Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.741
Peer-review started: August 19, 2021
First decision: November 1, 2021
Revised: November 12, 2021
Accepted: December 7, 2021
Article in press: December 7, 2021
Published online: January 14, 2022
Processing time: 145 Days and 14.7 Hours
Fibrotic hypersensitivity pneumonitis (FHP) is an allergic and diffuse pneumonia caused by repeated inhalation of antigenic substances, and sometimes developed in people working in specific environments. While novel antigens and exposures continued to be described, physicians should maintain a high suspicion of potential exposures. A detailed assessment of the patient's occupational exposures as well as living environment is necessary and complete allergen avoidance is the first and most important step in the management of FHP once the allergens are determined.
A 35-year-old female was admitted to the hospital with a cough and breathing difficulties for more than one year. She was a nonsmoker and a manufacturer of halogen dishes, which are characteristic Chinese foods, for 15 years without any protection. High resolution computed tomography of the chest demonstrated an interstitial pneumonia pattern. Pulmonary function examination showed restricted ventilation dysfunction and a significant reduction in dispersion ability. Cell differentiation in bronchoalveolar lavage fluid demonstrated lymphocytosis (70.4%) with an increased lymphocyte CD4/CD8 ratio (0.94). Transbronchial lung biopsy combined with lung puncture pathology showed diffuse uniform alveolar interval thickening, chronic inflammatory cell infiltration, a proliferation of tissue in the bronchial wall fiber and alveolar epithelial follicle degeneration, resulting in fibrosis.
Exposure to spices used for the production of halogen dishes may cause FHP.
Core Tip: Fibrotic hypersensitivity pneumonitis (FHP) is a disease related to immunological response to an inhaled antigen. Avoiding contact with susceptible antigen is the key. Here, we report a case of FHP in a halogen dishes manufacturer probably associated with exposure to the spices. We recommend to enhance respiratory protection during the production of such dishes to prevent this lung disease.
- Citation: Wang M, Fang HH, Jiang ZF, Ye W, Liu RY. Occupational fibrotic hypersensitivity pneumonia in a halogen dishes manufacturer: A case report. World J Clin Cases 2022; 10(2): 741-746
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/741.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.741
Fibrotic hypersensitivity pneumonitis (FHP) is a chronic and fibrosing interstitial lung disease caused by inhaled antigen exposure which can develop in people working in specific environments or with specific career[1]. The commonly known form is Farmer's lung[2]. Halogen dishes are Chinese cuisines in which long-term boiling of various spices powder is required before meat and vegetables are added. Each halogen maker has a so-called secret recipe, but almost all contain ginger, pepper, soy sauce, and other spices. A single case of hypersensitivity pneumonitis (HP) associated with curry powder and ground pepper in a potato chip factory has been described[3]. We herein report a case of FHP in a halogen dishes manufacturer, which may have been caused by the inhalation of spices.
FHP can lead to impaired respiratory function, reduced disease-related quality of life, and early mortality. Management of FHP should start with exposure remediation once the source of allergy is identified. A high index of suspicion is important to diagnosis, even after innocuous and apparently trivial exposures to potential antigens. We herein report a case of FHP in a halogen dishes manufacturer, which may have been caused by inhalation of spices.
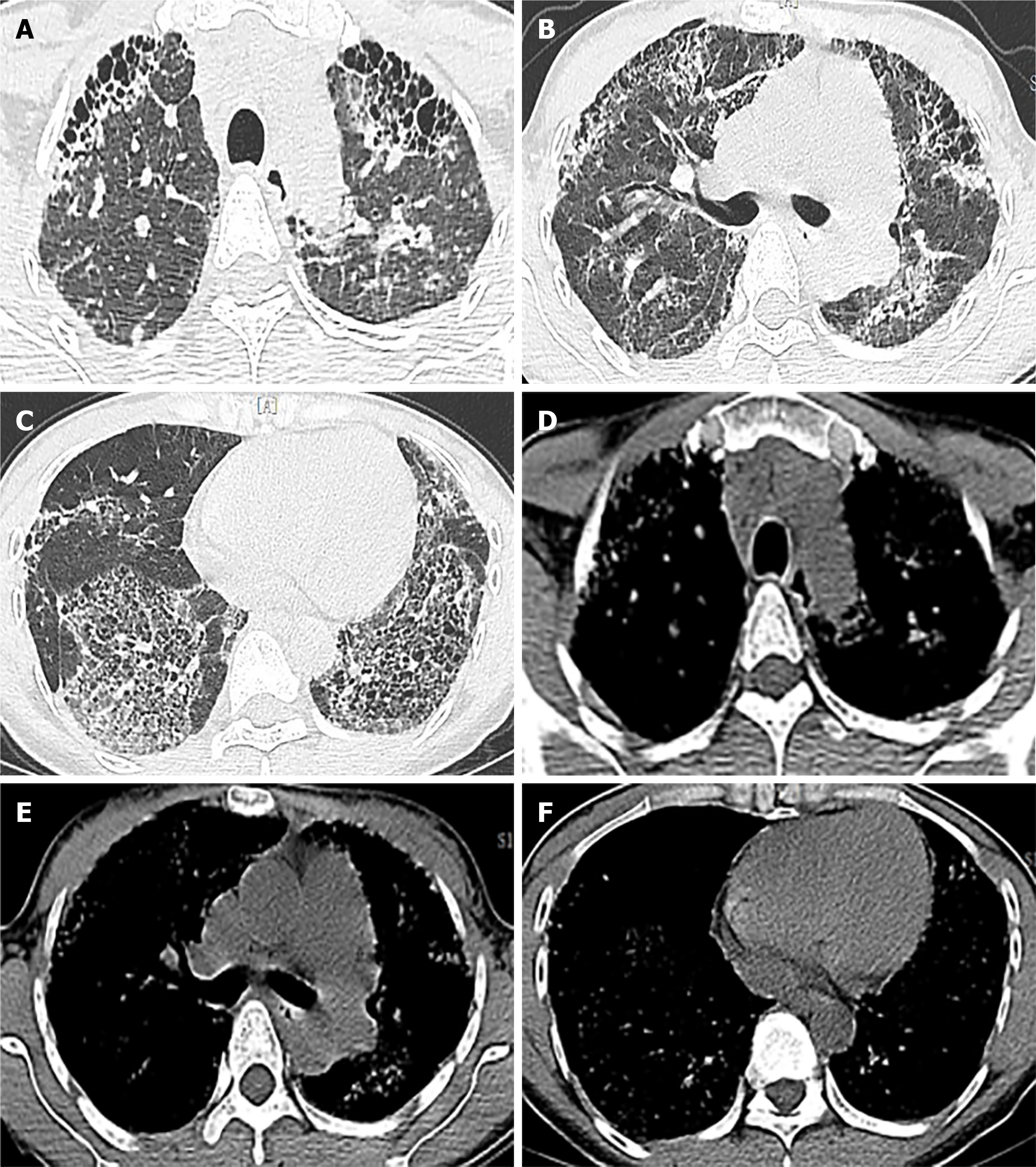
High resolution computed tomography (HRCT) of the chest showed thickening of interlobular septa and central lobular nodules which revealed honeycomb changes in severe areas (mainly in the lung base), as well as traction bronchiectasis (Figure 1).
Routine blood, liver function, renal function tests and serum sodium, potassium, creatinine, magnesium, and calcium were all within normal limits. Blood tumor biomarkers including anti-nuclear antibody, anti-centromere antibody, anti-neutrophil cytoplasmic antibody, and Scl-70 antibody screens and C-reactive protein were negative. Pulmonary function tests showed a forced vital capacity (FVC) of 1.75 L (51.2% predicted), a forced expiratory volume in 1 s (FEV1) of 1.63 L (55%), an FEV1/FVC ratio of 109.6%, and carbon monoxide diffusing capacity 11.9 mmHg/mL/min (39% predicted). Cytology of bronchoalveolar lavage (BAL) fluid showed a large number of lymphocytes (the total number of cells was 4.16x106/mL, lymphocytes accounted for 70.4%, of which the lymphocyte CD4/CD8 ratio was 0.94, and bronchoscopy was performed to rule out a superimposed infection. Allergen determination showed that tree, pollen, ragweed, Artemisia argyi, home dust mite, home dust, cat hair, dog hair, cockroach, mold combination, legume, egg white, milk, peanut, soybean, beef, mutton, cod, shrimp, crab, salmon, lobster, scallop, etc. were all negative.
On examination, her temperature was 36.7 ℃, blood pressure was 118/82 mmHg, heart rate was 74 bpm, oxygen saturation was 92% in room air, and respiratory rate was 22 breaths/min. The patient was identified as Grade 3-shortness of breath according to the mMRC (Modified Medical Research Council) dyspnea scale and lung examination revealed bilateral Velcro like crackles in the lower lung fields. The rest of her physical examination was unremarkable.
This patient had no special personal and family history.
She was a self-employed worker, cooking and selling halogen dishes for over 15 years, without any measures to protect the respiratory tract. There was no history of orthopnea, chest pain, or paroxysmal nocturnal dyspnea. She denied smoking and there was no history of asthma, allergies, or any other prior pulmonary disease.
The patient took anti-inflammatory and cough medications intermittently, but there was no improvement in her symptoms.
A 35-year-old Chinese woman with no significant medical history was admitted to our hospital because of a cough and breathing difficulties. She was a self-employed cook who produced and sold halogen dishes for more than 15 years without appropriate equipment to protect the airway from inhalation.
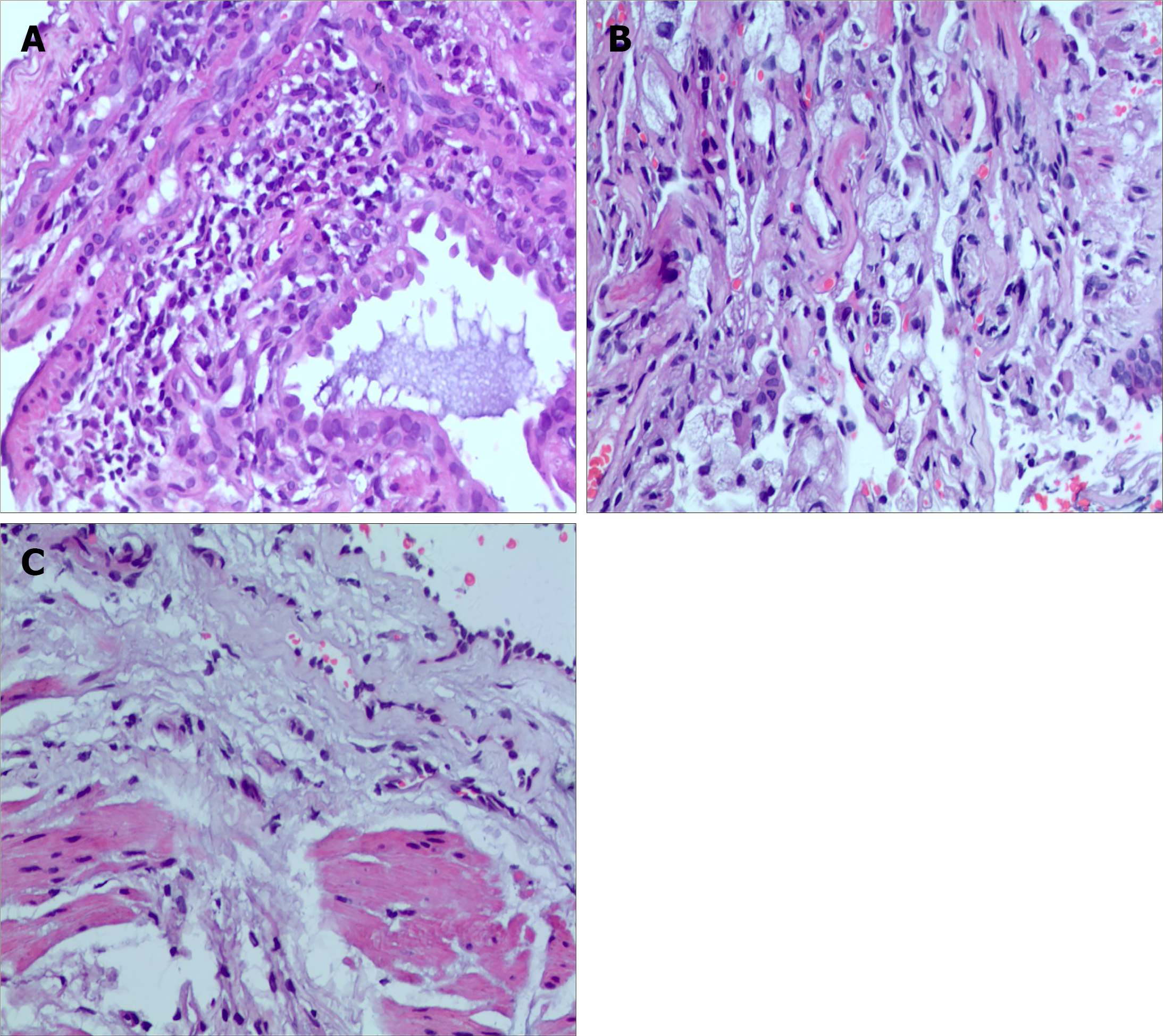
Fan-Qing Meng, MD, Professor, Department of Pathology. Fibrin-like exudation, more lymphocytes, foam-like tissue cells and a small number of macrophages were observed on histopathology of lavage fluid, suggesting persistent exposure to inhaled antigen. Transbronchial lung biopsy (TBLB) and computerized tomography-guided percutaneous lung puncture showed chronic lymphocyte and foamy macrophages infiltration, diffuse, relatively uniform alveolar septal thickness, hyperplasia of fibrous tissue in the bronchial wall, resulting in fibrosis (Figure 2).
Occupational FHP due to probable long-term exposure of spices in a halogen dishes manufacturer.
The patient was started on prednisone 30 mg/d and pirfenidone anti-fibrosis treatment. Considering the side effects of high doses of hormones, the patient was discharged on a tapering schedule of prednisolone which was reduced by 5 mg every 2 wk.
The main symptoms of cough and breathing difficulties gradually improved slightly three months later, but no improvement in chest HRCT was noted. No significant adverse side-effects were noticed. The patient is currently on the lung transplant list.
This patient met the diagnostic criteria for FHP as she had a cough, breathing difficulties, long-term inhalation of spices, lymphocytic cellular pattern on BAL, bi-basilar rales, reduction in diffusion capacity, and compatible radiologic and histopathological findings. BAL can not only exclude other major causes of interstitial pneumonia including alveolar hemorrhage, malignancy, infection, and eosinophilic lung disease, but also exclude common allergens. While BAL lymphocyte percentage in HP can vary substantially from 1.7% to 82%[4], in this patient BAL showed an obvious lymphocytic cellular pattern (70.4% lymphocytes) defined as a BAL differential count greater than 15%[5]. Additionally, aggregation of foamy macrophages and lymphocyte infiltration was observed which indicated exposure to inhalant pathogens[6]. Serologic studies for spices were not performed due to the patient’s insurance status (she only had basic medical insurance and restricted economics), and had no relevance to the diagnosis even if negative as this would not exclude the clinical diagnosis of HP due to exposure to spices. Therefore, inhaled spices were the presumed cause of FHP in this case, especially given the absence of any other identifiable exposures.
Novel antigens and exposures related to occupation continue to be described, even innocuous and trivial exposures to potential antigens such as green tea[7], citrus[8], and pyrethrin[9] have been described. To our knowledge, this is the first case of FHP in a halogen dishes manufacturer caused by spices globally, which was confirmed by the presence of fibrosis through histological evaluation of TBLB and percutaneous lung puncture. However, it has also been pointed out that in the presence of a concomitant allergic predisposition, such as bronchial asthma, allergic rhinitis, or chronic bronchitis, the biological response to inhalation may be enhanced. There was no apparent comorbidity in our patient and she was a nonsmoker.
Heightened awareness of potential exposures is imperative in making a diagnosis and a detailed assessment of occupational exposures as well as the occupational environment is necessary as demonstrated in this case. Avoiding contact is the key for patients with HP, not only for patients but also for other individuals who may be exposed to the same allergen[9]. Although there are no obvious symptoms or failure of regular occupational disease physical examination or disease detection, it is essential to remind workers of their safety during the production process[8] (respirator, masks, improve ventilation, regular monitoring of air quality) and the compliance of workers should be confirmed. For those with established allergies, there are various ways to avoid exposure, for example, by changing jobs or occupations. Clinically appreciable improvement in symptomatic, physiologic, and radiographic features may be seen only in patients with non-fibrotic HP[10]. Due to the long and insidious exposure to antigen, fibrosis was observed both radiologically and pathologically in our patient. Management of FHP should start with exposure remediation where possible, oral glucocoticoids and azathioprine achieved an initial improvement in pulmonary function tests and symptoms[11], anti-fibrosis therapy should be considered in patients with symptomatic or progressive disease, and non-pharmacologic and supportive management should be offered and, in cases of treatment-resistant, progressive illness, lung transplant should be considered[12,13]. Based on this, we advised our patient to change her occupation, and prednisone and anti-fibrosis therapy was given to improve her symptoms. Halogen dishes manufacture is mostly a family business in China, the patient inherited the shop from her mother and had no other life skills, although she was no longer responsible for food preparation, she still sold the halogen dishes at the counter. Following treatment, her symptoms improved slightly and requiring long-term oxygen therapy, the HRCT scan showed no improvement. The patient is currently on the waiting list for a lung transplant.
Attention should be paid to the possibility of inhalation hypersensitivity pneumonitis caused by spices. Improvements in respiratory protection measures should be suggested for workers during the production process to avoid this type of lung disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Allergy
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Islam SMRU S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Fernández Pérez ER, Crooks JL, Swigris JJ, Solomon JJ, Mohning MP, Huie TJ, Koslow M, Lynch DA, Groshong SD, Fier K. Design and rationale of a randomised, double-blind trial of the efficacy and safety of pirfenidone in patients with fibrotic hypersensitivity pneumonitis. ERJ Open Res. 2021;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Chauvin P, Kerjouan M, Jégo P, Jouneau S, Lescoat A. [Hypersensitivity Pneumonitis: An update]. Rev Med Interne. 2021;42:772-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Ando S, Arai T, Inoue Y, Kitaichi M, Sakatani M. NSIP in a curry sauce factory worker. Thorax. 2006;61:1012-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | D'Ippolito R, Chetta A, Foresi A, Marangio E, Castagnaro A, Merliniaft S, Zompatori M, Olivieri D. Induced sputum and bronchoalveolar lavage from patients with hypersensitivity pneumonitis. Respir Med. 2004;98:977-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Meyer KC, Raghu G. Reply: The clinical utility of bronchoalveolar lavage cellular analysis in interstitial lung disease. Am J Respir Crit Care Med. 2013;187:777-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Sato S, Kusano K, Ohta H, Tsukahara Y, Kida G, Tsumiyama E, Nishizawa T, Oba T, Kawabe R, Yamakawa H, Akasaka K, Amano M, Takemura T, Matsushima H. Hairspray Inhalation-induced Interstitial Pneumonitis Evaluated by a Transbronchial Lung Cryobiopsy. Intern Med. 2021;60:2285-2289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Tanaka Y, Shirai T, Enomoto N, Asada K, Oyama Y, Suda T. Occupational hypersensitivity pneumonitis in a green tea manufacturer. Respirol Case Rep. 2016;4:e00152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kutsuzawa N, Takihara T, Shiraishi Y, Kajiwara H, Imanishi T, Fukutomi Y, Kamei K, Takahashi M, Enokida K, Horio Y, Ito Y, Hayama N, Oguma T, Asano K. Occupational Hypersensitivity Pneumonitis in a Japanese Citrus Farmer. Intern Med. 2021;60:3581-3584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Pu CY, Rasheed MR, Sekosan M, Sharma V. Pet Groomer's Lung: A novel occupation related hypersensitivity pneumonitis related to pyrethrin exposure in a pet groomer. Am J Ind Med. 2017;60:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Fernández Pérez ER, Travis WD, Lynch DA, Brown KK, Johannson KA, Selman M, Ryu JH, Wells AU, Tony Huang YC, Pereira CAC, Scholand MB, Villar A, Inase N, Evans RB, Mette SA, Frazer-Green L. Executive Summary: Diagnosis and Evaluation of Hypersensitivity Pneumonitis: CHEST Guideline and Expert Panel Report. Chest. 2021;160:595-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Ceci Bonello E, Gauci J, Bonello S, Fsadni P, Montefort S. Rituximab therapy in a patient with steroid-refractory bird fancier's lung. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Barnes H, Johannson KA. Management of Fibrotic Hypersensitivity Pneumonitis. Clin Chest Med. 2021;42:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Kapnadak SG, Raghu G. Lung transplantation for interstitial lung disease. Eur Respir Rev. 2021;30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |