Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7883
Peer-review started: June 5, 2021
First decision: July 15, 2021
Revised: July 24, 2021
Accepted: May 16, 2022
Article in press: May 16, 2022
Published online: August 6, 2022
Processing time: 412 Days and 1.1 Hours
Rectal mature teratoma is rare and has been reported as a case report in this study. Herein, clinical presentation, magnetic resonance imaging findings, and immunohistochemistry showed a pelvic rectal mature teratoma. The case report and the surgical treatment procedure have been discussed below.
A 29-year-old Chinese female showed up with over a 1-mo history of perianal mass that emerged after defecation. Physical examination indicated that the mass was 4 cm × 3 cm × 3 cm. The intraoperative procedure involved ligation of the sigmoid colon 10 cm above the upper edge of the tumor, followed by ligation of the rectum 3.5 cm above the upper edge of the tumor, and subsequent complete removal of the mass. The histopathology confirmed the mature teratoma.
The tumor can be completely removed using surgery to prevent its recurrence.
Core Tip: Herein, a rectal mature teratoma patient was reported. However, only a few similar cases have been reported. Currently, it is difficult to diagnose mature rectal teratoma using a computed tomography scan. However, complete removal of the tumor using surgery can prevent its recurrence.
- Citation: Liu JL, Sun PL. Rectal mature teratoma: A case report. World J Clin Cases 2022; 10(22): 7883-7889
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7883.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7883
Teratoma is a tumor caused by pluripotent cells, especially the embryonic stem or seed cells in the gonad or embryonic part of the body. It occurs in the midline or on both sides of the body. It often originates from the Hensen’s node, the location of pluripotent stem cells. Teratoma also occurs in the sacral region where pluripotent cells are located[1]. Teratoma is mostly benign with low malignant potential, but it can also develop into a malignancy[2]. Rectal teratoma is rare, and there are few reports worldwide. Mature teratoma is a benign tumor (dermoid cyst) and accounts for over 95% of teratomas. Mature teratoma mostly occurs in women of childbearing age and sometimes in young girls and postmenopausal women. It rarely occurs in males[3]. This study aimed to review the diagnosis and treatment of rectal teratoma and to determine the clinical characteristics associated with this rare tumor.
A 29-year-old female, G1P0, with over a 1-mo history of a perianal mass that emerged after defecation, was hospitalized in the First Affiliated Hospital of Guangxi Chinese Medicine University.
She reported a 1-mo medical history of perianal mass that emerged after defecation and complained about the anal bulge. The patient had not used contraceptives, was not injured, had no pain, chills, or fever, and no difficulty during defecation.
The patient had no past illness.
The patient had a history of artificial abortion and no family history of rectal mature teratoma. The condition was diagnosed as a rectal mass (nature to be investigated).
The mass was 4 cm × 3 cm × 3 cm inside the anus with a dentate line distance of about 6 cm and was smooth upon palliation. A non-tender mass was seen outside the anus.
Hematological examinations, including serum electrolyte levels, human chorionic gonadotropin, comprehensive metabolic panel, and complete blood count, were normal.
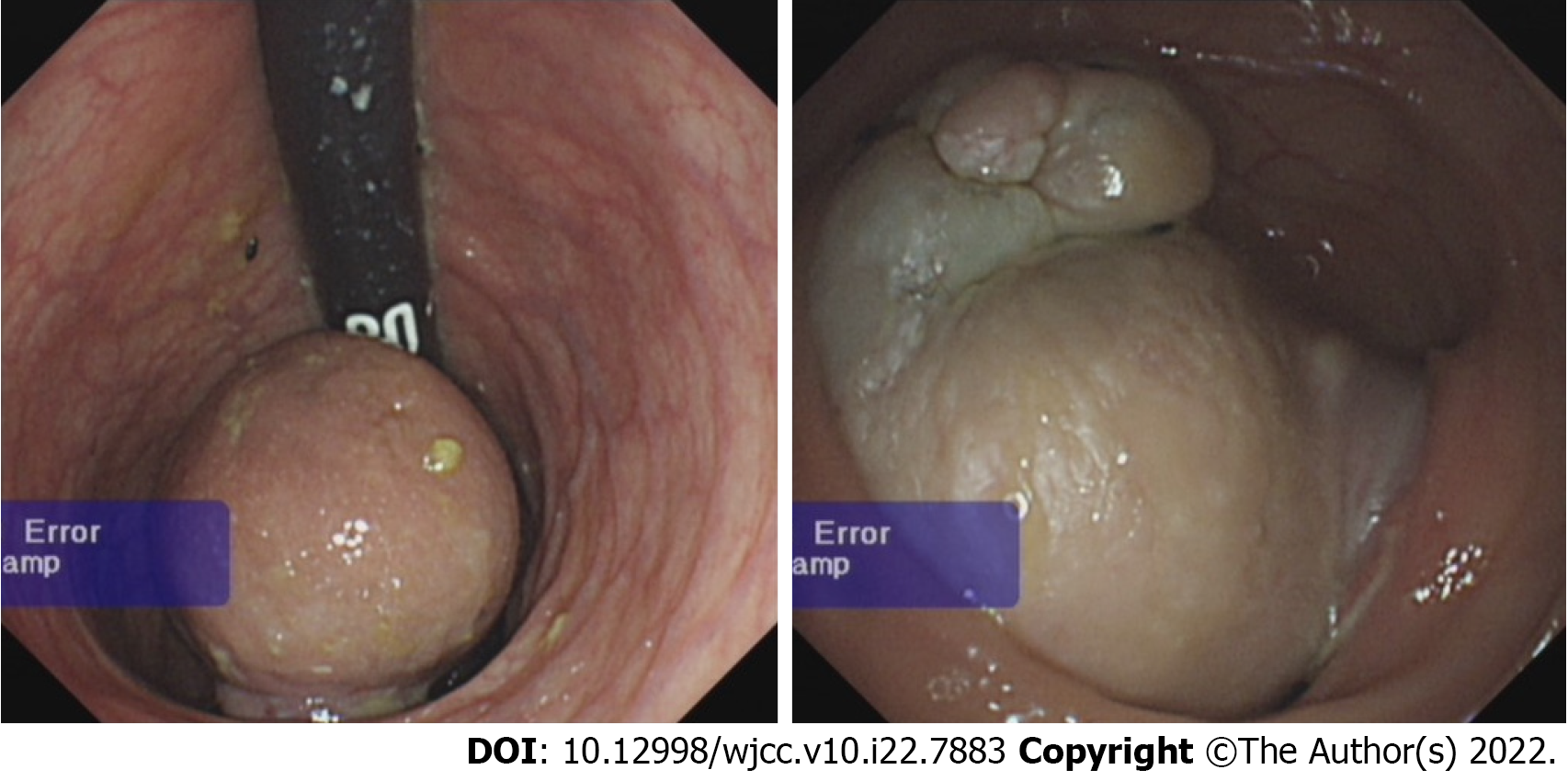
Electronic colonoscopy: Rectal mass (nature to be investigated) (Figure 1).
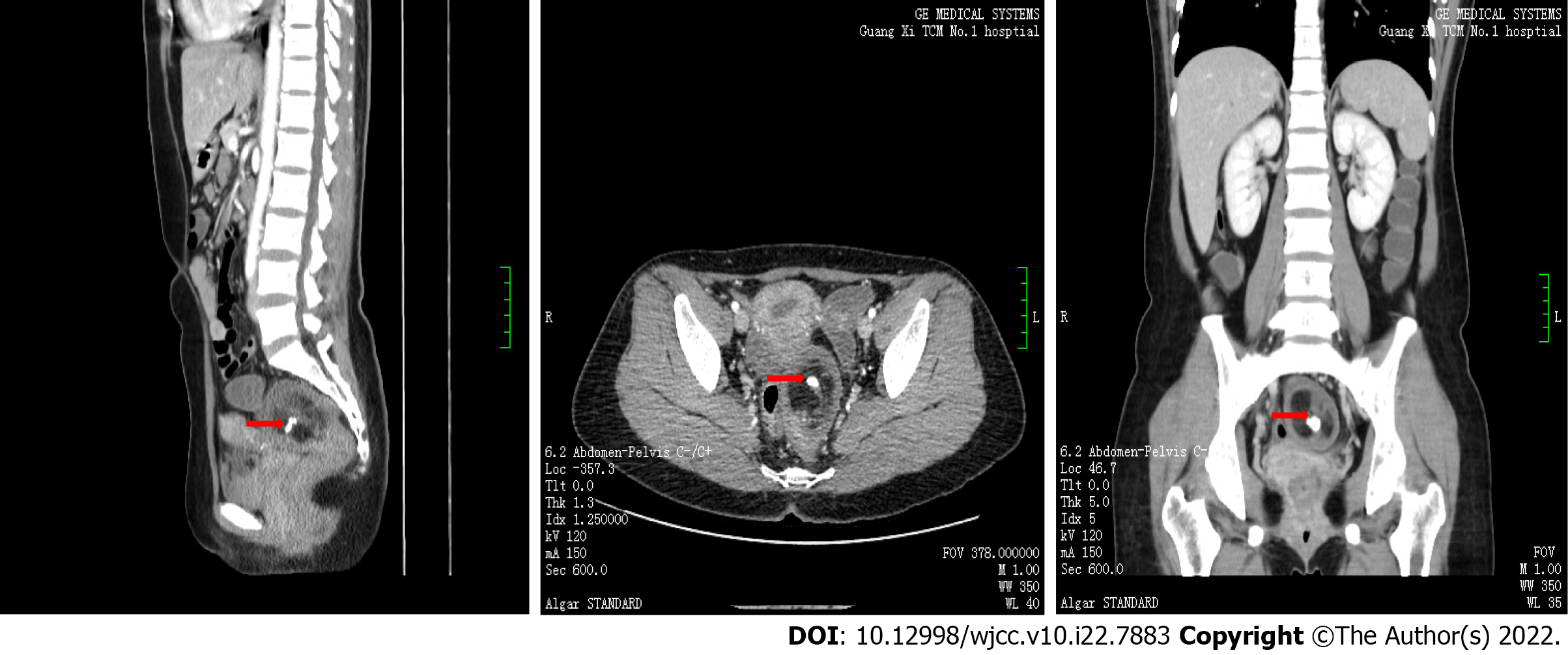
The computed tomography (CT) scan revealed: (1) A 6.3 cm × 4.7 cm × 5.1 cm round mass, flaky low-density shadow and calcification on center, enhanced scanning lesions with circular mild enhancement, non-enhancement on center, and clear boundary on the pelvis (unclear if this is a teratoma); and (2) Double-sided adnexal area low-density shadow (cyst) (Figure 2).
A rectal mass resection was performed via laparoscopy under anesthesia to alleviate the patient’s symptoms.
The condition was diagnosed as mature rectal teratoma based on the above physical examinations and imaging data.
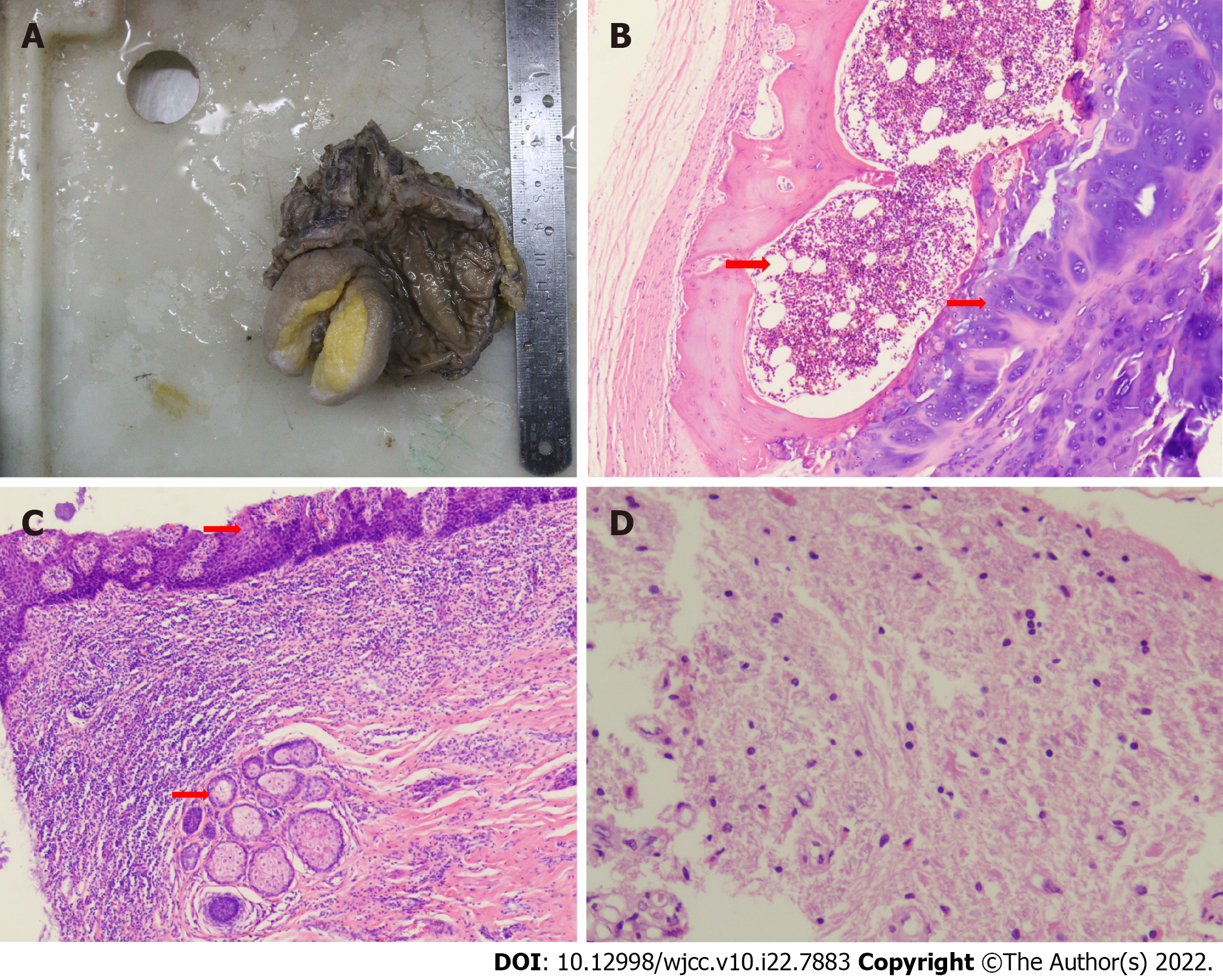
A rectal mass resection was conducted via laparoscopy under anesthesia. Intraoperative ligation was conducted on the sigmoid colon 10 cm above the upper edge of the tumor and on the rectal area 3.5 cm above the upper edge of the tumor, followed by complete removal of the mass. Full hemostasis, sigmoid colon and rectal suture repair, placement of a negative pressure drainage tube in the anus and abdominal cavity, and layer-by-layer suture repair of the incision was then conducted (Figure 3).
In the intestinal section, two connected tumors, about 6 cm × 5 cm × 4 cm and 2 cm × 2 cm × 2 cm, were seen in the intestinal mucosa and intestinal serosal layer, respectively. In the microscopic view, skin and appendages, glands, fat, bone tissue, bone marrow tissue, and brain tissue indicated mature teratoma. No tumor tissue was seen at the two ends (upper and lower margins) after the examination. Six lymph nodes were found, and no tumor metastasis was identified (0/6). Therefore, the condition was diag
Postoperatively, the patient was discharged after healing. She returned for a follow-up in August 2018. On examination, there was evident wound healing and no tumor recurrence. Additionally, the patient was free of discomfort, pain, and fecal incontinence.
The colonoscopy and CT scan revealed a rectal mass, 6 cm × 5 cm × 4 cm in the intestinal mucosa and 2 cm × 2 cm × 2 cm in the intestinal serosal layer, which was diagnosed as mature rectal teratoma. Laparoscopic tumor resection was conducted to remove the tumor. No tumor metastasis was found 6 mo after successful 1-mo treatment. The teratoma was located in the rectal wall, which is close to the pelvic cavity. The teratoma volume increases and breaks into the intestinal wall, and bulging occurs to the posterior wall of the rectum. The teratoma then comes out of the anus and can only be returned by hand.
Clinical reports of teratoma are common in the sacrococcygeal, appendix, ovary, testis, retroperitoneum, mediastinum, etc. Several studies have shown that the incidence of teratoma may be related to various factors, such as genetic, environmental, and gene-level regulation[4,5]. Teratoma can be divided into benign and malignant transformations based on the degree of tissue differentiation. Teratoma incidence is about 1:35000-1:40000[6] and mostly occurs in women (the ratio of male to female is about 1:2-4) with few occurrences in children and postmenopausal women[7,8]. Although mostly reported in the ovary and testis, it also occurs in the midline of the mediastinum, appendix, sacrococcygeal, pineal body, mediastinum, posterior peritoneal cavity, omentum, uterine rectum, vagina, and cervix[9-12]. Immature teratomas occur in adolescents. Most malignancies transform into cancer (squamous cell carcinoma). About 1%-2% of teratoma cases are malignant and are common in young women (the average age of onset is 11 years to 19 years) with poor prognosis[13-15]. CT images of mature teratoma reveal calcification, adipose tissue, bone, tooth, and obviously cysts[16,17].
CT scan is sensitive to calcification and fat, common and quick, and combined with enhanced scan can evaluate the soft tissue composition well. However, it lacks specificity for differentiating between tumor types. While magnetic resonance imaging has a higher resolution of fat and soft tissue, which helps to determine the retrorectal tumors and their relationships to surrounding structures and cystic degeneration, but it poorly shows calcification[18,19]. To some extent, magnetic resonance imaging is more accurate than CT to estimate the possible complications such as torsion, rupture, and malignant transformation.
Badmos et al[20] reported that laparoscopic surgery can enlarge the field of view, reducing the incision and intraoperative blood loss. Lee et al[21] also reported that laparoscopic surgery could significantly reduce the body’s inflammatory response compared to open surgery. Chansoon et al[22] reported a case of complicated duodenal mature teratoma, which was resected via laparoscopic surgery. Herein, the mature cystic teratoma was identified, and the patient was discharged after the operation. No recurrence occurred after 6 mo of follow-up. Laparoscopic pelvic and teratogenic teratoma surgery is widely used because of the minimally invasive advantages. Laparoscopic surgery completely removes the tumor without damaging adjacent tissues and organs, avoiding the rupture of the tumor and preventing leakage of the teratoma, thus inhibiting malignant transformation, recurrence, and meta
Murdock and Abbas[25] reported that an anorectal cystic teratoma transabdominal approach is necessary, which can be done laparoscopically safely and successfully, even for a large lesion. Wang et al[26] reported that it is generally not recommended to use preoperative biopsy of retrorectal tumors because of the risk of infection or tumor seeding in the pelvis. As such, a definitive diagnosis is best obtained by following complete resection of the tumor. Resection of retrorectal teratoma is generally regarded as appropriate because of the malignant potential.
Aiken et al[27] reported that the diagnosis can be made with endoscopy alone by the presence of hair over the mass. Nam and Kim[28] reported that the mass was removed by polypectomy because the patient’s lesion was a pedunculate polyp measuring approximately 4 cm and located approximately 15 cm from the anus. Endoscopic resection was performed to make a diagnosis. Endoscopic resection is indicated for a pedunculate polyp that measures < 4 cm. If the diagnosis is unclear or malignancy cannot be excluded, surgical resection is preferable. The summaries of reported cases of rectal mature teratoma are shown in Table 1.
| Ref. | Year | Age/sex | Symptoms | Previous history | Method | Final diagnosis |
| Murdock and Abbas[25] | 2010 | 26/female | Right-sided pelvic pain radiating down her lower extremities | Transanal drainage of a presumed presacral abscess | Laparoscopic abdomino-paracoccygeal resection | Anorectal cystic teratoma |
| Wang et al[26] | 2019 | 44/female | Submucosal rectal mass | Not described | Laparoscopic tumor resection | Mature retrorectal teratoma |
| Aiken et al[27] | 2020 | 47/female | Bleeding from the rectum for 10 d | Not described | Partial resection of the rectum | Rectum mature teratoma |
| Nam and Kim[28] | 2021 | 68/female | Hematochezia | Not described | Polypectomy | Primary mature teratoma of the rectum |
| Our case | 2021 | 29/female | Perianal mass that emerged after defecation | Not described | Laparoscopic | Rectal mature teratoma |
Rectal teratoma remains a rare disease despite a recent uptick in diagnoses. Radiological imaging is helpful to preoperative diagnosis and planning. Complete surgical excision is the treatment of choice, and regular follow-up after surgery is needed to prevent recurrence. The prognosis of mature teratomas is excellent, and we report this case to raise awareness of this disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Nakaji K, Japan; Ohta H, Japan S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Yoon HM, Byeon SJ, Hwang JY, Kim JR, Jung AY, Lee JS, Yoon HK, Cho YA. Sacrococcygeal teratomas in newborns: a comprehensive review for the radiologists. Acta Radiol. 2018;59:236-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Gatcombe HG, Assikis V, Kooby D, Johnstone PA. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004;86:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 146] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Patel MD, Feldstein VA, Lipson SD, Chen DC, Filly RA. Cystic teratomas of the ovary: diagnostic value of sonography. AJR Am J Roentgenol. 1998;171:1061-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 98] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Prener A, Engholm G, Jensen OM. Genital anomalies and risk for testicular cancer in Danish men. Epidemiology. 1996;7:14-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Kuczyk MA, Serth J, Bokemeyer C, Jonassen J, Machtens S, Werner M, Jonas U. Alterations of the p53 tumor suppressor gene in carcinoma in situ of the testis. Cancer. 1996;78:1958-1966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Frazier AL, Weldon C, Amatruda J. Fetal and neonatal germ cell tumors. Semin Fetal Neonatal Med. 2012;17:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Altman RP, Randolph JG, Lilly JR. Sacrococcygeal teratoma: American Academy of Pediatrics Surgical Section Survey-1973. J Pediatr Surg. 1974;9:389-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 510] [Cited by in RCA: 422] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Peterson CM, Buckley C, Holley S, Menias CO. Teratomas: a multimodality review. Curr Probl Diagn Radiol. 2012;41:210-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Hegde P. Extragonadal omental teratoma: a case report. J Obstet Gynaecol Res. 2014;40:618-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Tokunaga M, Seta M, Yamada M, Nishio M, Yamamoto K, Koyasu Y. Coexistent dermoid cysts of the pouch of the Douglas and ovary resected by laparoscopy. Asian J Endosc Surg. 2012;5:31-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Koo YJ, Im KS, Jung HJ, Kwon YS. Mature cystic teratoma of the uterosacral ligament successfully treated with laparoendoscopic single-site surgery. Taiwan J Obstet Gynecol. 2012;51:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Makni A, Ben Rhouma S, Farah J, Jouini M, Kacem M, Ben Safta Z. A case of mature teratoma of the Douglas. Tunis Med. 2013;91:473-474. [PubMed] |
| 13. | Hackethal A, Brueggmann D, Bohlmann MK, Franke FE, Tinneberg HR, Münstedt K. Squamous-cell carcinoma in mature cystic teratoma of the ovary: systematic review and analysis of published data. Lancet Oncol. 2008;9:1173-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 203] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 14. | Lu Z, Chen J. Introduction of WHO classification of tumours of female reproductive organs, fourth edition. Zhonghua Bing Li Xue Za Zhi. 2014;43:649-650. [PubMed] |
| 15. | Farghaly SA. Current diagnosis and management of ovarian cysts. Clin Exp Obstet Gynecol. 2014;41:609-612. [PubMed] |
| 16. | Asano T, Kawakami S, Okuno T, Tsujii T, Nemoto T, Kageyama Y, Kihara K. Malignant transformation in a mature testicular teratoma left untreated for more than 50 years since childhood. Scand J Urol Nephrol. 2003;37:177-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Reis F, Faria AV, Zanardi VA, Menezes JR, Cendes F, Queiroz LS. Neuroimaging in pineal tumors. J Neuroimaging. 2006;16:52-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Sogni P, Chaussade S, Mosnier H, Abecassis JP, Bonnichon P, Louvel A, Couturier D, Guerre J. Retrorectal tumor in adults. Combination of computed tomography and endorectal echography. Gastroenterol Clin Biol. 1990;14:501-503. [PubMed] |
| 19. | Yang BL, Gu YF, Shao WJ, Chen HJ, Sun GD, Jin HY, Zhu X. Retrorectal tumors in adults: magnetic resonance imaging findings. World J Gastroenterol. 2010;16:5822-5829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Badmos KB, Ibrahim OK, Aboyeji AP, Omotayo JA. Squamous cell carcinoma arising in a mature cystic ovarian teratoma with bladder invasion: a case report. Afr Health Sci. 2011;11:285-287. [PubMed] |
| 21. | Lee SW, Southall JC, Gleason NR, Huang EH, Bessler M, Whelan RL. Time course of differences in lymphocyte proliferation rates after laparotomy vs CO(2) insufflation. Surg Endosc. 2000;14:145-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Chansoon T, Angkathunyakul N, Aroonroch R, Jirasiritham J. Duodenal mature teratoma causing partial intestinal obstruction: A first case report in an adult. World J Clin Cases. 2020;8:1489-1494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Yoon SS, Tanabe KK, Warshaw AL. Adult primary retroperitoneal teratoma. Surgery. 2005;137:663-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | James J, Dhillon GS, Blewett CJ, Halldorsson A, Cecalupo AJ. A large adrenal teratoma in a neonate. Am Surg. 2009;75:347-349. [PubMed] [DOI] [Full Text] |
| 25. | Murdock J, Abbas MA. Laparoscopic abdomino-paracoccygeal resection of anorectal cystic teratoma. JSLS. 2010;14:583-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Wang L, Hirano Y, Ishii T, Kondo H, Hara K, Ishikawa S, Okada T, Obara N, Yamaguchi S. Laparoscopic surgical management of a mature presacral teratoma: a case report. Surg Case Rep. 2019;5:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Aiken A, Yu W, Abudoureyimu A, Aizimu X, Tong J. A case of primary rectal teratoma. Turk J Gastroenterol. 2020;31:835-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Nam KH, Kim B. Primary Mature Teratoma of the Rectum: A Case Report. Am J Case Rep. 2021;22:e930272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |