Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5770
Peer-review started: November 21, 2021
First decision: December 26, 2021
Revised: January 6, 2022
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Processing time: 200 Days and 2 Hours
No known case of neuroendocrine tumour (NET) with schwannoma has been reported.
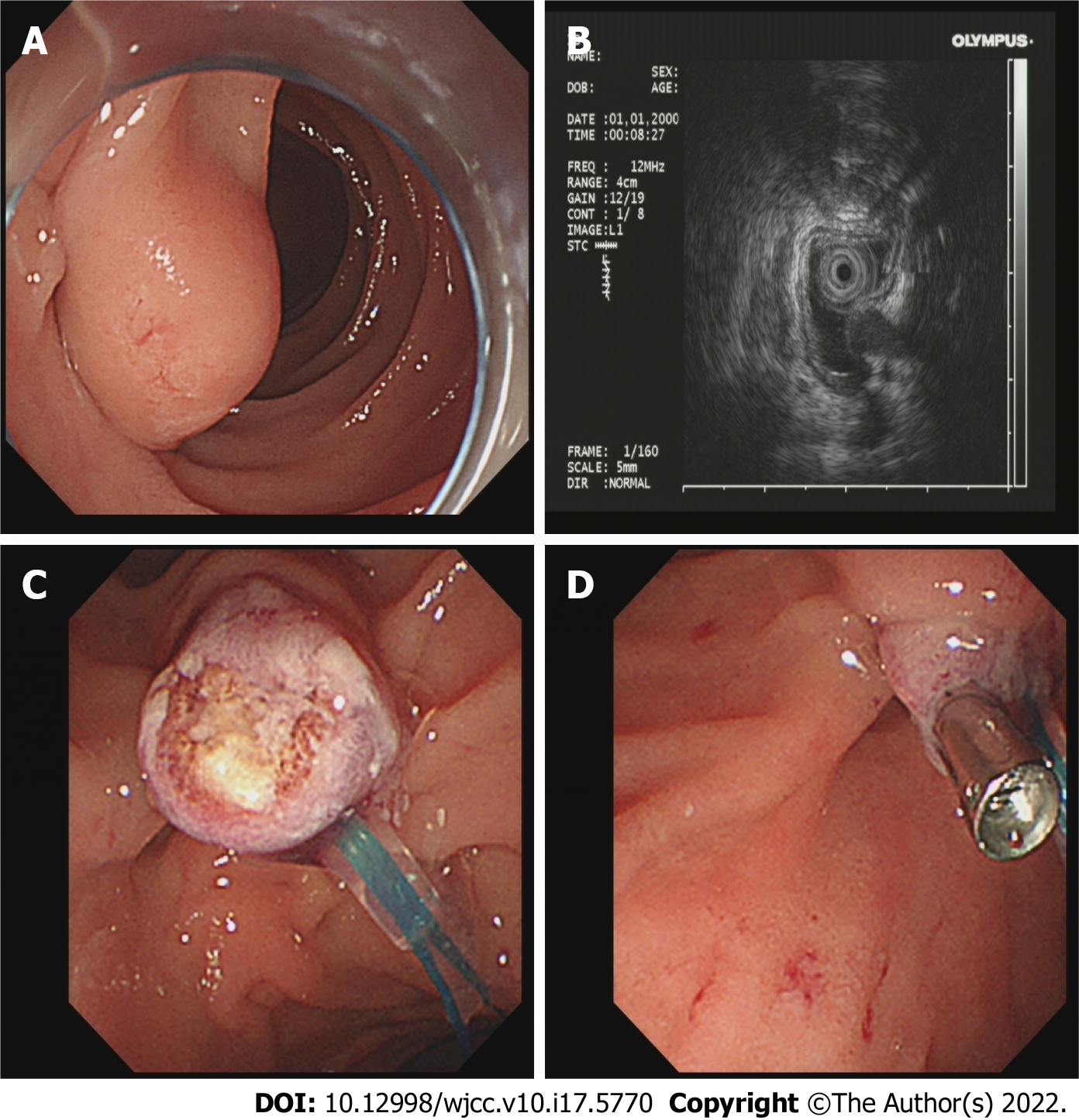
A 63-year-old female presented to our hospital with nausea and vomiting. Upper gastrointestinal endoscopy revealed a mass in the descending part of the duodenum. Using ultrasound gastroscopy, we found that the tumour originated from the submucosa and showed low echo. We removed the tumour by electrocoagulation and sent it for pathological biopsy.
Immunohistochemical results showed that the mass was a rare NET with neurile
Core Tip: Neuroendocrine tumours (NETs) and schwannomas of the duodenum are quite rare and few clinical cases have been reported. To the best of our knowledge, this is the first publication of a NET of descending duodenum complicated with schwannoma. Through a review of relevant literature, we can deepen the understanding of this type of tumour.
- Citation: Zhang L, Zhang C, Feng SY, Ma PP, Zhang S, Wang QQ. Neuroendocrine tumour of the descending part of the duodenum complicated with schwannoma: A case report. World J Clin Cases 2022; 10(17): 5770-5775
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5770.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5770
Neuroendocrine tumours (NETs) are rare tumours originating from neuroendocrine cells that account for approximately 2% of all malignant tumours, and approximately 50.6% of NETs are found in the digestive system; duodenal NETs are extremely rare, accounting for only 2%-3% of gastrointestinal NETs[1]. Schwannoma is a benign tumour originating from the nerve fibre sheath, accounting for approximately 5% of all soft tissue tumours; it is mostly located in the body surface and auditory nerve, less often in the digestive tract, and even more rarely in the duodenum[2].
One month of nausea and vomiting.
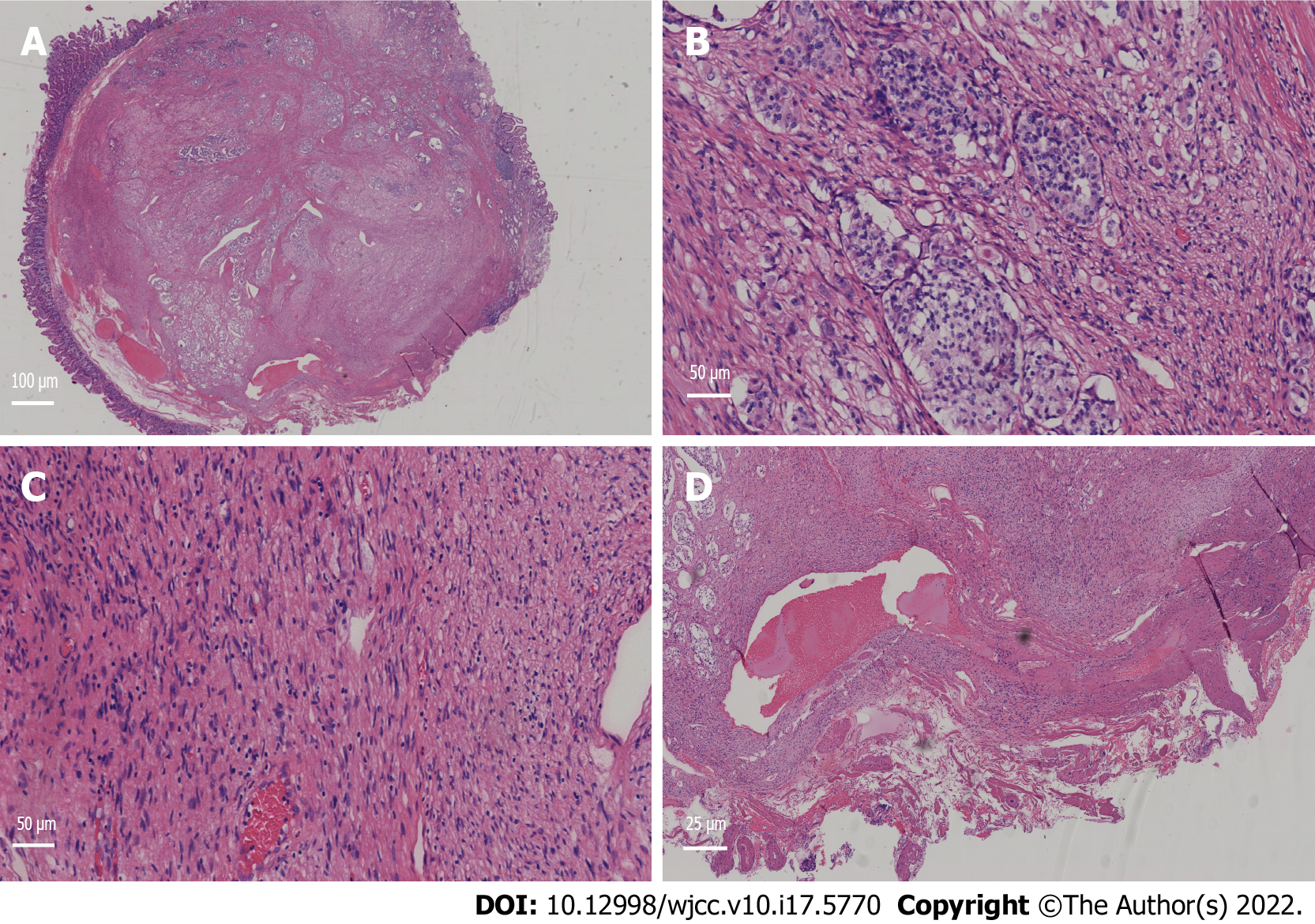
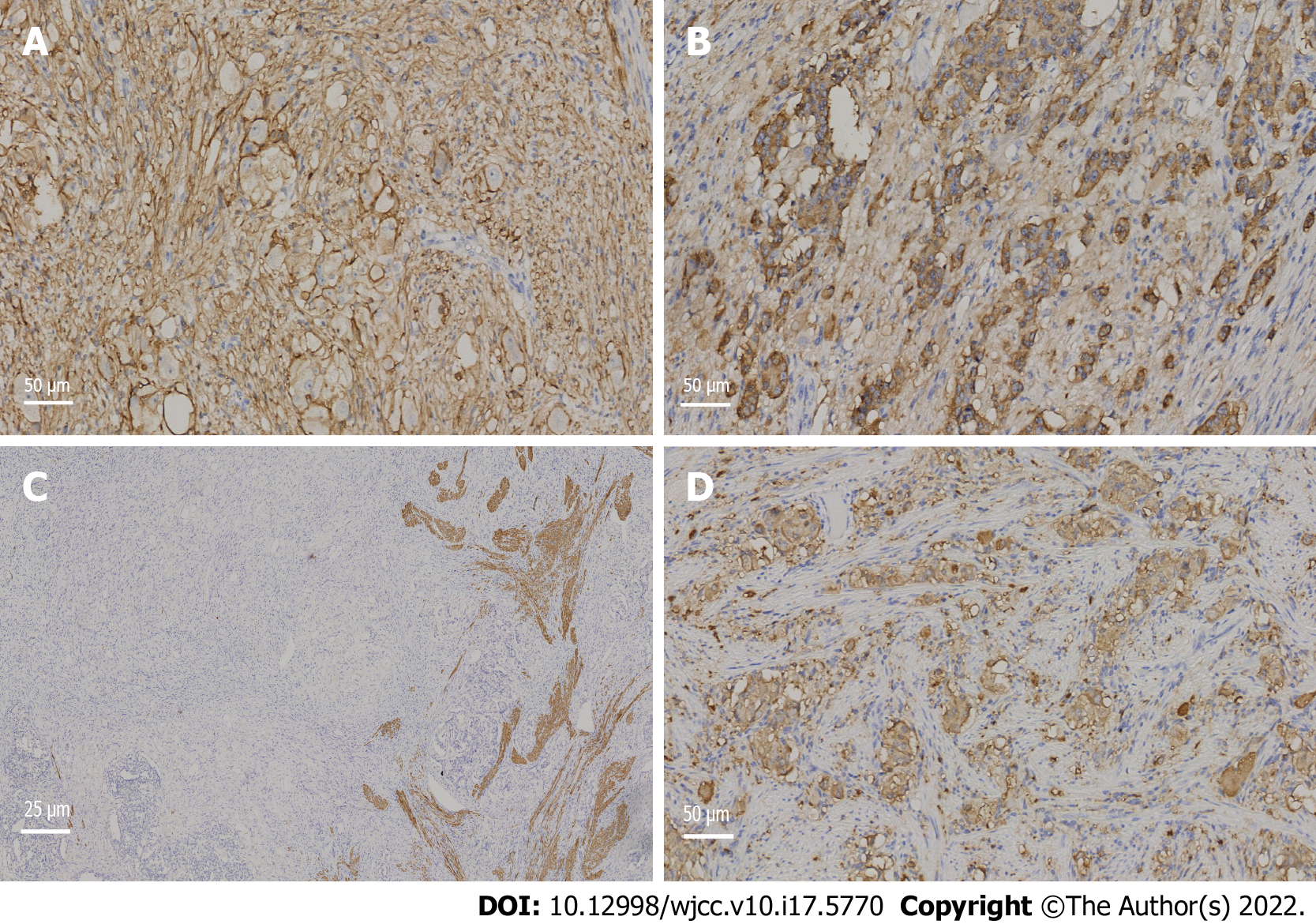
A 63-year-old female underwent upper gastrointestinal endoscopy at a local, grassroots hospital due to 1 mo of nausea and vomiting, and a large nipple was found in the descending part of the duodenum. The patient’s faecal occult blood test was positive. The patient had obvious symptoms of nausea and vomiting, often vomiting with no stomach contents and had lost 2 kg of weight within a month. Before the operation, we administered symptomatic treatment, such as replenishing gastric protective fluid. After excluding relevant surgical contraindications, endoscopic examination was performed on the patient in our hospital, and we found a protuberant mass above the nipple of the descending duodenum, with a smooth surface and a diameter of approximately 0.5 cm. A 12 MHz ultrasound probe showed that the tumour originated from the submucosa and showed low echo. We used a nylon noose to trap the tumour, cut the bottom of the base by snaring with an electrocurrent, and clamped the wound with a titanium clip to stop the bleeding (Figure 1). To confirm the diagnosis, the excised specimens were sent for pathological examination and immunohistochemistry. One week after the operation, the patient recovered smoothly and was discharged from the hospital. The pathological results showed that the tumour in the descending part of the duodenum was a NET (grade 1) with schwannoma, and the cutting edge was negative (Figure 2). The results of immunohistochemical staining indicated that the tumour cells were positive for antigen KI-67, broad-spectrum cytokeratin, CD56, synaptophysin (Syn), chromogranin A (CgA), S-100, nerve specific enolase, CD68, CD163, and myoglobin and were negative for CD34, succinate dehydrogenase B, CD117, DOG-1, smooth muscle actin, desmin, cytokeratin (CK) 7, CK20, and myogenic differentiation 1 (Figures 3 and 4).
The patient has a history of infection with tuberculosis 40 years ago. The history of surgical trauma was bronchiectasis in 2015, hysterectomy and minimally invasive hysteroptosis in 2020.
Parents have a history of hypertension.
Mild tenderness in the abdomen, no rebound pain.
Immunohistochemical results showed that the mass was a rare NET with neurilemmoma.
Mediastinal computed tomography (CT) showed no tumour metastasis.
Because this patient does not have other systemic diseases, multidisciplinary experts were not invited to discuss it.
NET of the descending part of the duodenum complicated with schwannoma.
We removed the tumour by electrocoagulation and gave the patient some other symptomatic treatment to help stopping vomiting and protect the stomach.
Mediastinal CT showed no tumour metastasis, and the prognosis of the patient is good.
There may be rare cases of NETs with schwannoma in the descending part of the duodenum worldwide, but there are no clinical reports. To the best of our knowledge, this is the first clinical case report of a duodenal NET complicated with schwannoma, which has high clinical value. Endoscopic NETs and schwannomas of the duodenum do not have specific features and are often mistaken for enlarged duodenal papilla, resulting in missed diagnosis and worsening of the disease. Endoscopic ultrasonography (EUS) is of high value in the diagnosis of these two kinds of tumours. Under EUS, most of the lesions are hypoechoic lesions originating from the submucosa, with clear boundaries and homogeneous internal echoes, which is consistent with our ultrasound results[3]. Duodenal schwannoma is extremely rare in gastrointestinal mesenchymal tumours, and only a few cases have been reported thus far. Duodenal neurilemmoma is often found by accident and is difficult to diagnose before surgery. There was no typical duodenal schwannoma under ordinary endoscopy. Due to the rare nature of duodenal schwannoma, no typical endoscopic ultrasonographic features have been reported[4]. The immunohistochemical results of the specimen remain the gold standard for diagnosis. NET cells are often positive for CgA, CD56, CK, and Syn, while schwannoma cells are often positive for S-100[5], which is consistent with our immunohistochemical results. Endoscopic treatment is usually the first choice for gastrointestinal NETs or schwannomas with diameters less than 1 cm, as it does not invade the lamina propria and because endoscopic treatment has the characteristics of less trauma, less cost, good prognosis, and easy follow-up after the operation[6]. It has been reported that snare polypectomy has a very high complete resection rate of gastrointestinal NETs (93.8%), and this rate may be high for several reasons. First, decoy polypectomy is more commonly used in smaller tumours (< 5.2 mm), and the appearance of polyps is more likely to be limited to the mucosa. The second reason is that electrosurgical devices, such as argon plasma coagulators, damage a larger field of vision during treatment. Therefore, for some small gastrointestinal NETs with specific shapes, the use of decoy electrocoagulation is completely effective[7]. In this case, we used EUS to determine the lesion level and endoscopic electrocoagulation for R0 resection, suggesting the feasibility and broad prospect of early endoscopic diagnosis and treatment of the tumour. The KI-67 index of the specimen was approximately 1%, suggesting that the NET phase was G1. In addition, we examined the vertical edge of the specimen with a high-power microscope. The vertical edge was negative, and there was no lymphatic invasion, which proved that we successfully removed the tumour completely. Mediastinal CT showed no tumour metastasis, and the prognosis of the patient is good.
To the best of our knowledge, this is the first publication of a neuroendocrine tumour of descending duodenum complicated with schwannoma. We removed the tumour by electrocoagulation completely and the patient recovered and was discharged.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D, D
Grade E (Poor): 0
P-Reviewer: Cerwenka H; Austria, Endo S; Japan, Symeonidis N; Greece S-Editor: Guo XR L-Editor: Filipodia P-Editor: Guo XR
| 1. | Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia. 2017;19:991-1002. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 405] [Cited by in RCA: 482] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 2. | Madero Velázquez L, Uceda F, Buendía L. Duodenal schwannoma, an infrequent entity. Rev Esp Enferm Dig. 2021;113:548-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | De Angelis C, Manfrè SF, Bruno M, Pellicano R. Hegemony and cost-effectiveness of endoscopic ultrasound (EUS) in the field of gastroenteropancreatic-neuroendocrine tumors (GEP-NETs). Minerva Med. 2014;105:363-370. [PubMed] |
| 4. | Mori Y, Kurita A, Yazumi S. Gastrointestinal: Schwannoma of the duodenum. J Gastroenterol Hepatol. 2020;35:1855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Bellizzi AM. Immunohistochemistry in the diagnosis and classification of neuroendocrine neoplasms: what can brown do for you? Hum Pathol. 2020;96:8-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (1)] |
| 6. | Scherübl H, Cadiot G. Early Gastroenteropancreatic Neuroendocrine Tumors: Endoscopic Therapy and Surveillance. Visc Med. 2017;33:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Sun W, Wu S, Han X, Yang C. Effectiveness of Endoscopic Treatment for Gastrointestinal Neuroendocrine Tumors: A Retrospective Study. Medicine (Baltimore). 2016;95:e3308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |