Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7944
Peer-review started: November 22, 2021
First decision: May 11, 2022
Revised: May 19, 2022
Accepted: June 21, 2022
Article in press: June 21, 2022
Published online: August 6, 2022
Processing time: 241 Days and 16.2 Hours
Percutaneous endoscopic lumbar discectomy (PTED) is a procedure that is commonly used to treat lumbar disc herniation and spinal stenosis. Despite its less invasiveness, this surgery is rarely used to treat spinal metastases. Per
A 68-year-old woman presented with low back pain and radicular symptoms. She couldn't straighten her legs because of severe pain. Computed tomography (CT) showed a mass lesion in the lung and bone destruction in the L4 vertebrae. The biopsy of the lung lesion revealed adenocarcinoma and the biopsy for L4 vertebrae revealed metastatic adenocarcinoma. PTED paired with PVP was performed on the patient due to the patient's poor overall physical state and short survival time. Transcatheter arterial embolization of vertebral tumors was performed before surgical resection to reduce excessive blood loss during the operation. The incision was scaled up with the TESSY technology. The pain was obviously relieved following the operation and no serious complications occurred. Postoperative CT showed that the decompression around the nerve root was successful, polymethyl methacrylate filling was satisfactory and the tumor tissue around the nerve root was obviously removed. During the 1-year follow-up period, the patient was in a stable condition.
PTED in combination with PVP is an effective and safe treatment for Lumbar single-level Spinal Column metastases with radicular symptoms. Because of the small sample size and short follow-up time, the long-term clinical efficacy of this method needs to be further confirmed.
Core Tip: Spinal metastatic tumor is a common clinical disease. Because of the poor general condition of patients, minimally invasive treatment is widely used. We present a case of metastatic adenocarcinoma in the L4 vertebrae treated with percutaneous endoscopic lumbar discectomy (PTED) combined with percutaneous vertebroplasty (PVP), with transcatheter arterial embolization of vertebral tumors performed before surgical resection. The therapeutic results were satisfactory. PTED combined with PVP is a safe and effective method for treating Lumbar single-level Spinal Column metastases with radicular symptoms.
- Citation: Ran Q, Li T, Kuang ZP, Guo XH. Percutaneous transforaminal endoscopic decompression combined with percutaneous vertebroplasty in treatment of lumbar vertebral body metastases: A case report. World J Clin Cases 2022; 10(22): 7944-7949
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7944.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7944
As the number of cancer cases increases, the incidence of spinal metastases also increases year by year. Patients suffer from severe low back pain and lower extremity radiating pain due to metastases in the vertebral body[1,2]. Some patients with single vertebral metastases can be treated with open surgery in addition to total bed immobilization and symptomatic pain management. Percutaneous vertebroplasty (PVP) has been widely used in patients who suffer from pain without spinal cord compression and radicular symptoms[3-5]. Percutaneous Transforaminal Endoscopic Decompression (PTED) is rarely reported to be used in spinal metastatic disease. In this report, we introduced and described the surgical technique using PTED combined with PVP in lumbar vertebral body metastases[6,7].
A 68-year-old woman with low back pain and radicular symptoms was unable to straighten her leg due to severe pain.
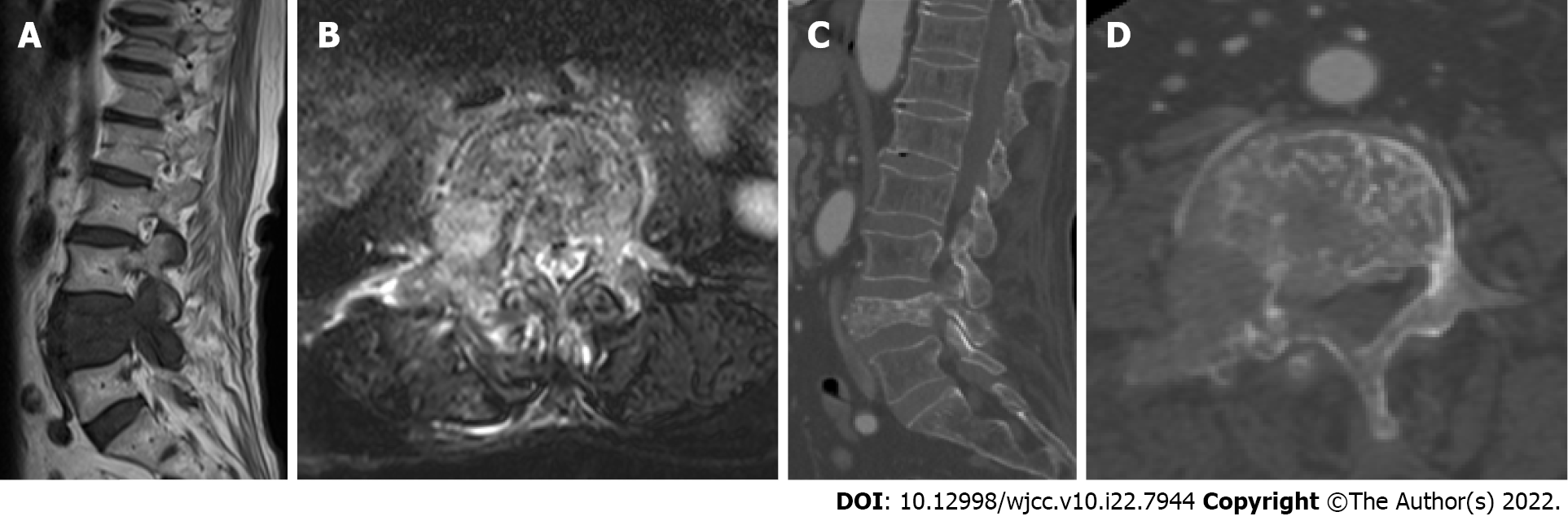
Low back pain and radicular symptoms first appeared 2 wk ago. The Lumbar computed tomography (CT) scan showed a mass lesion in the lung. Lumbar CT and magnetic resonance imaging (MRI) showed metastases in the lumbar vertebral body. The severe radicular symptom could not be relieved by painkillers. Furthermore, this patient could not receive an invasive surgery due to poor general conditions.
Previous medical history revealed no significant illnesses.
Previous medical history revealed no significant illnesses.
Low back tenderness, percussion pain and the straight leg raising test all yielded positive results.
According to cell blood count results, the white blood cell count was increased (10.8 × 109/L) and the hemoglobin level was 157 g/L.
Lumbar CT and MRI showed bone destruction in the L4 vertebrae. MRI revealed that the tumor had invaded the L4 vertebral body and was compressing the nerve root (Figure 1).
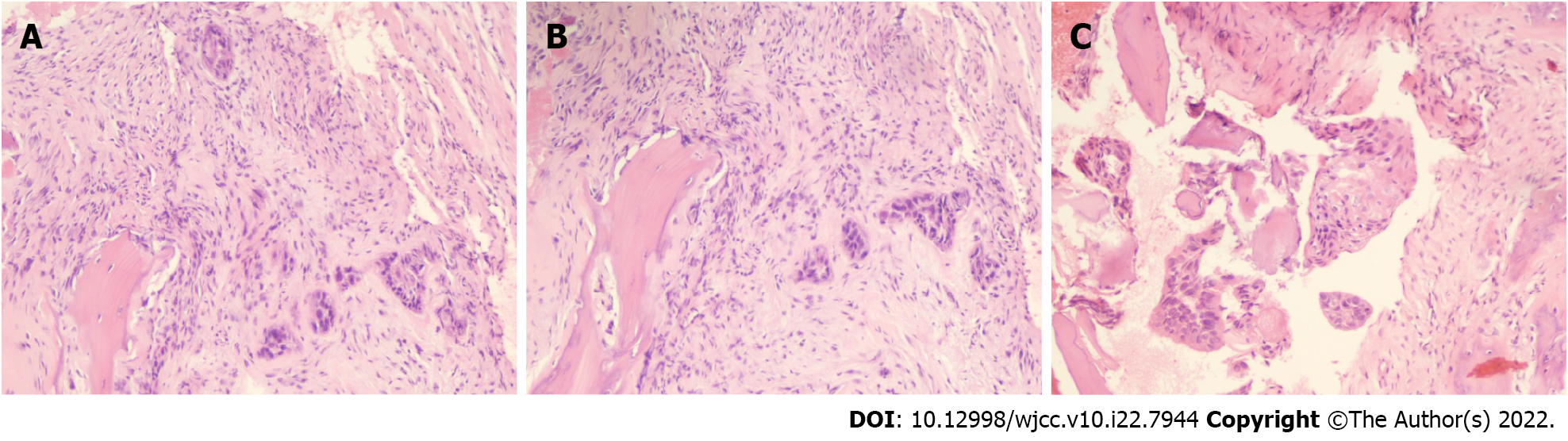
Biopsy and histopathological examination of the L4 vertebrae revealed metastatic adenocarcinoma which probably originated from the lung (Figure 2).
The diagnosis of the presented case was lung cancer with lumbar vertebrae metastasis.
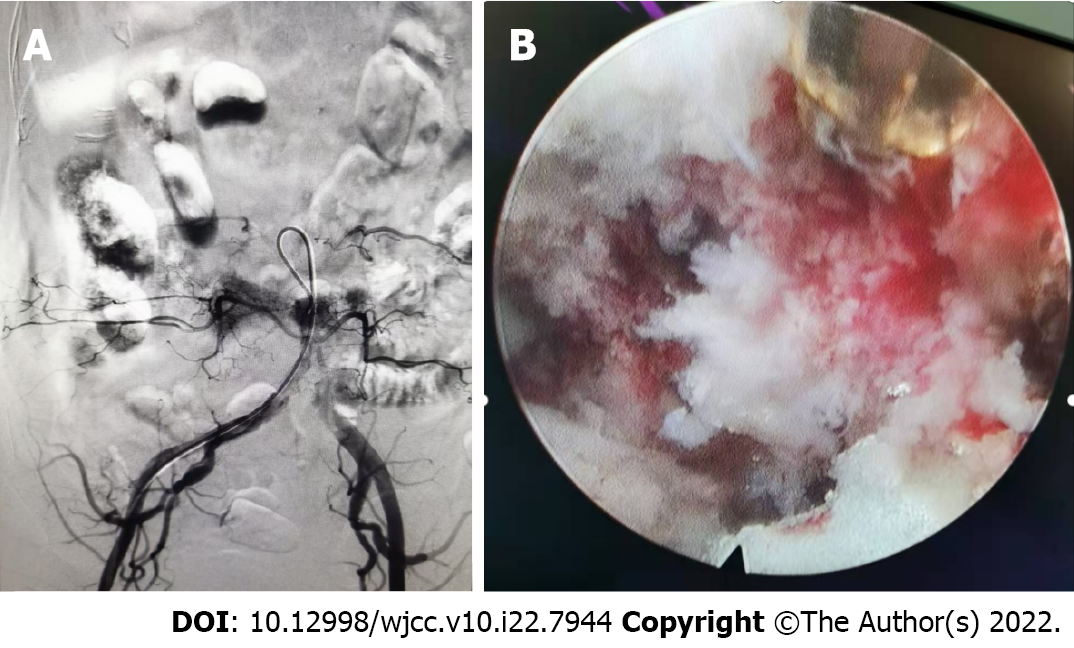
Given the patient's poor general physical condition, a minimally invasive technique was chosen after a multidisciplinary medical staff discussion. The operation plan was PTED combined with PVP under local anesthesia. Transcatheter arterial embolization of vertebral tumors was performed before surgical resection in order to minimize excessive blood loss during the operation (Figure 3A). PVP and PTED were conducted prone on a radiolucent table under local anesthetic. PVP was conducted on both sides of the vertebral body using standard procedures. Because there was no cement leakage, it was confirmed that the patient's radicular symptoms did not worsen after the treatment. The point of entry was 8 cm from the midline. TESSY technology was used to scale up the incision and no obvious bleeding occurred. Endoscopy could observe pathologic fracture fragments and tumor tissue at the rear of the intervertebral space. The tumor invaded the posterior border of the L4 vertebrae and paravertebral tissue compressing the L4 nerve root. The tissues compressing the nerve root were removed carefully with endoscopic forceps and bleeding was coagulated by radiofrequency electrode (Figure 3B).
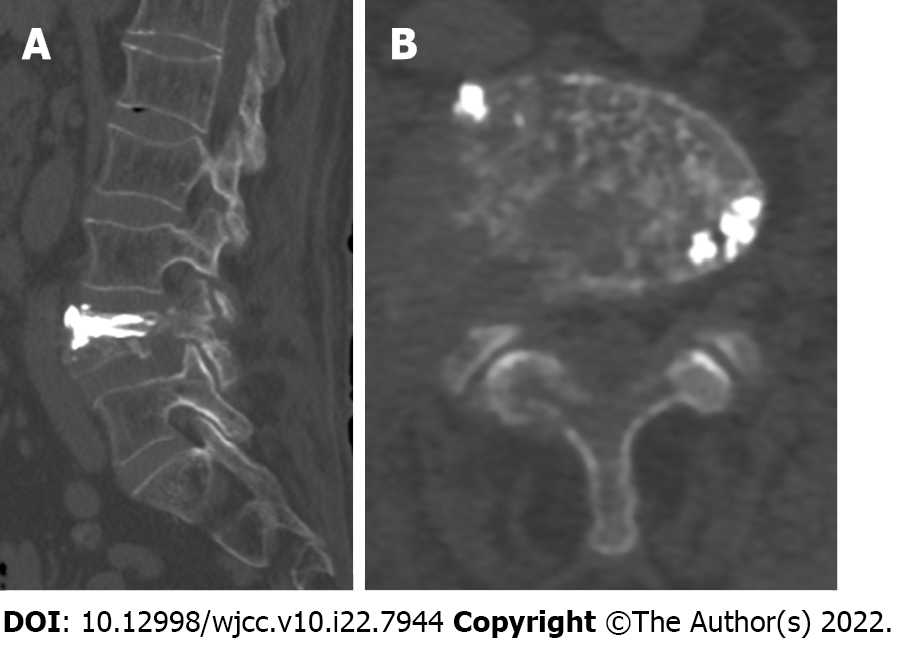
We have completed sufficient decompression of the intervertebral foramen, partial resection of the vertebral body and pedicle of the vertebral arch and exposure of polymethyl methacrylate injected into the vertebral body (Figure 4). The patient's low back pain and radicular symptoms were clearly relieved after the operation. Postoperative CT showed that the decompression around the nerve root was successful. During the 1-year follow-up period, the patient was in a stable condition.
The vertebral body is the most common site among bone metastases accounting for 5.00%-10.00% of patients with malignant tumors[8]. Spinal metastases often present as lesions, site pain and limited mobility[9]. Further progression to spinal canal metastases might result in myeloid or radicular symptoms in some patients. The current treatment options include radiotherapy, chemotherapy and surgery with radiotherapy being the first choice for the majority of patients with spinal metastases[8]. Most patients and their families are hesitant to accept traditional surgical treatment due to the short survival time. In recent years, with the development and maturity of minimally invasive techniques, PVP and PTED have been gradually applied in treating vertebral column metastases[10]. However, PVP is ineffective in treating sciatica patients and decompression of the compressed nerve root is required[11]. In order to remove the tumor thoroughly and reconstruct the stability of the column, total spinal resection should be performed under the condition of ensuring the safety of the spinal cord. In this case, these two procedures were operated alternately. The criterion of complete decompression was that the nerve root could move freely with the changes in irrigation pressure.
Palliative decompression, intralesional resection or marginal resection of the tumor are ineffective when the vertebral body, appendages or the entire column are involved. Compared with traditional open surgery, PTED has the following advantages: (1) The survival time for patients with metastatic tumors in the column is short and their general physical condition is poor. The combined minimally invasive technique is safe and effective so it is easy to be accepted by patients and their families; (2) The symptoms of nerve root compression can be relieved with less trauma, bleeding and operation time; (3) It has a significant impact on vertebral body stability. The incidence of wound infection and complications (e.g., thrombus, infection caused by post-operative incapacitation) were reduced; and (4) This technique will not cause severe damage to the column's normal bone and soft tissue structure while removing the tumor. The pain caused by internal fixation can be relieved.
Because the tumor invaded the nerve root, causing accumulated necrotic bone tissue and crucial adhesion in the nerve root, partial nerve root decompression occurred. Meanwhile, the nerve might be drawn at the same time, resulting in nerve root injury. Even a tiny amount of blood oozing might easily cause an unclear view in the surgical field due to the invaded tumor tissue. In this case, the nerve root could not be completely separated from the surrounding tissue and easily recognized. Because of the complicated anatomic structure and abundant blood supply, the tumors in the vertebral body are often accompanied by unclear views in the surgical field, difficulties in separating surrounding tissue, a large amount of bleeding and a long operation time. Before surgery, arterial embolization can drastically limit the tumor's blood supply, reduce blood loss during the operation, allow for complete resection of the tumor, and increase the operation's success rate. Recent research and advances in technique have reported that preoperative embolization is a safe and effective method of decreasing intraoperative blood loss[12]. However, the authors consider that this procedure is unsuitable for patients with multiple segmental metastases or tumor’s that are spinal canal space-occupying[13].
PTED combined with PVP is a safe and effective method for treating Lumbar single-level Spinal Column metastases with radicular symptoms. Because of the small sample size and short follow-up time, the long-term clinical efficacy of this method needs to be further confirmed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anazawa U, Japan; Naem AA, Syria S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Hariri O, Takayanagi A, Miulli DE, Siddiqi J, Vrionis F. Minimally Invasive Surgical Techniques for Management of Painful Metastatic and Primary Spinal Tumors. Cureus. 2017;9:e1114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Pennington Z, Ahmed AK, Molina CA, Ehresman J, Laufer I, Sciubba DM. Minimally invasive vs conventional spine surgery for vertebral metastases: a systematic review of the evidence. Ann Transl Med. 2018;6:103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 3. | Chen C, Li D, Wang Z, Li T, Liu X, Zhong J. Safety and Efficacy Studies of Vertebroplasty, Kyphoplasty, and Mesh-Container-Plasty for the Treatment of Vertebral Compression Fractures: Preliminary Report. PLoS One. 2016;11:e0151492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Tian QH, Sun XQ, Lu YY, Wang T, Wu CG, Li MH, Cheng YS. Percutaneous Vertebroplasty for Palliative Treatment of Painful Osteoblastic Spinal Metastases: A Single-Center Experience. J Vasc Interv Radiol. 2016;27:1420-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Zhang JJ, Zhou Y, Hu HY, Sun YJ, Wang YG, Gu YF, Wu CG, Shen Z, Yao Y. Safety and efficacy of multilevel vertebroplasty for painful osteolytic spinal metastases: a single-centre experience. Eur Radiol. 2017;27:3436-3442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Wang FA, He SC, Xiao EH, Wang SX, Sun L, Lv PH, Huang WN. Sequential Transarterial Embolization Followed by Percutaneous Vertebroplasty Is Safe and Effective in Pain Management in Vertebral Metastases. Pain Physician. 2016;19:E559-E567. [PubMed] |
| 7. | Gao Z, Wu Z, Lin Y, Zhang P. Percutaneous transforaminal endoscopic decompression in the treatment of spinal metastases: A case report. Medicine (Baltimore). 2019;98:e14819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Miscusi M, Polli FM, Forcato S, Ricciardi L, Frati A, Cimatti M, De Martino L, Ramieri A, Raco A. Comparison of minimally invasive surgery with standard open surgery for vertebral thoracic metastases causing acute myelopathy in patients with short- or mid-term life expectancy: surgical technique and early clinical results. J Neurosurg Spine. 2015;22:518-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 9. | Verlaan JJ, Choi D, Versteeg A, Albert T, Arts M, Balabaud L, Bunger C, Buchowski JM, Chung CK, Coppes MH, Crockard HA, Depreitere B, Fehlings MG, Harrop J, Kawahara N, Kim ES, Lee CS, Leung Y, Liu Z, Martin-Benlloch A, Massicotte EM, Mazel C, Meyer B, Peul W, Quraishi NA, Tokuhashi Y, Tomita K, Ulbricht C, Wang M, Oner FC. Characteristics of Patients Who Survived < 3 Months or > 2 Years After Surgery for Spinal Metastases: Can We Avoid Inappropriate Patient Selection? J Clin Oncol. 2016;34:3054-3061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Uei H, Tokuhashi Y, Maseda M, Nakahashi M, Sawada H, Nakayama E, Soma H. Comparison between minimally invasive spine stabilization with and without posterior decompression for the management of spinal metastases: a retrospective cohort study. J Orthop Surg Res. 2018;13:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Mansoorinasab M, Abdolhoseinpour H. A review and update of vertebral fractures due to metastatic tumors of various sites to the spine: Percutaneous vertebroplasty. Interv Med Appl Sci. 2018;10:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Ma J, Tullius T, Van Ha TG. Update on Preoperative Embolization of Bone Metastases. Semin Intervent Radiol. 2019;36:241-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Uei H, Tokuhashi Y, Oshima M, Maseda M, Matsumoto K, Soma H, Nakayama E, Tachikawa Y. Clinical Results of Minimally Invasive Spine Stabilization for Spinal Metastases. Orthopedics. 2017;40:e693-e698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |