Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7720
Peer-review started: September 29, 2021
First decision: April 7, 2022
Revised: April 26, 2022
Accepted: June 16, 2022
Article in press: June 16, 2022
Published online: August 6, 2022
Processing time: 296 Days and 6.9 Hours
Cervical facet joint pain (CFP) is one of the most common causes of neck pain and headache. Persistent CFP deteriorates the quality of life of patients and reduces their productivity at work.
To investigate the effectiveness of pulsed radiofrequency (PRF) stimulation of cervical medial branches in patients with chronic CFP.
We retrospectively included 21 consecutive patients (age = 50.9 ± 15.3 years, range 26-79 years; male: female = 8:13; pain duration = 7.7 ± 5.0 mo) with chronic CFP, defined as ≥ 4 on the numeric rating scale (NRS). We performed PRF stimulation on the cervical medial branches. The outcomes of the PRF procedure were evaluated by comparing the NRS scores for CFP before treatment and 1 and 3 mo after treatment. Successful pain relief was defined as a ≥ 50% reduction in the NRS score at 3 mo when compared with the pretreatment NRS score.
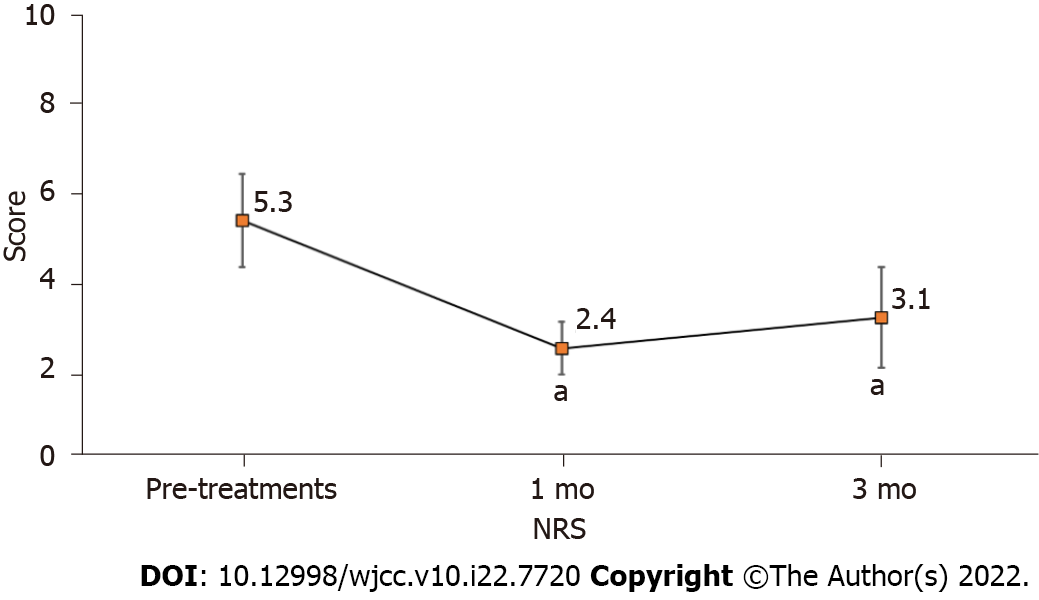
No patient had immediate or late adverse effects following PRF. The average NRS score for CFP decreased from 5.3 ± 1.1 at pre-treatment to 2.4 ± 0.6 at the 1 mo follow-up, and 3.1 ± 1.1 at the 3 mo follow-up. Compared to the NRS scores before PRF stimulation, those at 1 and 3 mo after PRF stimulation had significantly decreased. Eleven of the 21 patients (52.4%) reported successful pain relief 3 mo after the PRF procedure. PRF stimulation on cervical medial branches may be a useful therapeutic option to control chronic CFP.
PRF stimulation of the cervical medial branches may be used as an alternative treatment method in patients with CFP. PRF can effectively alleviate CFP, and is safe to perform.
Core Tip: This is a retrospective study to investigate the effectiveness of pulsed radiofrequency (PRF) stimulation of cervical medial branches in patients with chronic cervical facet pain (CFP). Eleven of the 21 patients (52.4%) reported successful pain relief 3 mo after the PRF procedure. Compared to the numeric rating scale scores for CFP before PRF stimulation, those at 1 and 3 mo after PRF stimulation had significantly decreased after 1-month and 3-month follow-up. PRF stimulation on cervical medial branches may be a useful therapeutic option to control chronic CFP.
- Citation: Chang MC, Yang S. Effectiveness of pulsed radiofrequency on the medial cervical branches for cervical facet joint pain. World J Clin Cases 2022; 10(22): 7720-7727
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7720.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7720
Cervical facet joint pain (CFP) is one of the most common causes of neck pain and headache[1,2]. Clinicians frequently encounter patients with CFP, the prevalence of which ranges from 36% to 55%[1]. If CFP persists and progresses to chronic pain, its management becomes difficult[3]. Persistent CFP deteriorates the quality of life of patients and reduces their productivity at work[4]. Furthermore, it can cause affective disorders, such as depression and anxiety, and sleep disturbance[5]. Therefore, clinicians should actively control CFP.
Several treatments, such as facet joint injection of corticosteroids, oral medication, and physical therapy, have been used to control CFP[6-8]. However, despite these treatments, many patients complain of persistent CFP. Conventional radiofrequency (CRF) stimulation of the cervical medial branch has also been used to control CFP[9,10]. This involves continuous stimulation, which causes the ablation of nerves and tissues by frictional heat from a catheter needle[6,7]. Due to this characteristic of CRF, neuropathic pain following the ablation of nerves can occur, and electrical burns after the procedure have been reported[10,11]. In contrast to CRF, pulsed radiofrequency (PRF) is a useful tool to alleviate chronic pain. This uses a brief stimulation, followed by a long resting phase[12]. PRF exposes the target nerves and tissues to an electric field, and rarely damages these structures[12]. Because of this minimal tissue-destructive characteristic, PRF has been rapidly adopted in clinical practice for the treatment of several types of pain, including neuralgia, joint pain, and myofascial pain[12-16]. Recently, several studies have reported a positive effect of PRF on medial branches in the spine to manage facet pain[17,18]. However, little is known about its effect on the cervical medial branch in the management of CFP.
In the current study, we evaluated the effectiveness of PRF stimulation of cervical medial branches in patients with chronic CFP.
This study was conducted retrospectively. We consecutively recruited patients who received PRF stimulation of the cervical medial branches under fluoroscopy in a pain clinic at a single university hospital from January 2014 to December 2019. The inclusion criteria were as follows: (1) PRF stimulation of cervical medial branches performed to control CFP; (2) Aged between 20 and 79 years; (3) ≥ 3 mo history of axial cervical pain without radicular symptoms; (4) ≥ 80% temporary pain relief following a diagnostic cervical medial branch block with 0.5 mL of 1% lidocaine for each level prior to PRF stimulation of cervical medical branches; (5) ≥ 4 points on the Numeric Rating Scale (NRS, 0 = no pain, 10 = worst pain imaginable) prior to PRF stimulation of the cervical medial branches; and (6) No procedure to treat CFP performed ≥ 3 mo prior to the PRF stimulation. Each patient underwent cervical spine magnetic resonance imaging. We excluded patients who experienced cervical radicular pain due to disc herniation or foraminal stenosis and neck pain due to cervical canal stenosis. We retrospectively reviewed the medical records of 90 patients and included 21 patients (age = 50.9 ± 15.3 years, range 26-79 years; male: female = 8:13; pain duration = 7.7 ± 5.0 mo) in the analysis. A putatively painful cervical facet joint was selected on the basis of the distribution of pain and the location of tenderness[12]. All the included patients agreed to undergo PRF stimulation of cervical medial branches prior to the procedure. The Institutional Review Board of Yeungnam university hospital approved this study, and the need for written informed consent was waived due to the retrospective design of the study.
An aseptic technique was adopted for PRF stimulation of the cervical medial branches using a posterior approach. For the procedure, patients were placed in a prone position, with the chest supported by a pillow, and the head slightly bent. Under the guidance of C-arm fluoroscopy (Siemens), a 22-gauge cannula (SMK Pole needle, 100 mm with a 10 mm active tip, Cotop International BV) was inserted in a posterior to anterior direction, and its tip was placed around the cervical medial branches, just lateral to the posteroanterior center of the C2-3 facet joint for the superficial medial branch of the third cervical spinal dorsal ramus (third occipital nerve), waists of the articular pillars of C3-C6 for C3-6 medial branches, and the apex of the superior articular process of C7 for the C7 medial branch (Figure 1). PRF stimulation of the superficial medial branch of the third cervical spinal dorsal ramus was conducted to control the C2-3 facet joint pain (third occipital nerve). For C3-4, C4-5, and C6-7 facet joint pain, the two vertically adjacent spinal medial branches, the C3 (deep medial branch of the third cervical spinal dorsal ramus) and C4, C4 and C5, and C6 and C7 medial branches were stimulated, respectively (Table 1)[19]. Once the needle tip was at the target site of the medial cervical branch, the needle was repositioned until the patient reported pain or a pressure sensation similar to the pain they usually experienced at less than 0.5 V to confirm the proximity to the medial cervical branch. An electrode was connected to the cannula, and the thoracic medial branch was stimulated (G4 radiofrequency generator; Cosman Medical Inc., Burlington, MA, United States). PRF treatment was administered at 5 Hz, with a 5-millisecond pulsed width for 360 s at 45 V under the condition that the electrode tip temperature did not exceed 42 °C.
| Patient | Stimulated level |
| 1 | Lt. C4, 5, 6 |
| 2 | Rt. C4, 5, 6 |
| 3 | Rt. TON, C3, 4, 5 |
| 4 | Both C3, 4, 5 |
| 5 | Rt. C3, 4 |
| 6 | Rt. TON, C3, 4 |
| 7 | Lt. C3, 4, 5 |
| 8 | Rt. C3, 4, 5 |
| 9 | Rt. TON, C3, 4, 5 |
| 10 | Lt. C3, 4, 5 |
| 6 | Rt. TON, C3, 4 |
| 7 | Lt. C3, 4, 5 |
| 8 | Rt. C3, 4, 5 |
| 9 | Rt. TON, C3, 4, 5 |
| 10 | Lt. C3, 4, 5 |
| 11 | Rt. TON, C3, 4, 5, 6 |
| 12 | Lt. C5, 6, 7 |
Pain intensities were assessed using the NRS pain scores before and 1 and 3 mo after PRF treatment. Successful pain relief was defined as ≥ 50% reduction in the NRS score at 3 mo as compared with the pretreatment NRS score. Changes in NRS scores were also calculated as the difference between the pretreatment and 3 mo post treatment scores, to validate the degree of change in pain reduction [change in NRS (%) = (pretreatment score – scores at 3 mo post treatment)/pretreatment score × 100]. After 3 mo, the patient global perceived effect (GPE) was assessed using a 7-point Likert scale (Table 2)[20,21]. Patients reporting very good (score = 7) or good results (score = 6) were considered to be satisfied with the procedure.
| Score | % Change | Description |
| 7 | ≥ 75 improvement | Very good |
| 6 | 50-74 improvement | Good |
| 5 | 25-49 improvement | Fairly good |
| 4 | 0-24 improvement or worse | Same as before |
| 3 | 25-49 worse | Fairly bad |
| 2 | 50-74 worse | Bad |
| 1 | ≥ 75 worse | Very bad |
Statistical analysis was performed with SPSS, version 23.0 (IBM Corporation, Armonk, NY, United States) for Windows (Microsoft Corporation, Redmond, WA, United States). The overall change in NRS scores over time was evaluated using a repeated-measures one-factor analysis. Multiple comparison results were obtained with Bonferroni correction. Statistical significance was set at P < 0.05.
None of the patients presented immediate or late adverse effects following the PRF procedure. The average NRS score for CFP declined from 5.3 ± 1.1 at pre-treatment to 2.4 ± 0.6 at the 1 mo follow-up and 3.1 ± 1.1 at the 3 mo follow-up. The NRS scores significantly changed over time (P < 0.001; Figure 2). Compared to the NRS scores before PRF stimulation, those at 1 and 3 mo after PRF stimulation were significantly decreased (P < 0.001). Eleven of the 21 patients (52.4%) reported successful pain relief (≥ 50%) at 3 mo after PRF stimulation.
On the 7-point Likert scale, Good (score = 6) and fairly good results (score = 5) were observed in 11 (52.4%) and 5 patients (23.8%), respectively. However, no change in results (score = 4) was observed in 5 patients (23.8%). Accordingly, 11 patients (52.4%) were satisfied with the results 3 mo after the PRF procedure. Very good (score =7), fairly bad (score = 3), bad (score = 2), and very bad (score = 1) scores were not reported. These findings demonstrated that PRF stimulation was effective at alleviating CFP, and more than half of patients who received the treatment were satisfied with the results of this treatment.
In the current study, we found that PRF simulation of the cervical medical branches could effectively control chronic CFP. After undergoing PRF stimulation of the cervical medial branch, significant pain relief was observed in patients with CFP, and approximately half of the patients reported successful pain relief (≥ 50% pain reduction); this effect lasted for at least 3 mo. Furthermore, about half of the patients reported successful pain relief and satisfaction with the results following PRF stimulation.
Facet joints are true synovial joints. It is assumed that the production of inflammatory cytokines and matrix-degrading enzymes disturbs chondrocyte metabolism, leading to cartilage degradation, as in other osteoarthritic joints[22]. Repetitive chemical and mechanical stress on cervical facet joints causes inflammation and narrowing of the capsule, resulting in osteoarthritis and chronic CFP[23]. Additionally, facet joint injury can occur due to whiplash injury following a sudden acceleration-deceleration force, which is a common cause of chronic CFP[19].
Medial branch nerves are very small nerve branches that carry pain signals from facet joints to the brain. There are various treatment methods for CFP. Physical therapy, manipulation, mobilization, oral medication, and cognitive behavioral therapy may all be applied, but their pain-reducing effect is controversial[24]. Three types of interventions for the treatment of CFP include intraarticular facet injections, medial branch blocks (MBBs), and neurolysis of medial branch nerves using radiofrequency[25]. The MBB is performed with corticosteroids and local anesthetics to reduce CFP. This may provide pain relief by suppressing nociceptive discharges and blocking the axonal transport and sympathetic reflex arc, thereby exerting anti-inflammatory effects[17]. However, local anesthetics can cause various adverse effects, such as hypotension, dizziness, nausea, seizures, and cardiac arrest[26]. Moreover, repeated corticosteroid injections can cause hyperglycemia, suppression of the hypothalamic-pituitary-adrenal axis, and osteoporosis[27]. To avoid the side effects of local anesthetics and corticosteroids, PRF stimulation was suggested as an alternative treatment method for CFP. No previous study has yet directly compared the effect of PRF stimulation to the cervical medial branches with other treatment methods for non-traumatic facet pain. Therefore, this study aimed to investigate whether PRF stimulation was effective in the management of chronic CFP.
PRF stimulation is a minimally neuro-destructive treatment applied in clinical practice to treat pain related to the facet joint, without inducing any significant complications[9]. The main advantages of PRF stimulation are that the procedure is painless and does not induce thermal damage to the tissues. PRF produces an electric field, which exerts a local or regional effect on immune cells, thus preventing progression to chronic pain[28,29]. The nociceptive inputs may be reduced along the pain pathways, and the electrical fields produced by PRF may alter the synaptic signal transmission[12]. Furthermore, PRF stimulation is reported to decrease microglia activity in the spinal dorsal horn[28]. Because microglia release several cytokines and chemokines that are associated with progression to chronic pain, the down-regulation of microglia activity can control pain[28]. Additionally, PRF stimulation may cause microscopic damage to unmyelinated C fibers that transfer the pain sensation[30].
The effect of PRF stimulation on the management of patients with CFP was documented in two studies. Mikeladze et al[30] investigated the effect of PRF on patients with cervical or lumbar facet joint pain. More than half of the patients (68 out of 114 patients) reported pain relief of 50% or more after PRF stimulation at 42 °C for 120 s. Liliang et al[31] enrolled patients with whiplash-related chronic CFP, and showed that PRF stimulation of the cervical medial branches relieved pain and reduced medication requirement. Our study included patients with only CFP, and the enrolled patients were not confined to those with a history of trauma. In line with these previous studies, the results of our study support the fact that PRF stimulation is safe and might effectively relieve CFP. In our study, PRF simulation was performed by a single physician with approximately 20 years of spinal intervention experience. Therefore, the risk of operator bias is low. Five patients in our study showed no improvement in CFP after PRF stimulation. This may be due to different underlying mechanisms involved in the deve
However, there are several limitations to this study. First, the sample size was small. Second, this study lacked a placebo-controlled group. However, there are ethical considerations regarding the use of placebo in a controlled trial with patients who suffer from moderate to severe pain. Third, this study was conducted retrospectively. Fourth, the level of the origin of CFP was determined on the basis of distribution of pain, potentially adding a subjective component to our study. Fifth, we did not measure a beneficial effect on the quality of life. Further studies, including randomized controlled trials, are needed to compensate for these limitations. Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
In conclusion, we found that CFP was significantly reduced at 1 and 3 mo after PRF stimulation. The rate of successful pain relief and patient satisfaction at 3 mo after PRF stimulation was found to be 52.4%. In the current study, we showed that PRF stimulation of the cervical medial branches may be used as an alternative treatment method in patients with CFP. PRF may alleviate CFP effectively and is safe to perform.
Cervical facet joint pain (CFP) is one of the most common causes of neck pain and headache. Persistent CFP deteriorates the quality of life of patients and reduces their productivity at work.
In order to investigate the effectiveness of pulsed radiofrequency (PRF) stimulation of cervical medial branches in patients with chronic CFP.
The authors aim to investigate the effectiveness of PRF stimulation of cervical medial branches in patients with chronic CFP.
The authors retrospectively included 21 consecutive patients (age = 50.9 ± 15.3 years, range 26-79 years; male: female = 8:13; pain duration = 7.7 ± 5.0 mo) with chronic CFP, defined as ≥ 4 on the numeric rating scale (NRS). The authors performed PRF stimulation on the cervical medial branches.
The outcomes of the PRF procedure were evaluated by comparing the NRS scores for CFP before treatment and 1 and 3 mo after treatment. Successful pain relief was defined as a ≥ 50% reduction in the NRS score at 3 mo when compared with the pretreatment NRS score.
PRF stimulation of the cervical medial branches may be used as an alternative treatment method in patients with CFP. PRF can effectively alleviate CFP, and is safe to perform.
PRF stimulation on cervical medial branches may be a useful therapeutic option to control chronic CFP.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhatjiwale M, India A-Editor: Lin FY, China S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Kirpalani D, Mitra R. Cervical facet joint dysfunction: a review. Arch Phys Med Rehabil. 2008;89:770-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 284] [Cited by in RCA: 236] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 3. | Yang S, Chang MC. Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Affective States. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 210] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 4. | Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 386] [Cited by in RCA: 575] [Article Influence: 63.9] [Reference Citation Analysis (0)] |
| 5. | Davis MC, Zautra AJ, Smith BW. Chronic pain, stress, and the dynamics of affective differentiation. J Pers. 2004;72:1133-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 116] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Choo YJ, Chang MC. Effectiveness of orthoses for treatment in patients with spinal pain. Yeungnam Univ J Med. 2020;37:84-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Curatolo M. Pharmacological and Interventional Management of Pain After Whiplash Injury. J Orthop Sports Phys Ther. 2016;46:845-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Manchikanti L, Pampati V, Parr Iii A, Manchikanti MV, Sanapati MR, Kaye AD, Hirsch JA. Cervical Interlaminar Epidural Injections in the Treatment of Cervical Disc Herniation, Post Surgery Syndrome, or Discogenic Pain: Cost Utility Analysis from Randomized Trials. Pain Physician. 2019;22:421-431. [PubMed] |
| 9. | Arsanious D, Gage E, Koning J, Sarhan M, Chaiban G, Almualim M, Atallah J. Pulsed Dose Radiofrequency Before Ablation of Medial Branch of the Lumbar Dorsal Ramus for Zygapophyseal Joint Pain Reduces Post-procedural Pain. Pain Physician. 2016;19:477-484. [PubMed] |
| 10. | Wu H, Zhou J, Chen J, Gu Y, Shi L, Ni H. Therapeutic efficacy and safety of radiofrequency ablation for the treatment of trigeminal neuralgia: a systematic review and meta-analysis. J Pain Res. 2019;12:423-441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | McCormick ZL, Smith CC, Engel AJ; Spine Intervention Society’s Patient Safety Committee. Preventing External Skin Burns During Thermal Radiofrequency Neurotomy. Pain Med. 2019;20:852-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Sluijter ME, Cosman E, Rittman W. The effects of pulsed radiofrequency fields applied to the dorsal root ganglion—a preliminary report. Pain Clin. 1998;11:109-117. |
| 13. | Boudier-Revéret M, Thu AC, Hsiao MY, Shyu SG, Chang MC. The Effectiveness of Pulsed Radiofrequency on Joint Pain: A Narrative Review. Pain Pract. 2020;20:412-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Cho IT, Cho YW, Kwak SG, Chang MC. Comparison between ultrasound-guided interfascial pulsed radiofrequency and ultrasound-guided interfascial block with local anesthetic in myofascial pain syndrome of trapezius muscle. Medicine (Baltimore). 2017;96:e6019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Park CH, Lee SH. The Outcome of Pulsed Radiofrequency Treatment According to Electodiagnosis in Patients with Intractable Lumbosacral Radicular Pain. Pain Med. 2019;20:1697-1701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Park SM, Cho YW, Ahn SH, Lee DG, Cho HK, Kim SY. Comparison of the Effects of Ultrasound-Guided Interfascial Pulsed Radiofrequency and Ultrasound-Guided Interfascial Injection on Myofascial Pain Syndrome of the Gastrocnemius. Ann Rehabil Med. 2016;40:885-892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Chang MC. Effect of Pulsed Radiofrequency Treatment on the Thoracic Medial Branch for Managing Chronic Thoracic Facet Joint Pain Refractory to Medial Branch Block with Local Anesthetics. World Neurosurg. 2018;111:e644-e648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Colini-Baldeschi G. Evaluation of pulsed radiofrequency denervation in the treatment of chronic facetjoint pain: an observational study. Anesth Pain Med. 2012;1:168-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Persson M, Sörensen J, Gerdle B. Chronic Whiplash Associated Disorders (WAD): Responses to Nerve Blocks of Cervical Zygapophyseal Joints. Pain Med. 2016;17:2162-2175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3507] [Cited by in RCA: 4030] [Article Influence: 167.9] [Reference Citation Analysis (0)] |
| 21. | Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;140-145. |
| 22. | Schianchi PM. A new technique to treat facet joint pain with pulsed radiofrequency. Anesth Pain Med. 2015;5:e21061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | van Kleef M, Vanelderen P, Cohen SP, Lataster A, Van Zundert J, Mekhail N. 12. Pain originating from the lumbar facet joints. Pain Pract. 2010;10:459-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 24. | van Eerd M, Patijn J, Lataster A, Rosenquist RW, van Kleef M, Mekhail N, Van Zundert J. 5. Cervical facet pain. Pain Pract. 2010;10:113-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Falco FJ, Erhart S, Wargo BW, Bryce DA, Atluri S, Datta S, Hayek SM. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 2009;12:323-344. [PubMed] |
| 26. | Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician. 2002;5:182-199. [PubMed] |
| 27. | Manchikanti L, Boswell MV, Singh V, Derby R, Fellows B, Falco FJ, Datta S, Smith HS, Hirsch JA. Comprehensive review of neurophysiologic basis and diagnostic interventions in managing chronic spinal pain. Pain Physician. 2009;12:E71-120. [PubMed] |
| 28. | Cho HK, Cho YW, Kim EH, Sluijter ME, Hwang SJ, Ahn SH. Changes in pain behavior and glial activation in the spinal dorsal horn after pulsed radiofrequency current administration to the dorsal root ganglion in a rat model of lumbar disc herniation: laboratory investigation. J Neurosurg Spine. 2013;19:256-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 29. | Higuchi Y, Nashold BS Jr, Sluijter M, Cosman E, Pearlstein RD. Exposure of the dorsal root ganglion in rats to pulsed radiofrequency currents activates dorsal horn lamina I and II neurons. Neurosurgery. 2002;50:850-5; discussion 856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 164] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 30. | Mikeladze G, Espinal R, Finnegan R, Routon J, Martin D. Pulsed radiofrequency application in treatment of chronic zygapophyseal joint pain. Spine J. 2003;3:360-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 81] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Liliang PC, Lu K, Hsieh CH, Kao CY, Wang KW, Chen HJ. Pulsed radiofrequency of cervical medial branches for treatment of whiplash-related cervical zygapophysial joint pain. Surg Neurol. 2008;70 Suppl 1 S1:50-5; discussion S1:55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Fornasari D. Pain mechanisms in patients with chronic pain. Clin Drug Investig. 2012;32 Suppl 1:45-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |