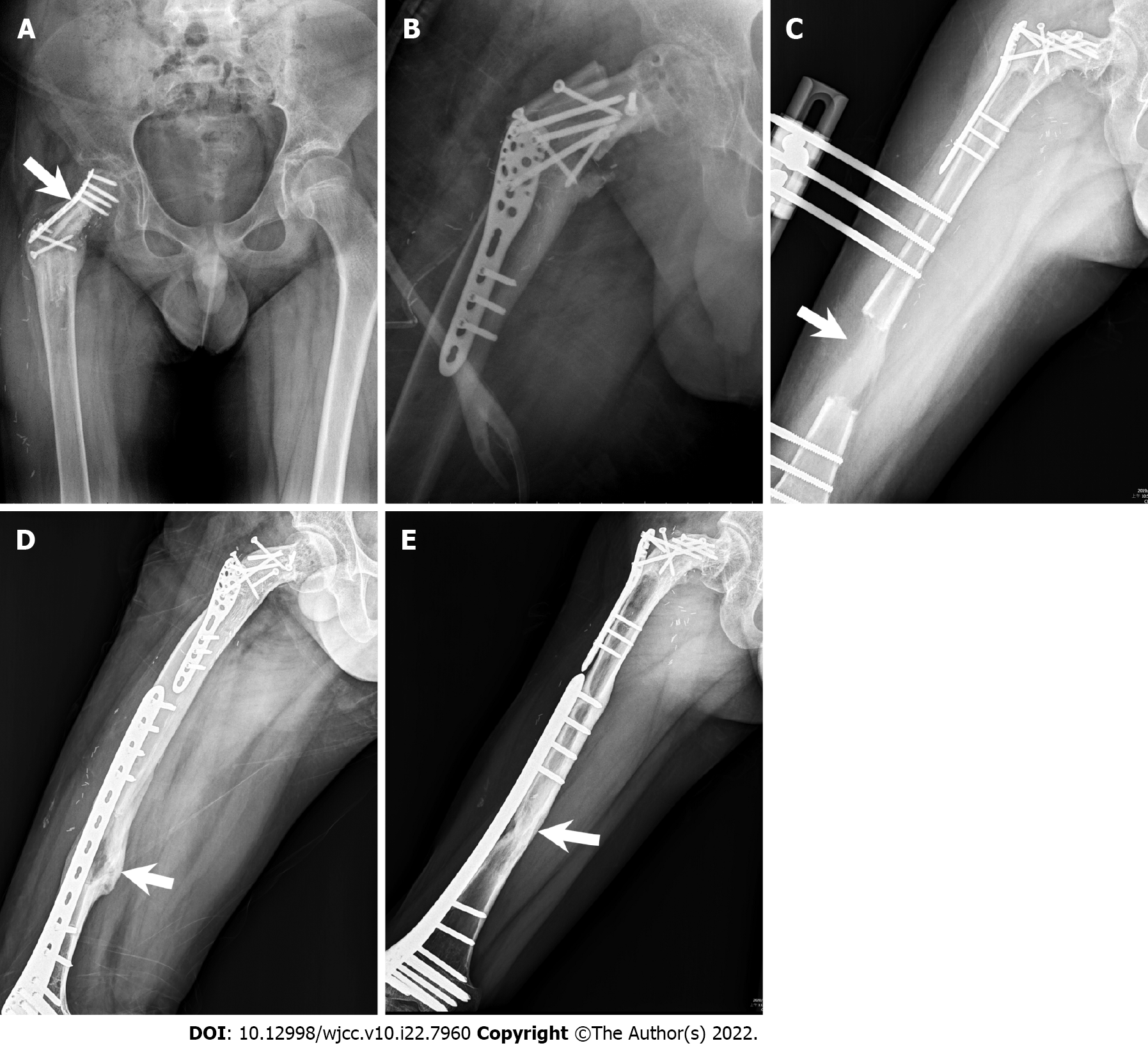
After 5 mo, the patient started with gradual limited weight bearing on the right hip. After 14 mo, partial weight bearing (over 30 kg) and walking with a crutch were achieved. However, the plate deformed with broken screws after an increase in partial weight bearing (Figure 5A).
After 16 mo, we performed a repeat open reduction and internal fixation for the plate impending failure and malalignment of the vascular fibular bone graft with the AO proximal humeral internal locking system (PHILOS) plate (Figure 5B). The femoral head had enlarged with age, but there was also a limb length discrepancy. After a 7.5-year follow-up period since the tumor excision surgery, a symmetric bilateral hip joint surface and equal femoral head size were noted on radiography. There was also no osteonecrotic change in the right femoral head. The right and left lower limb length were 77 and 83 cm, respectively, with a lower limb discrepancy of 6 cm.
Femoral lengthening with orthosis with a distraction rate of 1 mm/day (Figure 5C).
Orthosis removal. The AO less-invasive stabilization system locking compression plate elongated the bone by approximately 6 cm.
Two months postoperatively, plain film radiography showed complete corticalization of the elongated femur (Figure 5D). The last follow-up plain film was obtained 14 mo postoperatively, and it showed good bone formation of the elongated femur (Figure 5E). The Musculoskeletal Tumor Society score was 28, and the Harris hip score was 96, 16 mo postoperatively[9,10].
Data on the long-term outcomes of Ewing’s sarcoma are currently lacking[2,11]. In Taiwan, Ewing’s sarcoma accounted for only 8% of all bone cancer cases during 2003-2010[12]. We reported the case of an adolescent patient with Ewing’s sarcoma who underwent three types of surgery. The first was a successful hip joint preservation, with the final imaging during follow-up showing an equal femoral head diameter and joint surface congruity. The second was graft substitution of the femoral neck with vascular autograft for the preservation of growth potential, and the choice of bone and implant for augmentation and fixation. The third was femoral lengthening technique selected to enable the patient to regain normal ambulatory capacity.
Despite novel treatment modalities, oncological surgery remains crucial for improving survival. In addition, both patients and their family are concerned about regaining normal function and cosmetic appearance after tumor resection. Given that Ewing’s sarcoma affects the bones and soft tissues, potential functional changes are an important consideration when planning surgery. The three main growth areas in the proximal femur are the physeal plate, the growth plate of the greater trochanter, and the femoral neck isthmus. The proximal femoral physeal plate contributes to approximately 30% of the overall length of the femur, and 13% of the entire lower limb[13]. It is important to preserve joint function and activity if limb preservation can be expected, especially in pediatric patients who still have growth potential.
A malignant tumor in the proximal femur can affect the hip joint. Once we decided to perform limb salvage surgery, age, growth potential, and physis involvement were the first factors to be considered. Tsuchiya et al[14] used a vascular fibular graft to allow growth of the physis in the fibula in the hip joint, with cadaveric femoral allograft as reinforcement. However, this method has not yet been proven to effectively enable growth. Intra-epiphyseal excision is sometimes an option for long bone tumors[15]. In our case, we selected a hip joint preservation technique. Tumor resection in the proximal femur, particularly the femoral neck, arthroplasty, or vascular bone graft with allograft bone augmentation as a structural graft, can be performed in adult patients[14,16].
Although vascular grafts allow for bony growth in pediatric patients, surgery allows enlargement of the hip joint; thus, hip-preservation surgery is needed. Furthermore, the small diameter of the femoral neck makes it challenging to obtain an appropriate proximal femoral allograft in this patient population. Re-implantation of the resected proximal femur bone post cryotherapy is another option to reinforce the biomechanical construct[13]. We used a folded autologous vascular fibula graft reconstructed from the proximal femur, particularly the femoral neck. However, given that the tumor was not resected from the femoral subtrochanteric region and that the patient was only 11 years old, we used a locking plate to stabilize the vascular fibula graft[17]. The Capanna technique was not suitable in our case, because the literature on pediatric allograft is limited, and the smaller bone diameter makes this technique challenging, as it involves a sandwich-like bone graft. If we performed a reconstruction technique similar to that for adults, hemi-arthroplasty is an option with a low risk of mechanical failure. However, the bony growth of the proximal femur in our patient did not reach the expected length, and thus, the implant failed. Accordingly, we performed another surgery with AO PHILOS after 1.5 years. This allowed for better biomechanical distribution of the head-neck force to the femoral shaft, and the vascular graft successfully combined.
After 8 years, the diameter of the femoral head was equal to that of the other site, indicating that preservation of the physis allowed for enlargement of the hip joint. However, the length discrepancies remained an issue. Similar to those in the tibia, complications, particularly infection, in extra-skeletal fixation are of great concern[18,19]. Concerning the femoral lengthening device, an extra-skeletal mono-lateral system, such as orthosis, is an efficient approach that does not require joint involvement. The system avoids broken screws and allows for preservation of the remaining physis[20]. One study compared limb length discrepancies among elongation devices in 73 patients with Ewing’s sarcoma or osteosarcoma, and found that 10 patients required secondary lengthening. The average length achieved was 8.1 cm, and the final residual discrepancy was 1.5-2.5 cm.
Angulation, torsion, osteoporosis, joint instability, muscular weakness, and patient and family cooperation are factors that must be considered prior to long bone elongation surgery. In general, the patient needs to undergo the following five phases before removing the orthosis: (1) Osteotomy; (2) Latency; (3) Distraction; (4) Neutralization; and (5) Consolidation[19]. Physical activity is limited during the consolidation phase and the percutaneous pins of orthosis also increase the risk of pin tract infection. An internal fixation with a locking plate prevents these problems. The patient underwent another surgery after the complete distraction phase to change the orthosis to an internal fixator during the consolidation phase.
Each surgical modality used to treat Ewing’s sarcoma has its own challenges and risks of failure or complications. In the current case, tumor resection, reconstruction, rehabilitation, elongation, and rehabilitation within 9 years enabled good recovery of the patient. Corticalization was confirmed on the final radiographic follow-up, and the patient is currently doing well, with good physical function.
The authors are grateful to the patient and his family for consenting to publish the case.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Doski JO, Iraq; Tian YT, China S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Guo W, Xu W, Huvos AG, Healey JH, Feng C. Comparative frequency of bone sarcomas among different racial groups. Chin Med J (Engl). 1999;112:1101-1104. [PubMed] |
| 2. | Hung GY, Horng JL, Yen HJ, Yen CC, Chen WM, Chen PC, Wu HT, Chiou HJ. Incidence patterns of primary bone cancer in taiwan (2003-2010): a population-based study. Ann Surg Oncol. 2014;21:2490-2498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Kennedy JG, Frelinghuysen P, Hoang BH. Ewing sarcoma: current concepts in diagnosis and treatment. Curr Opin Pediatr. 2003;15:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Wilkins RM, Pritchard DJ, Burgert EO Jr, Unni KK. Ewing's sarcoma of bone. Experience with 140 patients. Cancer. 1986;58:2551-2555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Paulussen M, Ahrens S, Dunst J, Winkelmann W, Exner GU, Kotz R, Amann G, Dockhorn-Dworniczak B, Harms D, Müller-Weihrich S, Welte K, Kornhuber B, Janka-Schaub G, Göbel U, Treuner J, Voûte PA, Zoubek A, Gadner H, Jürgens H. Localized Ewing tumor of bone: final results of the cooperative Ewing's Sarcoma Study CESS 86. J Clin Oncol. 2001;19:1818-1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 271] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;106-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 890] [Cited by in RCA: 755] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 7. | Miller BJ, Gao Y, Duchman KR. Does surgery or radiation provide the best overall survival in Ewing's sarcoma? J Surg Oncol. 2017;116:384-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Xu L, Li X, Wang Z, Xiong J, Wang S. Functional evaluation for patients with lower extremity sarcoma: application of the Chinese version of Musculoskeletal Tumor Society scoring system. Health Qual Life Outcomes. 2017;15:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 243] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 10. | Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 189] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Worch J, Matthay KK, Neuhaus J, Goldsby R, DuBois SG. Ethnic and racial differences in patients with Ewing sarcoma. Cancer. 2010;116:983-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Weinstein SL, Dolan LA. Proximal femoral growth disturbance in developmental dysplasia of the hip: what do we know? J Child Orthop. 2018;12:331-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Seu MY, Haley A, Cho BH, Carl HM, Bos TJ, Hassanein AH, Wong AL, Morris CD, Sacks JM. Proximal femur reconstruction using a vascularized fibular epiphysis within a cadaveric femoral allograft in a child with Ewing sarcoma: a case report. Plast Aesthet Res. 2017;4:209-214. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Tsuchiya H, Abdel-Wanis ME, Sakurakichi K, Yamashiro T, Tomita K. Osteosarcoma around the knee. Intraepiphyseal excision and biological reconstruction with distraction osteogenesis. J Bone Joint Surg Br. 2002;84:1162-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Donati F, Di Giacomo G, D'Adamio S, Ziranu A, Careri S, Rosa M, Maccauro G. Silver-Coated Hip Megaprosthesis in Oncological Limb Savage Surgery. Biomed Res Int. 2016;2016:9079041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Abdel Rahman M, Bassiony A, Shalaby H. Reimplantation of the resected tumour-bearing segment after recycling using liquid nitrogen for osteosarcoma. Int Orthop. 2009;33:1365-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Capanna R, Campanacci DA, Belot N, Beltrami G, Manfrini M, Innocenti M, Ceruso M. A new reconstructive technique for intercalary defects of long bones: the association of massive allograft with vascularized fibular autograft. Long-term results and comparison with alternative techniques. Orthop Clin North Am. 2007;38:51-60, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 176] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 18. | Salcedo Cánovas C. Bone elongation using monolateral external fixation: a practical guide. Strategies Trauma Limb Reconstr. 2015;10:175-188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Mizoshiri N, Shirai T, Terauchi R, Tsuchida S, Mori Y, Katsuyama Y, Hayashi D, Oka Y, Kubo T. Limb saving surgery for Ewing's sarcoma of the distal tibia: a case report. BMC Cancer. 2018;18:503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | González-Herranz P, Burgos-Flores J, Ocete-Guzmán JG, López-Mondejar JA, Amaya S. The management of limb-length discrepancies in children after treatment of osteosarcoma and Ewing's sarcoma. J Pediatr Orthop. 1995;15:561-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |