Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5487
Peer-review started: December 8, 2021
First decision: January 10, 2022
Revised: January 11, 2022
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: June 6, 2022
Processing time: 175 Days and 23.4 Hours
Specific pulmonary infection could seriously threaten the health of pilots and their companions. The consequences are serious. We investigated the clinical diagnosis, treatment, and medical identification of specific pulmonary infections in naval pilots.
We analyzed the medical waiver and clinical data of four pilots with specific pulmonary infections, who had accepted treatment at the Naval Medical Center of Chinese People’s Liberation Army between January 2020 and November 2021, including three cases of tuberculosis and one of cryptococcal pneumonia. All cases underwent a series of comprehensive treatment courses. Three cases successfully obtained medical waiver for flight after being cured, while one was grounded after reaching the maximum flight life after being cured.
Chest computed tomography scanning should be used instead of chest radiography in pilots’ physical examination. Most pilots with specific pulmonary infection can be cured and return to flight.
Core tip: Pilots are mostly young without underlying medical conditions; thus, the rate of lung infection is low. Lack of characteristic clinical manifestations of specific pulmonary infection can lead to misdiagnosis and delay treatment. Specific lung infection aggravates pilots’ health, and causes spread of pathogens in air forces. Chest computed tomography (CT) should be used instead of radiography for annual physical examination. When pilots are diagnosed with specific lung infection, related tests and CT should be used to screen the same camp to prevent further infections. After active treatment, most pilots with specific pulmonary infection can be cured and return to flight.
- Citation: Zeng J, Zhao GL, Yi JC, Liu DD, Jiang YQ, Lu X, Liu YB, Xue F, Dong J. Clinical diagnosis, treatment, and medical identification of specific pulmonary infection in naval pilots: Four case reports. World J Clin Cases 2022; 10(16): 5487-5494
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5487.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5487
Cryptococcal pneumonia is more common in immunodeficient people; however, in recent years, the incidence of cryptococcal pneumonia has been increasing in people with normal immune function[1,2]. While it is rare to see pilots infected with cryptococcal pneumonia, this infection may lead to central nervous system infection and serious consequences. Tuberculosis has been reported in pilots at home and abroad, ranking first in the respiratory disease spectrum of hospitalized pilots in China[3]. Most lung-specific infections caused by Cryptococcus neoformans or Mycobacterium tuberculosis have insidious onset and prolonged course of disease. The course of diagnosis and treatment takes more than 6 mo, and serious complications may occur that may threaten the physical and mental health of pilots. This may lead to grounding, which is a serious threat to the combat effectiveness of naval aviation corps. Therefore, it is necessary to carry out targeted research on it.
From January 2020 to November 2021, four naval pilots with specific pulmonary infection were successfully diagnosed and treated in the Aviation Disease Department of PLA Naval Medical Center, including three cases of tuberculosis and one of cryptococcal pneumonia. Three cases successfully obtained medical waiver for flight after being cured, and one was grounded after reaching the maximum flight life. The clinical data were summarized and analyzed to explore the preventive countermeasures of specific pneumonia in naval pilots.
Case 1: A male fighter pilot, age 33 years, had multiple lumps and shadows in his left lung found by physical examination for 1 d.
Case 2: A male helicopter pilot, age 30 years, had multiple patchy and nodular shadows in the left upper lung found by physical examination for 4 d.
Case 3: A male fighter pilot, age 34 years, had nodules in the upper apical segment of the right lung found by physical examination for 2 d.
Case 4: A male fighter pilot, age 48 years, had pulmonary nodules found on physical examination for 2 d.
Case 1: Two weeks before admission, the patient lost 10 kg due to fitness. One week before onset, he fished by the lake for 2 d. He reported occasional cough, usually accompanied by expectoration, but with no aggravation in the recent past.
Case 2: Although the patient presented without fever, cough, or other symptoms, physical examination showed multiple patchy and nodular shadows in the left upper lung, so the patient was admitted to hospital for 4 d.
Case 3: Although the patient presented without fever, cough, or other symptoms, physical examination showed nodules in the upper apical segment of right lung, so the patient was admitted to hospital.
Case 4: Pulmonary nodules were found in physical examination for 2 d, so he was admitted to hospital.
Case 1: Patient had a smoking history of 25 cigarettes per day for 13 years.
Case 4: Patient had two episodes of blood-tinged sputum 2 years ago. However, he had no fever and recovered after anti-infective therapy.
No other abnormal health conditions were reported in the other two cases.
All four cases had no specific history of genetic diseases.
All four cases had no positive signs found on physical examination.
Case 1: Hemogram, C-reactive protein (CRP), erythrocyte sedimentation rate, procalcitonin, G test, mycoplasma, Chlamydia, virus, tuberculosis antibody and syphilis, acquired immunodeficiency syndrome (AIDS), hepatitis C, and hepatitis B tests were all normal. T-SPOT.TB test was normal. Lymphocyte subtypes test, immunoassay, and sputum smear and culture were all normal. Cryptococcal capsular polysaccharide antigen (colloidal gold method) was positive with a titer of 1:20. Routine inspections showed that bacteria, fungi, acid-fast bacilli, cast-off cells, Pneumocystis jiroveci pneumonia, ink staining and mycobacterial culture results were normal. Cerebrospinal fluid, blood culture, middle urine culture and fecal culture were all normal.
Case 2: Hemogram, CRP, erythrocyte sedimentation rate, procalcitonin, G test, mycoplasma, Chlamydia, virus, and tuberculosis antibody were all normal. M. tuberculosis interferon- release assay was positive, tuberculin test strongly positive (+++), and sputum smear was negative.
Case 3: Hemogram, CRP, erythrocyte sedimentation rate, procalcitonin, G test, mycoplasma, Chlamydia, virus, and tuberculosis antibody were all normal. M. tuberculosis interferon- release test was positive, and tuberculin test was positive (++). Sputum smear was negative. G test, GM test, cryptococcal capsular polysaccharide antigen and Aspergillus fumigatus IgG and IgM were all negative. T cells subsets and immunity were normal. T-SPOT.TB test was positive (A wells of 56, B wells of 4), and tuberculosis antibody was positive after examination.
Case 4: Hemogram, CRP, erythrocyte sedimentation rate, procalcitonin, G test, Mycoplasma, Chlamydia, virus, and tuberculosis antibody were all normal. M. tuberculosis interferon- release test was positive, and tuberculin test was positive (++). Sputum smear was negative.
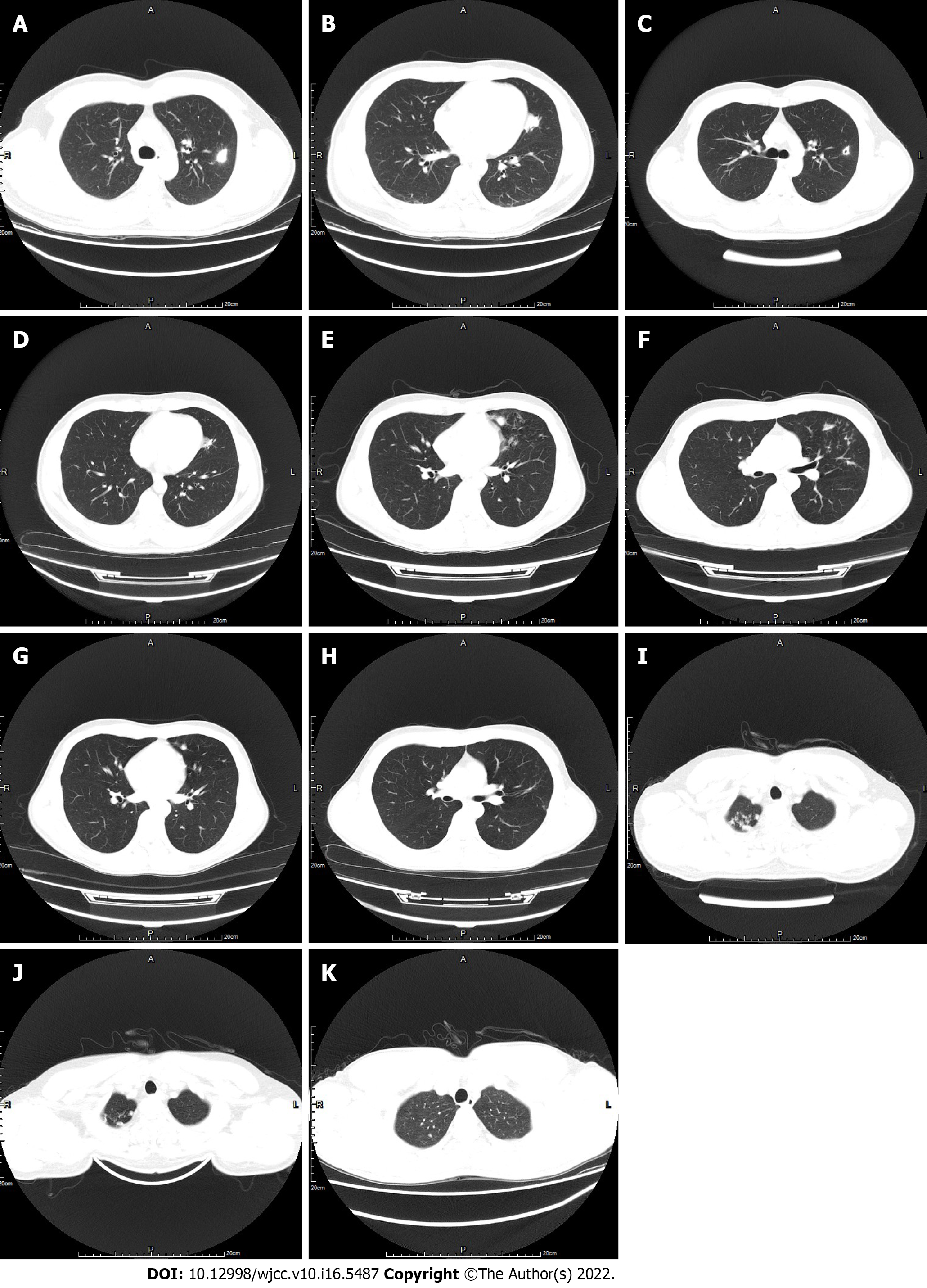
Case 1: Chest computed tomography (CT) showed that there were multiple patchy high-density shadows in the upper lobe of the left lung, with clear boundaries, patchy high-density shadows in the edge of the focus, with CT value of 30–45 HU and enhancement after intensification, with CT value of 35–80 HU, and the larger one was about 25 mm × 20 mm; a lesion in the inferior lingular segment could be seen with blood vessel shadow passing through, the tube wall was smooth, patchy halo was seen around the lesion, and no lymph node enlargement was found in the mediastinum and hilum. Bronchoscopy showed no abnormality. Bronchoalveolar lavage was performed in the posterior segment of the left upper apex, head magnetic resonance imaging and electroencephalogram (EEG) was all normal (Figure 1A–D).
Case 2: Chest CT showed that patchy and nodular shadows with increased density were found in the posterior and lingular segment of the upper lobe apex of left lung, with a small amount of bronchiectasis and thickening of the tube wall; micronodular shadow with a diameter < 3 mm was found in the posterior basal segment of the inferior lobe of left lung, with clear boundary, and no enlarged lymph nodes were found in the mediastinum and hilum. Bronchoscopy showed scar-like stenosis at the B1+2C opening in the superior lobe of the left lung, nodular protuberance on the wall of left B5 tube, uneven mucosa and positive GeneXpert in bronchoalveolar lavage fluid (Figure 1E–H).
Case 3: Chest CT showed that there were several spotted and round-like shadows with increased density in the upper apex of the right lung, local induration and calcification of the lesions, which increased compared with 2019, local nodular thickening of the left oblique fissure pleura, unobstructed trachea and bronchus, and no enlarged lymph nodes in the mediastinum and hilum. Bronchoscopy showed normality, no acid-fast bacilli were found in bronchial lavage fluid, negative GeneXpert, and negative identification of delivered Mycobacterium species in bronchial lavage fluid (Figure 1I and J).
Case 4: Chest CT showed that there were four small nodules under the pleura of the upper apex segment of the right lung, the basal segment of the lower lobe and the anterior segment of the upper lobe of left lung, with clear boundaries, the largest of which was 6 mm in diameter, the trachea and bronchus were unobstructed, and no enlarged lymph nodes were found in the mediastinum and hilus. Bronchoscopy showed no obvious abnormality, and one acid-fast bacillus was found in bronchial lavage fluid (Figure 1K).
Cryptococcal pneumonia.
Secondary pulmonary tuberculosis/upper middle (negative smear, positive GeneXpert in bronchoalveolar lavage fluid).
Right upper lung tuberculosis, bacteria (-), GeneXpert (-).
Right upper lung tuberculosis, bacteria (+).
He was treated with intravenous fluconazole of 400 mg for 1 d. After 18 d of treatment, fluconazole 400 mg/d was taken orally for 6 mo.
The treatment plan was for the regimen of isoniazide (H), rifampicin (R), pyrazinamide (Z), and ethambutol (E), as 6 HRZE/6 HRE, and the course of treatment was 1 year.
The treatment regimen was 4 HRZE/2 HRE, and the course of treatment was 6 mo.
The treatment plan was 4 HRZE/2 HRE, and the course of treatment was 6 mo.
After 18 d of fluconazole treatment, chest CT showed that the lesion was obviously reduced, cryptococcal capsular polysaccharide antigen (colloidal gold method) was positive with a titer of 1:10 and the curative effect was clear. Instead, fluconazole 400 mg/d was taken orally for 6 mo. Chest CT before and after treatment is shown below (Figure 1C and D). In the follow-up, the patient was qualified in flight test and obtained a medical waiver for flight to date without cryptococcal infection.
In the follow-up, the patient was qualified in flight test and obtained a medical waiver for flight without tuberculosis recurrence.
In the follow-up, the patient was qualified in flight test and obtained a medical waiver for flight without tuberculosis recurrence.
He was grounded after reaching the maximum flight life after being cured.
Specific pulmonary infections caused by fungi, M. tuberculosis, viruses, etc. are common in people with impaired immune function, and the common infection route is inhaling aerosol particles containing pathogenic bacteria through the respiratory tract. Due to the lack of characteristic clinical manifestations and signs of specific pulmonary infection, misdiagnosis and missed diagnosis are easy to occur clinically and delay treatment. Specific lung infection not only aggravates the patient’s own lung infection, but also causes the spread of M. tuberculosis and other pathogens within the air force in which naval pilots live mainly in groups, resulting in serious consequences such as noncombat attrition. Therefore, it is necessary to improve the understanding of flight surgeons about such diseases to reduce misdiagnosis and mistreatment.
Pilots are mostly young people without underlying medical conditions. After multilayer physical examination for selection and annual physical examination, most of them are people with normal immune function, so the rate of specific lung infection is low. However, if the flight training task is arduous, pilots are prone to excessive fatigue and decreased immunity, which provides opportunities for pathogens, such as fungi and M. tuberculosis, to be inhaled and cause diseases. In this study, three fighter pilots and one helicopter pilot, aged 30–48 years, were diagnosed and treated for lung infections. The causes of the cryptococcal infection in Case 1 were analyzed as follows: (1) Deliberate weight loss through fitness during flight training, leading to a decrease in immunity from excessive fatigue and rapid weight loss; and (2) A large number of chickens and ducks can be found in the humid environment by the lake where the patient fished for 2 d before the onset of the disease, although there was no clear contact history with the birds.
At present, the routine physical examination of pilots is mainly chest radiography, which may lead to missed diagnosis of some early small lesions. Therefore, it is necessary to suggest that the annual physical examination of pilots adopt thin-layer chest CT plain scan, especially at the stage of selecting pilots. The chest CT in Case 1 showed multiple patchy shadows, halo sign at the edge, visible air bronchogram, blood vessels passing through the lesions, and small holes in the treatment process, which accorded with the imaging findings of cryptococcal pneumonia[4]. Case 2 showed multiple patches and nodular changes in the posterior segment of the upper apex with bronchiectasis on CT, and bronchoscopy showed lesions in the bronchial mucosa, which were consistent with tuberculosis[5]. Attention should be paid to strengthening the follow-up mechanism and compare the changes in lesions on CT every year. In Case 3, chest CT demonstrated that the right upper apical pulmonary nodules were larger than 2 years ago, and the old and new nodules coexisted with calcification, which was in line with the imaging characteristics of tuberculosis. After positive T-SPOT.TB examination, pulmonary tuberculosis was clinically diagnosed[6]. For suspicious lesions, those with atypical imaging manifestations should improve the detection of bacteria, fungi, M. tuberculosis, viruses and other pathogens and antigens. Case 1 was diagnosed with repeated positive capsular antigen detection and titer detection of Cryptococcus[5,6]. Bronchoscopy can be improved when there are no cough and expectoration symptoms, and bronchial lavage fluid is inspected for pathogens. In Case 4, a small number of acid-fast bacilli was found in bronchial lavage fluid, and in Case 2, airway lesions were found under bronchoscopy, and GeneXpert is positive, so tuberculosis was diagnosed[7]. All four cases in this group had no obvious symptoms and signs, and abnormalities were found after chest CT scanning during physical examination. The final diagnosis was made after improving the detection of pathogens, antigens, and antibodies and bronchoscopy with bronchoalveolar lavage. Timely improvement of auxiliary inspection and early diagnosis are the key to ensuring flight safety.
Cryptococcus has neurotropic characteristics, and it is necessary to further check whether there is central nervous system infection after cryptococcal pneumonia is diagnosed. The treatment of cryptococcal infection is mainly based on the Guidelines for the Management of Cryptococcal Disease of Infectious Diseases Society of America (IDSA) in 2010[8], and the treatment is graded according to evaluation of immune status, systemic dissemination and severity of respiratory symptoms, with a course of treatment of 6–12 mo. The standard treatment of pulmonary tuberculosis (4 drugs for fortification period, 2 or 3 for consolidation period) lasts for 6–12 mo[9,10]. Sufficient dose and course of treatment are recommended during the treatment, and hepatic and renal function and chest CT are re-examined every month to evaluate the curative effect and side effects of the drugs. Regular re-examination is still needed after cure to prevent recurrence.
The hidden onset and long course of treatment of specific pulmonary infections caused by fungi and M. tuberculosis are seriously harmful to the combat effectiveness of naval pilots. Flight surgeons at all levels should pay attention to the following clinical aeromedical points.
Enhanced preventive measures should be taken. Attention should be paid to the combination of work and rest during high-intensity flight training, the degree of fatigue and immune status of pilots, and timely arrangement of rest and recuperation. Focus should be placed on ventilation maintenance, regular ultraviolet disinfection, and chemical disinfection in working and living environment[11,12]. When necessary, indoor dryers should be added in humid environments, moldy and rotten substances cleaned up, food classified and managed, and tainted and expired food including fruits and vegetables treated. Contact with birds, cats and dogs in the working environment should be reduced. Health promotion and education should be enhanced to improve the understanding of flight surgeons and pilots on fungal infection, tuberculosis and other diseases. Chest CT scanning should be used instead of chest radiography and the image changes should be compared every year. When suspicious lesions are found, the detection of related etiology, antigen and antibody should be improved as soon as possible, and bronchoscopy should be performed when necessary. When pilots are diagnosed with tuberculosis, tuberculin test and chest CT should be carried out to screen people in the same camp to prevent collective infection[13,14]. It should be clear that patients with tuberculosis need to be isolated at home, provided with regular antituberculous therapy in sufficient doses and courses, and re-evaluated for their flight assessment after being cured. There should be concern about regular disinfection and microbiological testing of cockpits, oxygen masks, and breathing lines of pilots.
The infection rate of specific lung infection in pilots is low. Due to the lack of characteristic clinical manifestations, misdiagnosis can occur easily. Specific lung infection not only aggravates the pilots’ health, but also causes the spread of pathogens in air forces, with serious consequences. Chest CT scanning should be used instead of chest radiography in pilots’ physical examination. When pilots are diagnosed with specific lung infection, relevant tests and chest CT scanning should screen people in the same camp. After active treatment, most pilots with specific pulmonary infection can be cured and return to flight.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tasdemir Z, Turkey; Yazar U, Turkey S-Editor: Chen YL L-Editor: Kerr C P-Editor: Chen YL
| 1. | Alves VS, Leite-Aguiar R, Silva JPD, Coutinho-Silva R, Savio LEB. Purinergic signaling in infectious diseases of the central nervous system. Brain Behav Immun. 2020;89:480-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Jiang XQ, Zhang YB. Cryptococcal pneumonia in a human immunodeficiency virus-negative patient: A case report. World J Clin Cases. 2020;8:2038-2043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Wang N, Li T, Du X, Li Y, Sun M, Huan S, Zhang H, Wang L, Chen M, Huang F, Zhao Y. Effectiveness of the Integrated TB Surveillance System - China, 2018-2019. China CDC Wkly. 2020;2:190-193. [PubMed] |
| 4. | Obmann VC, Bickel F, Hosek N, Ebner L, Huber AT, Damonti L, Zimmerli S, Christe A. Radiological CT Patterns and Distribution of Invasive Pulmonary Aspergillus, Non-Aspergillus, Cryptococcus and Pneumocystis Jirovecii Mold Infections - A Multicenter Study. Rofo. 2021;193:1304-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yan C, Wang L, Lin J, Xu J, Zhang T, Qi J, Li X, Ni W, Wu G, Huang J, Xu Y, Woodruff HC, Lambin P. A fully automatic artificial intelligence-based CT image analysis system for accurate detection, diagnosis, and quantitative severity evaluation of pulmonary tuberculosis. Eur Radiol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Liu Y, Yao L, Wang F, Sun Z, Tan Y, Sha W. The TBAg/PHA ratio in T-SPOT.TB assay has high prospective value in the diagnosis of active tuberculosis: a multicenter study in China. Respir Res. 2021;22:165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Kaso AW, Hailu A. Costs and cost-effectiveness of Gene Xpert compared to smear microscopy for the diagnosis of pulmonary tuberculosis using real-world data from Arsi zone, Ethiopia. PLoS One. 2021;16:e0259056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Gassiep I, Douglas J, Emeto TI, Crawley K, Playford EG. Cryptococcal infections over a 15 year period at a tertiary facility & impact of guideline management. Mycoses. 2018;61:633-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Padmapriydarsini C, Mamulwar M, Mohan A, Shanmugam P, Gomathy NS, Mane A, Singh UB, Pavankumar N, Kadam A, Kumar H, Suresh C, Reddy D, Devi P, Ramesh PM, Sekar L, Jawahar S, Shandil RK, Singh M, Menon J, Guleria R; METRIF Team. Randomized trial of Metformin with Anti-tuberculosis drugs For Early Sputum Conversion in Adults with Pulmonary Tuberculosis. Clin Infect Dis. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Syburra T, Nicol E, Mitchell S, Bron D, Rosendahl U, Pepper J. To fly as a pilot after cardiac surgery. Eur J Cardiothorac Surg. 2018;53:505-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Lin J, Yan D, Fu J, Chen Y, Ou H. Ultraviolet-C and vacuum ultraviolet inducing surface degradation of microplastics. Water Res. 2020;186:116360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 146] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 12. | Kühn KP, Chaberny IF, Massholder K, Stickler M, Benz VW, Sonntag HG, Erdinger L. Disinfection of surfaces by photocatalytic oxidation with titanium dioxide and UVA light. Chemosphere. 2003;53:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 255] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 13. | Creswell J, Khan A, Bakker MI, Brouwer M, Kamineni VV, Mergenthaler C, Smelyanskaya M, Qin ZZ, Ramis O, Stevens R, Reddy KS, Blok L. The TB REACH Initiative: Supporting TB Elimination Efforts in the Asia-Pacific. Trop Med Infect Dis. 2020;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Garcia R, Spiegel JM, Yassi A, Ehrlich R, Romão P, A Nunes E, Zungu M, Mabhele S. Preventing Occupational Tuberculosis in Health Workers: An Analysis of State Responsibilities and Worker Rights in Mozambique. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |