Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7899
Peer-review started: August 24, 2021
First decision: November 17, 2021
Revised: November 26, 2021
Accepted: June 24, 2022
Article in press: June 24, 2022
Published online: August 6, 2022
Processing time: 332 Days and 2 Hours
Non-secretory multiple myeloma (MM) is a rare condition that accounts for only 3% of MM cases and is defined by normal serum and urine immunofixation and a normal serum free light chain ratio. Non-secretory MM with multiple extra
A 36-year-old man presented with progressive facial swelling and nasal congestion with cough. Various imaging studies revealed an endobronchial mass in the left bronchus and a large left maxillary mass with multiple destructive bone metastatic lesions. He initially presented with lung cancer and multiple metastases. However, pathologic reports showed multiple extramedullary plasmacytomas in the left maxilla and the left bronchus. There was no change in the serum and urine monoclonal protein levels, and no abnormalities were observed in laboratory examinations, including hemoglobin, calcium, and creatinine levels. The bone marrow was hypercellular, with 13.49% plasma cells. The patient was diagnosed with non-secretory MM expressed as multiple extramedullary plasmacytomas with endobronchial lesions in a rare location. Radiation therapy for symptomatic lesions with high-dose dexamethasone was started, and the size of the left maxillary sinus lesion dramatically decreased. In the future, chemotherapy will be administered to control lesions in other areas.
We present a rare case of non-secretory MM with multiple extramedullary plasmacytoma with an endobronchial lesion.
Core Tip: Endobronchial and maxillary mass lesions without abnormality on laboratory examination are easily misdiagnosed as metastases of primary lung cancer or other head and neck malignancies. Histopathological studies are required to avoid erroneous diagnoses.
- Citation: Lee SB, Park CY, Lee HJ, Hong R, Kim WS, Park SG. Non-secretory multiple myeloma expressed as multiple extramedullary plasmacytoma with an endobronchial lesion mimicking metastatic cancer: A case report. World J Clin Cases 2022; 10(22): 7899-7905
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7899.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7899
Multiple myeloma (MM) is a mature B cell neoplasm that accounts for 10% of all hematologic malignancies and is defined by the presence of ≥ 10% of clonal plasma cells in the bone marrow or biopsy-proven extramedullary plasmacytoma and the presence of related tissue or organ damage[1]. Symptomatic MM is defined by the presence of a monoclonal protein in the serum or urine, plasma cells in the bone marrow (at least 10%), and presence of related organ disorders (hypercalcemia, renal insufficiency, anemia, and bone lesions)[1,2]. MM is primarily observed in older patients and considered difficult to treat[3]. Over the past decade, the median survival of patients with myeloma has increased with the development of therapeutic agents, including immunomodulatory drugs (thalidomide and lenalidomide) and proteasome inhibitors (bortezomib). High-dose therapy followed by autologous stem cell transplantation (ASCT) has also contributed to this improvement in the survival rate[4].
In most patients, plasma cell proliferation is restricted to the bone marrow. However, in some cases, extramedullary plasma cell proliferation is also observed in other tissues, such as the nasal cavity, lung, and pleura[5]. Endobronchial plasmacytoma has been reported in several cases. Although exceedingly rare, according to published reports, most cases were reported in solitary lesions or advanced MM[6]. Here, we report the first diagnosed case of multiple extramedullary plasmacytoma with endobronchial lesions in non-secretory MM.
A 36-year-old man presented to our hospital for evaluation of progressively worsening facial swelling and nasal congestion. He was initially diagnosed with a nasal polyp with sinusitis and underwent polyp removal with antibiotic therapy.
The patient visited our hospital for further evaluation after redeveloping facial swelling and nasal congestion, this time accompanied by a gradually worsening cough with sputum and blurred vision in the left eye.
The patient had no previous medical history.
The patient is a non-alcoholic and non-smoker. He has no family history.
The patient showed painful facial swelling and blurred vision. The patient's respiratory rate was 22 breaths per minute, blood pressure was p (B) = 15.99/10.7 kPa, and oxygen saturation in room air was 90%.
Based on laboratory findings, the hemoglobin level was 11.9 g/dL (normal range, 12-16 g/dL), and the creatinine level was 0.7 mg/dL (normal range, 0.5-1.3 mg/dL). Monoclonal proteins could not be detected by serum and urine protein immunofixation electrophoresis. The albumin level was 3.77 g/dL (normal range, 3.5-5.5 g/dL) and beta-2-microglobulin level was 4.2 mg/L (normal range, 0.0-2.4 mg/L). The lactate dehydrogenase level was 271 U/L (normal range, 125-220 U/L).
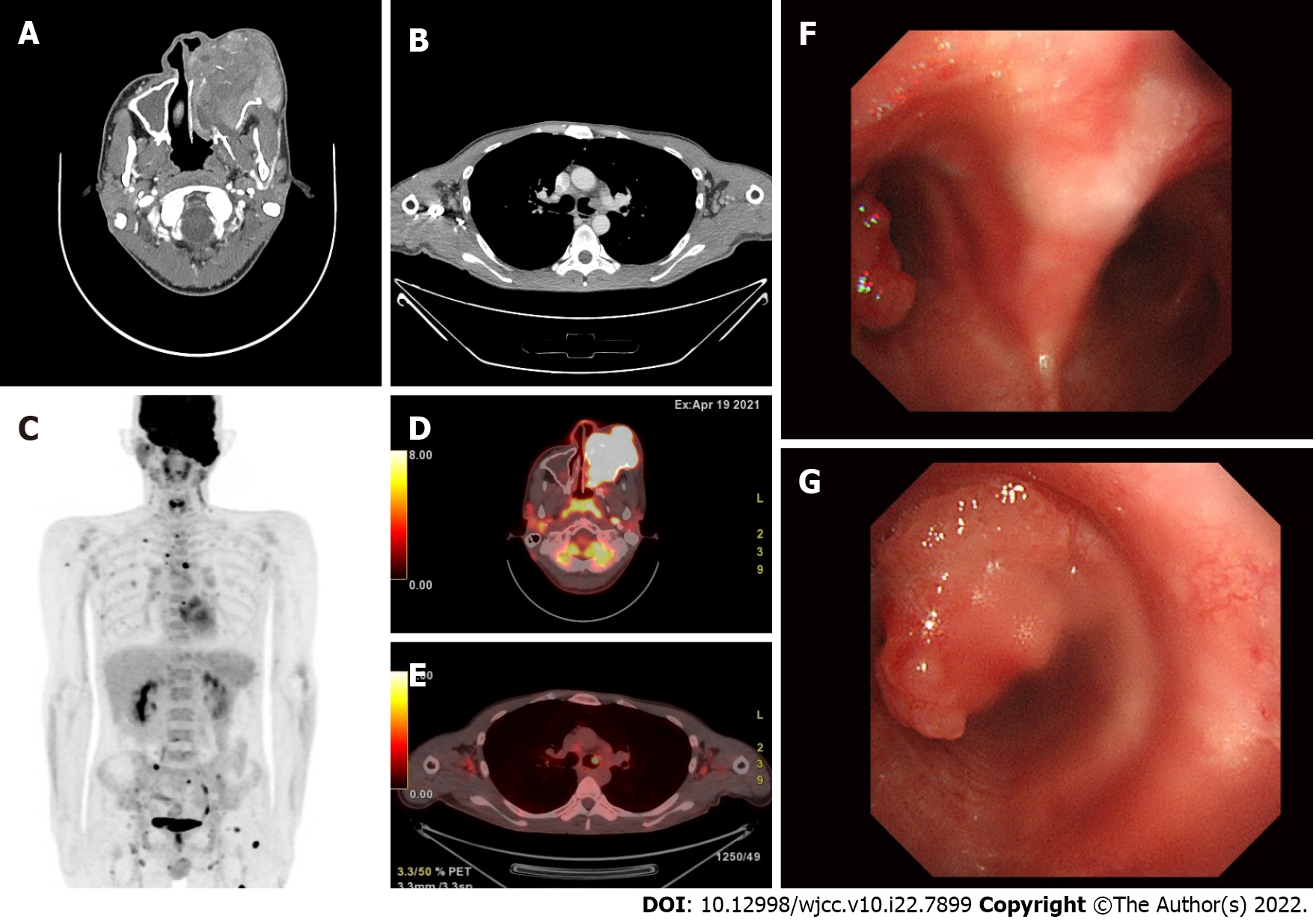
Computed tomography of the neck and thorax revealed a solid mass occupying the left maxillary sinus and an endobronchial lesion in the left main bronchus (Figure 1).
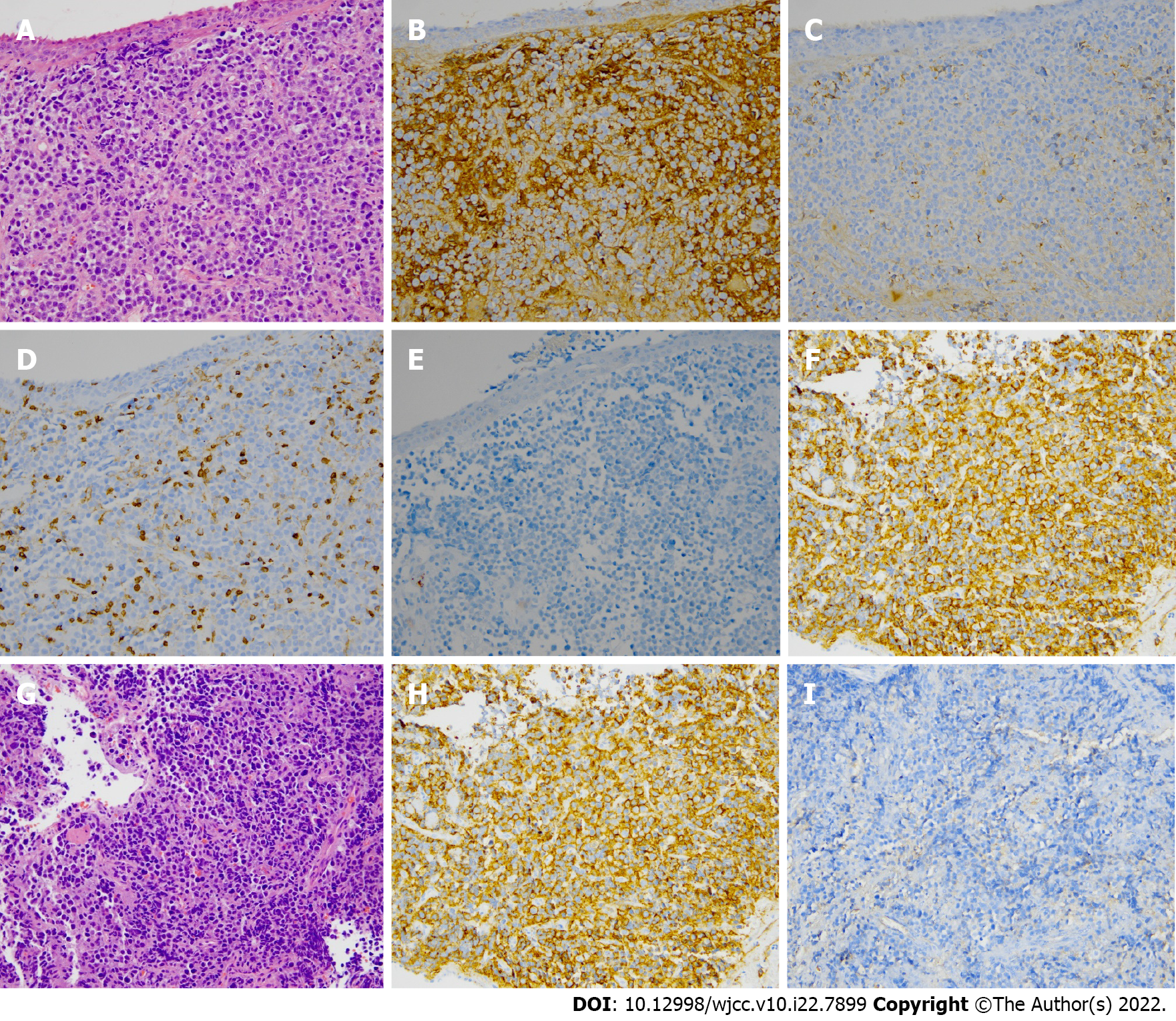
Positron emission tomography/computed tomography revealed a hypermetabolic mass in the left maxillary sinus extending to the left ethmoid sinus and nasal cavity and multiple hypermetabolic metastatic nodules in both the cervical and left supraclavicular areas. Multiple hypermetabolic osseous metastases had spread to the sternum, ribs, right scapula, right humerus, thoraxic and lumbar spines, pelvic bone, and left femur. Focal hypermetabolic nodular lesions in the left main bronchus were also observed (Figure 1). Primary lung cancer with multiple bone metastases was initially suspected, but double primary lung cancer with maxillary sinus cancer was excluded. We immediately performed a pathologic examination of the maxillary sinus mass and the endobronchial mass using bronchoscopy. Bronchoscopic findings showed a 1.5-cm protruding mass with pedicles arising from the anterior wall of the left proximal main bronchus (Figure 1), which was suspected to be primary lung cancer. Initially, the maxillary mass had pathologic findings of monomorphic plasmacytoid cytoplasm (positive for CD138, kappa light chain, and negative for CD3, CD20, and lambda light chain) (Figure 2), and it was subsequently diagnosed as a plasmacytoma, which was confirmed by the bronchoscopic biopsy result (Figure 2).
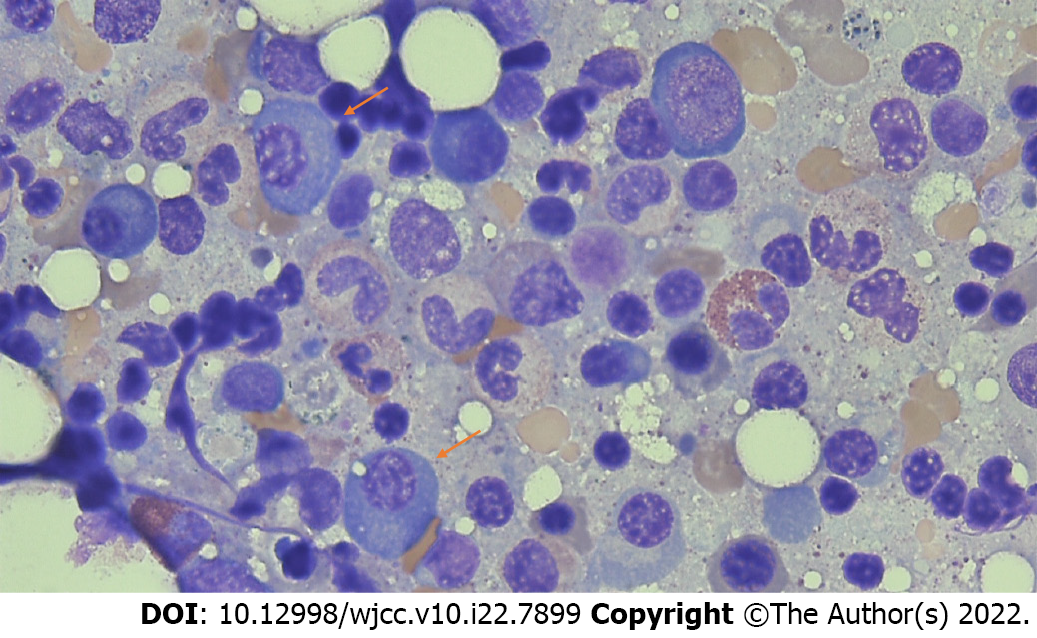
The patient was referred to the hematology department to undergo an evaluation for systemic MM. Biochemical tests revealed normal calcium and creatinine levels, and serum and urine immunofixation were negative for monoclonal proteins. However, the bone marrow biopsy from the iliac crest showed hypercellularity for his age with diffusely infiltrated plasma cells (13.49%) (Figure 3). Although the patient had no anemia and the serum creatinine levels were normal, a diagnosis of non-secretory MM was considered based on the bone marrow biopsy findings and the multiple lesions, including confirmation of the maxillary sinus and endobronchial lesions as plasmacytoma.
The patient was finally diagnosed with non-secretory MM, expressed as multiple extramedullary plasmacytomas with an endobronchial lesion. The International Staging System stage at the time of diagnosis was II.
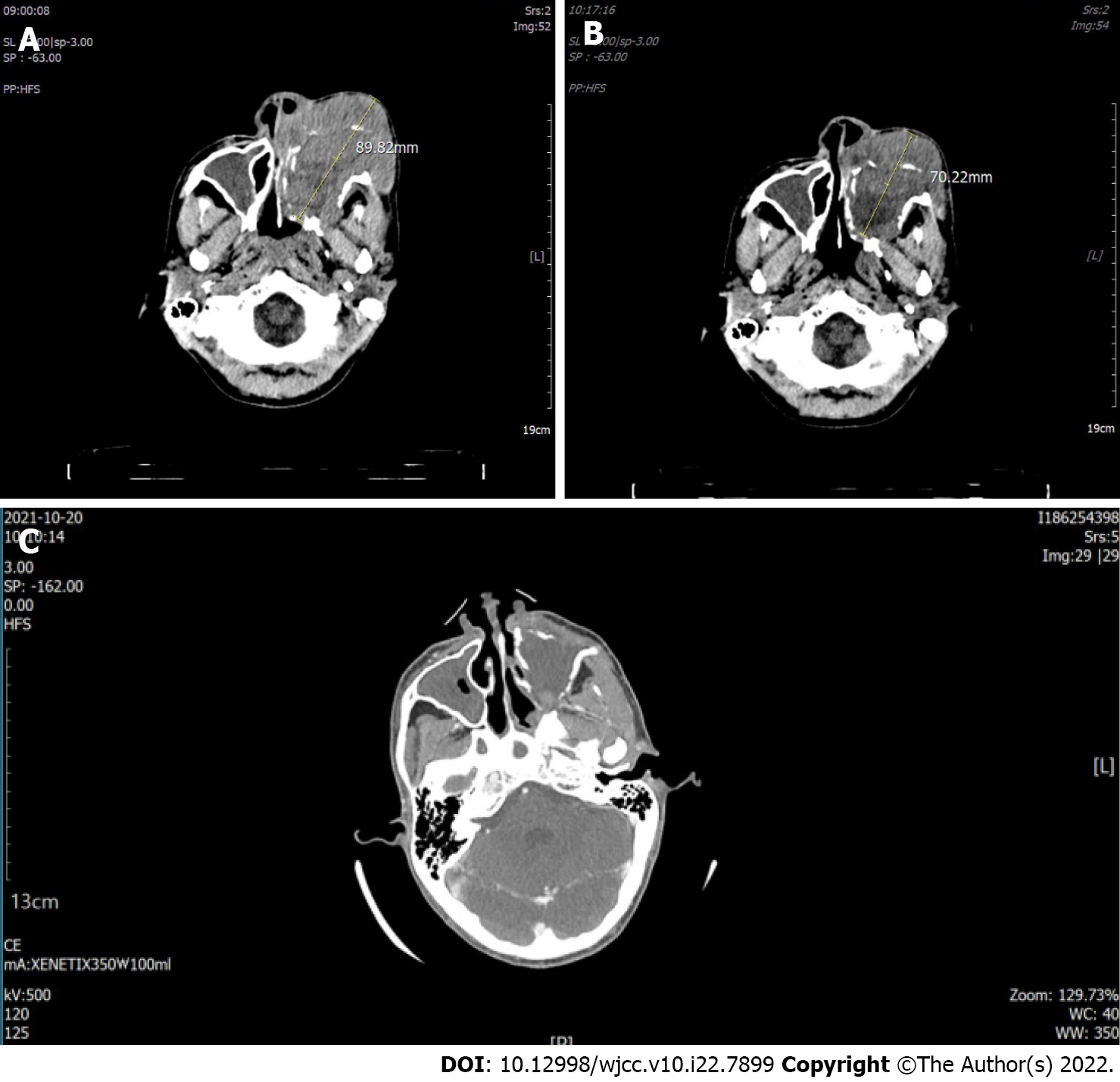
The left maxillary sinus mass extended to the nasopharynx and left ethmoid sinus, which had caused severe facial edema and blurred vision in the left eye. Moreover, endobronchial lesions also caused severe respiratory distress symptoms. Therefore, we started high-dose steroid therapy with dexamethasone 40 mg for 4 days. Palliative radiation therapy of the left maxillary sinus lesion was performed simultaneously. After steroid administration, facial edema dramatically decreased, and respiratory distress symptoms improved (Figure 4). We continued radiation therapy on the sym
Finally, the facial mass and symptoms almost regressed, and the patient will subsequently undergo chemotherapy with bortezomib, thalidomide, and dexamethasone, followed by ASCT.
In the initial stage of diagnosis, our patient was strongly considered as having primary lung cancer with multiple bone metastases or double primary lung cancer with maxillary sinus cancer. Our patient's laboratory tests showed normal results. For this reason, we excluded the possibility of plasmacytoma or non-secretory MM. However, the biopsy confirmed an extramedullary plasmacytoma. In addition, bone marrow examination showed more than 10% plasma cell infiltration without alterations in serum or urine paraprotein and immunoglobin subtype. Thus, we diagnosed the patient with non-secretory MM based on bone marrow examination and biopsy results.
Extramedullary plasmacytoma is a variant of a plasma cell tumor involving organs outside the bone marrow without any sign of systemic involvement (primary solitary plasmacytoma) or secondary to MM[7]. The differential diagnosis of plasma cell dyscrasias is vital because these diseases may exhibit diverse clinical courses and prognoses. Extramedullary plasmacytoma is most often located in the upper respiratory tract and nasopharynx, and involvement of the lower respiratory tract is rarely observed[8]. Endobronchial plasmacytoma is a rare manifestation of extramedullary plasmacytoma[6], with very few cases reported in the literature. Most endobronchial plasmacytoma cases were solitary plasmacytomas with no systemic involvement of MM[9-12]. Our patient showed systemic involvement of a plasma cell malignancy.
Extramedullary plasmacytoma is associated with adverse prognoses in patients with newly diagnosed and relapsing MM[13]. Almost all patients show multiple extramedullary plasmacytomas as the terminal event of their MM[13,14], whereas this patient showed multiple extramedullary plasmacytomas at the initial diagnosis of MM.
Non-secretory MM is a rare variant that accounts for 1%-5% of all cases of MM. It is characterized by the absence of monoclonal gammopathy in the serum and urine[15]. In this case, monoclonal gammopathy was not observed, and there was no organ dysfunction. Due to the inability to detect monoclonal proteins, it is difficult to establish an accurate diagnosis, and misdiagnosis of this condition as a solitary plasmacytoma delays systemic treatment[16,17].
Initially, this patient was diagnosed with primary lung cancer with multiple metastases because there was no reversal of the A/G ratio or increase in serum monoclonal protein levels. However, bone marrow and tissue biopsy results showed systemic involvement of MM. Thus, we present a case of non-secretory MM expressed as multiple extramedullary plasmacytoma with an endobronchial lesion.
Such cases are extremely rare and can be easily misdiagnosed as solid cancers of the upper respiratory tract until histologic confirmation. These clinical situations are extraordinarily heterogeneous, and care must be taken before making a diagnosis. These cases should be considered as having high-risk myeloma systemic involvement and treated appropriately.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Hematology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sueyasu T, Japan S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Kumar SK, Callander NS, Adekola K, Anderson L, Baljevic M, Campagnaro E, Castillo JJ, Chandler JC, Costello C, Efebera Y, Faiman M, Garfall A, Godby K, Hillengass J, Holmberg L, Htut M, Huff CA, Kang Y, Hultcrantz M, Larson S, Liedtke M, Martin T, Omel J, Shain K, Sborov D, Stockerl-Goldstein K, Weber D, Keller J, Kumar R. Multiple Myeloma, Version 3.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:1685-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 137] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 2. | Touzeau C, Moreau P. How I treat extramedullary myeloma. Blood. 2016;127:971-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 3. | Dimopoulos MA, Moreau P, Terpos E, Mateos MV, Zweegman S, Cook G, Delforge M, Hájek R, Schjesvold F, Cavo M, Goldschmidt H, Facon T, Einsele H, Boccadoro M, San-Miguel J, Sonneveld P, Mey U; EHA Guidelines Committee. Multiple myeloma: EHA-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2021;32:309-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 447] [Article Influence: 111.8] [Reference Citation Analysis (0)] |
| 4. | Nooka AK, Kastritis E, Dimopoulos MA, Lonial S. Treatment options for relapsed and refractory multiple myeloma. Blood. 2015;125:3085-3099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 133] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 5. | Bladé J, Fernández de Larrea C, Rosiñol L, Cibeira MT, Jiménez R, Powles R. Soft-tissue plasmacytomas in multiple myeloma: incidence, mechanisms of extramedullary spread, and treatment approach. J Clin Oncol. 2011;29:3805-3812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 258] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 6. | Sunnetcioglu A, Ekin S, Bayram I, Ekinci O, Bugday IB. Endobronchial plasmacytoma in patient with multiple myeloma. Clin Respir J. 2017;11(6):1057-1059. |
| 7. | Khan UZ, Masroor M, Yang W, Riaz M, Liu H. Solitary extramedullary plasmacytoma presenting as an adrenal tumor: case report and literature review. Gland Surg. 2021;10:1158-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Naymagon L, Abdul-Hay M. Primary extramedullary plasmacytoma with diffuse lymph node involvement: a case report and review of the literature. J Med Case Rep. 2019;13:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Fernández-Bussy S, Labarca G, Folch E, Majid A. Extramedullary endobronchial plasmacytoma. BMJ Case Rep. 2013;2013. [PubMed] |
| 10. | Maqsood U, Jones H, Gey van Pittius D, Haris M. Primary pulmonary plasmacytoma mimicking lung cancer diagnosed on endobronchial ultrasound (EBUS)-guided biopsy. BMJ Case Rep. 2016;2016. [PubMed] |
| 11. | Park JI, Lee YY, Lee SS, Ahn JH. A rare case of primary solitary endobronchial plasmacytoma. Thorac Cancer. 2021;12:958-961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Wei S, Li X, Song Z, Zhao H, Qiu X, Gong L, Chen J, Zhou Q. Primary endobronchial plasmacytoma involving local lymph nodes and presenting with rare immunoglobulin G lambda monoclonal gammopathy. Can Respir J. 2012;19:e28-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Nangia JR, Lakhani AA, Loew JM, Gregory SA. Multiple myeloma with multiple extramedullary plasmacytomas. Clin Adv Hematol Oncol. 2011;9:630-632. [PubMed] |
| 14. | Yoon YH, Cho WI, Seo SJ. Case of multiple myeloma associated with extramedullary cutaneous plasmacytoma and pyoderma gangrenosum. Int J Dermatol. 2006;45:594-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Dupuis MM, Tuchman SA. Non-secretory multiple myeloma: from biology to clinical management. Onco Targets Ther. 2016;9:7583-7590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 16. | Low SF, Mohd Tap NH, Kew TY, Ngiu CS, Sridharan R. Non Secretory Multiple Myeloma With Extensive Extramedullary Plasmacytoma: A Diagnostic Dilemma. Iran J Radiol. 2015;12:e11760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Corso A, Mangiacavalli S. Non-Secretory Myeloma: Ready for a new Definition? Mediterr J Hematol Infect Dis. 2017;9:e2017053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |