Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5359
Peer-review started: August 7, 2021
First decision: October 2, 2021
Revised: October 7, 2021
Accepted: April 2, 2022
Article in press: April 2, 2022
Published online: June 6, 2022
Processing time: 299 Days and 4.4 Hours
The most common site of paragonimiasis is in the lungs. The migratory route passes through the duodenal wall, peritoneum, and diaphragm to the lungs; thus, the thoracic cavity and central nervous system, as well as the liver, intestine, and abdominal cavity may be involved. Here, we present a case of intraperitoneal paragonimiasis without other organ involvement, mimicking tuberculous peritonitis.
A 57-year-old man presented with recurrent abdominal pain for 4 wk. Physical examination revealed tenderness in the right lower quadrant. Laboratory findings showed complete blood counts within the normal range without eosinophilia. Multiple reactive lymph nodes and diffuse peritoneal infiltration were noted on abdominal computed tomography (CT). There were no abnormalities on chest CT or colonoscopy. Intraoperative findings of diagnostic laparoscopy for the differential diagnosis of tuberculous peritonitis and peritoneal carcinomatosis included multiple small whitish nodules and an abscess in the peritoneum. Pathological reports confirmed the presence of numerous eggs of Paragonimus westermani (P. westermani). A postoperative serum enzyme-linked immunosorbent assay revealed P. westermani positivity. Persistent and repetitive history-taking led him to retrospectively recall the consumption of freshwater crab. After 3 d of treatment with praziquantel (1800 mg; 25 mg/kg), he recovered from all symptoms.
In patients who require diagnostic laparoscopy for the differential diagnosis of tuberculous peritonitis and peritoneal carcinomatosis, repetitive history-taking and preoperative serologic antibody tests against Paragonimus may be helpful in diagnosing intraperitoneal paragonimiasis without other organ involvement.
Core Tip: Intraperitoneal Paragonimus without lung involvement can be misdiagnosed for tuberculous peritonitis, even with a negative stool test and normal eosinophil counts. In this case, a positive result on the preoperative serum antibody test for P. westmani may help patients recall history of crustacean consumption and prevent unnecessary surgery.
- Citation: Choi JW, Lee CM, Kim SJ, Hah SI, Kwak JY, Cho HC, Ha CY, Jung WT, Lee OJ. Ectopic peritoneal paragonimiasis mimicking tuberculous peritonitis: A care report. World J Clin Cases 2022; 10(16): 5359-5364
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5359.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5359
Infestation with Paragonimus species is the diagnosis of paragonimiasis. Although Paragonimus westermani (P. westermani) infested the lungs most commonly, in rare cases, they can be found only in other organs without the involvement of the lungs. In the case of Involvement of the lungs, it is diagnosed by the identification of P. westermani eggs in stool or sputum examination. The diagnosis of ectopic infection can be made when worms or eggs of characteristic shape are found on tissue. Enzyme-linked immunosorbent assay (ELISA) for antibodies or molecular identification by polymerase chain reaction (PCR) can be helpful for diagnosis.
The nervous system and gastrointestinal system are other areas that can be infested other than the lungs. Humans are infected with P. westermani in form of metacercariae by eating raw freshwater crustaceans. The metacercariae exocyst in the duodenum, and then pass through the intestinal wall, peritoneal cavity, diaphragm, and pleural cavity to the lung. Due to this migratory route, ectopic infections can occur such as peritoneum. Intraperitoneal paragonimiasis without lung involvement may be misdiagnosed as tuberculous peritonitis. However, in most cases, it can be differentiated through eosinophilia, a positive stool test, and typical medical history of crustacean consumption.
Here, we present a case of intraperitoneal paragonimiasis mimicking tuberculous peritonitis with no involvement of lungs, no eosinophilia, and a negative stool test.
A 57-year-old man was admitted for the evaluation of recurrent lower abdominal pain that had persisted for 2 mo.
He received intermittent medications for abdominal pain in a private clinic for 2 mo. Two days before the visit, he underwent abdominal computed tomography (CT) at another hospital and was transferred for the differential diagnosis of tuberculous peritonitis and peritoneal carcinomatosis.
He received a diagnosis of a 5-mm-sized rectal neuroendocrine tumor at another hospital one year prior and underwent endoscopic mucosal resection.
He has smoked 1 pack a day for 30 years. He has consumed approximately 57 g of alcohol per week.
Physical examination revealed mild tenderness in the right lower quadrant. The patient’s temperature was 36.4 °C, heart rate was 72 bpm, respiratory rate was 18 breaths per minute, blood pressure was 125/85 mmHg
The white blood cell count was 4960/mm3 (reference, 4000-10000/mm3), the proportion of eosinophils was 4.4% (reference, 1%-5%), and there were no abnormal findings in the laboratory findings. The C-reactive protein level was 1.7 mg/L, which was within the normal range (reference, 0-5 mg/L). The carcinoembryonic antigen was 1.43 ng/mL (reference, 0-3.4 ng/mL) and carbohydrate antigen 19-9 was 13.98 U/mL (reference, 0-34 U/mL). The interferon-gamma release assay test result was negative, and the results of tuberculosis tests, including sputum stain, culture, and PCR, were all negative. The stool examination result was negative.
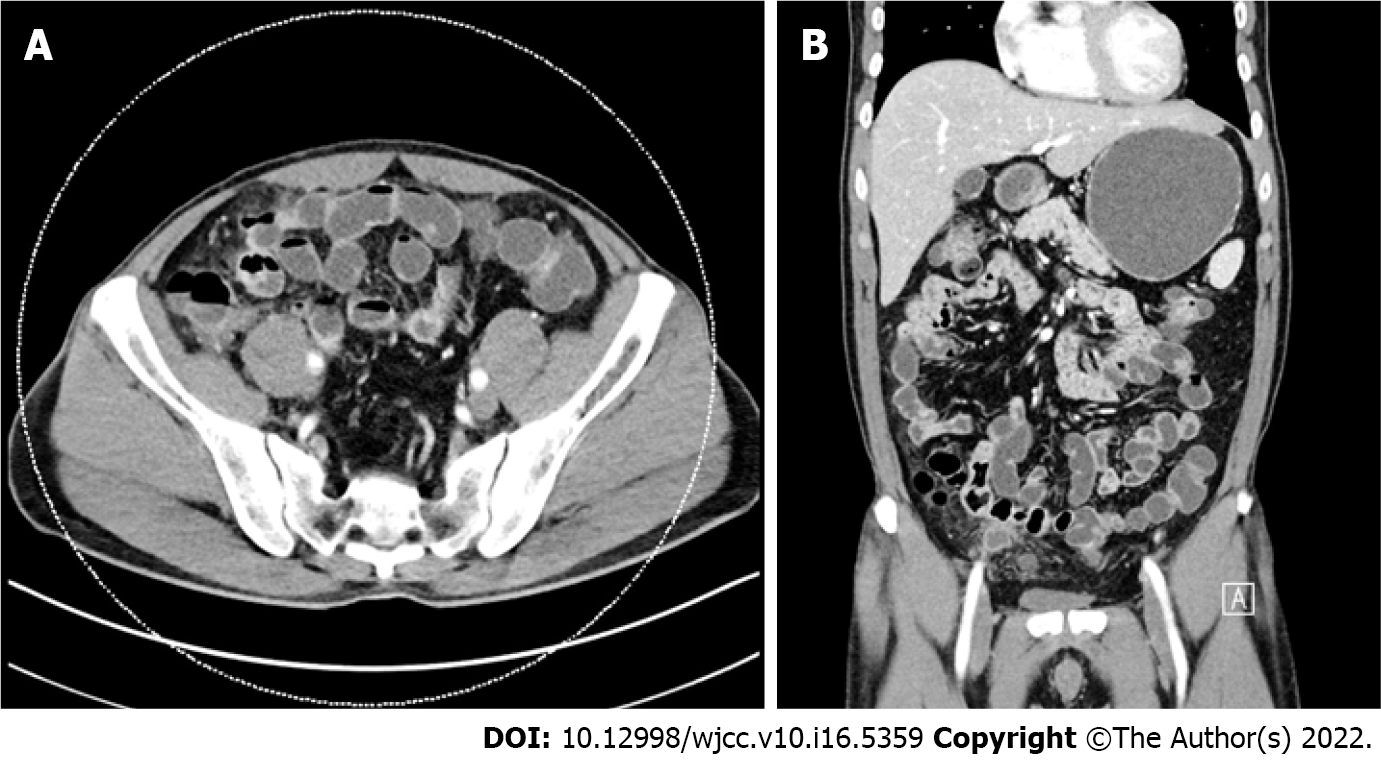
Diffuse peritoneal infiltration and subtle wall thickening of the right colon with multiple reactive lymph nodes were found on abdominal CT (Figure 1). Meanwhile, no lung lesions were observed on chest CT, and no enlarged lymph nodes were observed. On colonoscopy, a scar caused by a previous mucosal resection was observed 2 cm above the anal valve, and there was no evidence of recurrence. Only atrophic gastritis was found on esophagogastroduodenoscopy.
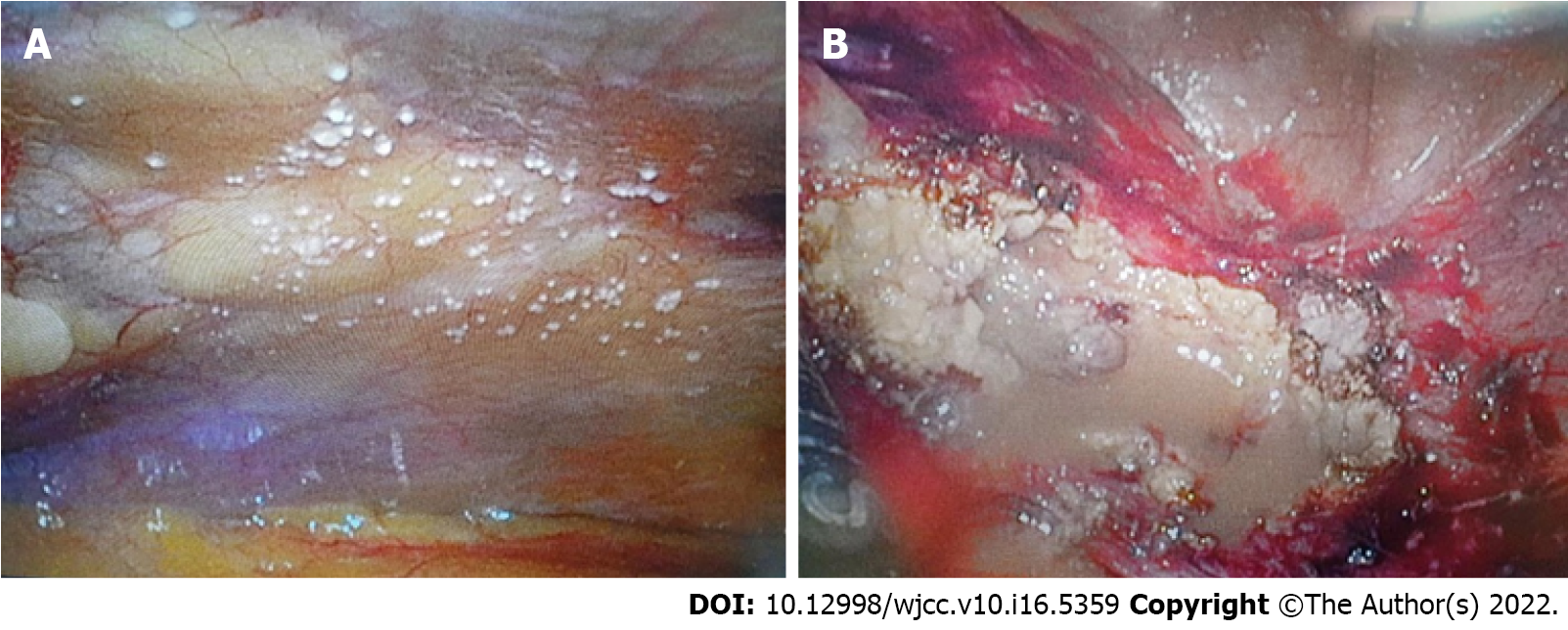
Exploratory laparoscopy was performed to determine the cause of the peritoneal lesions. Intraoperative findings showed multiple small whitish nodules and an abscess in the peritoneum (Figure 2). Peritoneal nodules 1-2 mm in size were observed throughout the abdominal cavity, and excisional biopsy was performed. During right pelvic wall dissection, abscess pockets with pus surrounded by the omentum were observed. Omentectomy was performed for some of the omentum. An incidental appendectomy was also performed.
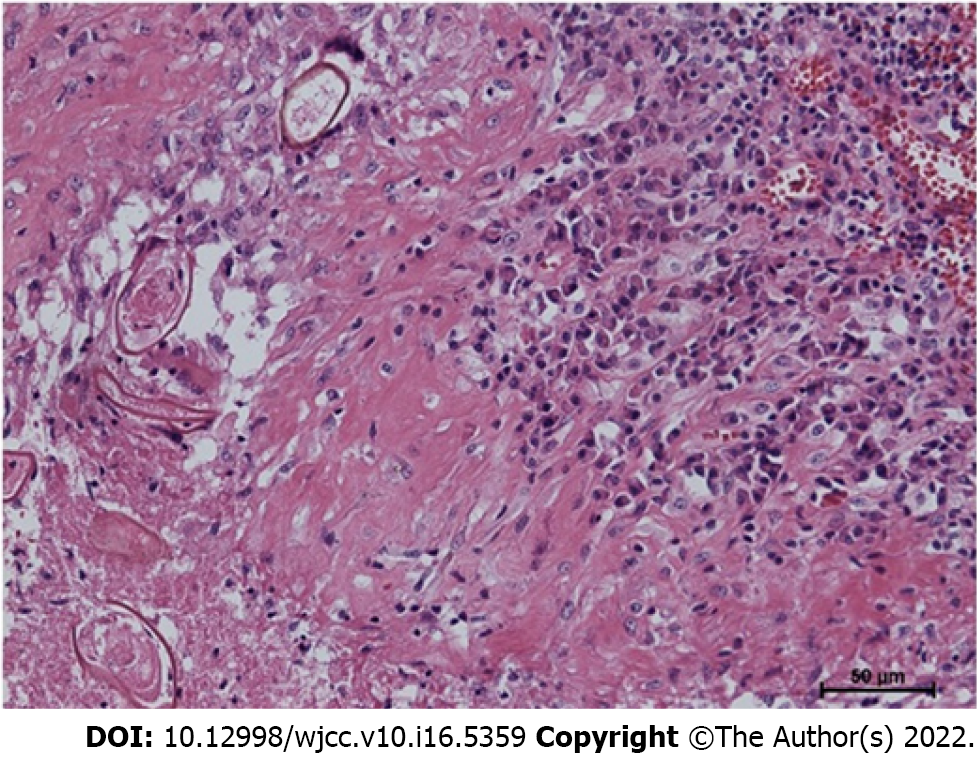
Based on the pathological reports, numerous eggs of P. westermani were confirmed in all specimens of the excisional biopsy, omentectomy, and appendectomy (Figure 3).
A postoperative ELISA revealed positivity for antibodies against P. westermani in the serum. There were no specific findings on brain CT.
During retrograde history-taking, it was reported that he often consumed food consisting of raw freshwater crab several months prior.
The final diagnosis was intraperitoneal paragonimiasis without other organ involvement.
He was given a total of 1800 mg (25 mg/kg) of praziquantel in 3 divided doses per day for 3 d and he recovered from all symptoms. He was discharged on the 10th day of hospitalization.
Recurrence was not observed in the subsequent 2 years.
This case was intraperitoneal paragonimiasis, which was difficult to differentiate from tuberculous peritonitis and peritoneal carcinomatosis. This is because he denied crustacean consumption during his first history-taking, the stool test result was negative, and there was no eosinophilia or lung involvement.
There have been previous reports of intraperitoneal paragonimiasis, but with differentiating points, such as intrathoracic lesions[1], intraperitoneal calcifications[2,3], and eosinophilia[4], whereas no signs of paragonimiasis, such as calcification or eosinophilia, were observed in the present case. In a Korean case report[5], similar to the present case, a 57-year-old woman presented with paragonimiasis mimicking omental seeding nodules and transverse colonic wall thickening without eosinophilia and lung involvement, and an intraoperative frozen biopsy was performed for diagnosis. She was treated with praziquantel for 2 d.
In addition, despite the denial of the possibility of parasitic infestation at the time of history-taking in the present case, he recalled that he had consumed soy sauce crab several months before being diagnosed with paragonimiasis through surgery. Soy sauce crab is a dish that commonly causes paragonimiasis in Korea.
For the differential diagnosis of tuberculous peritonitis mimicking peritoneal infiltration without eosinophilia and other involvement, especially with a negative latent tuberculosis test result, serologic ELISAs for antibodies against Paragonimus can be helpful. If serologic antibody tests for parasitic infestations had been performed before diagnostic laparoscopy, unnecessary surgery may have been avoided through repeated medical history taking. He was treated with praziquantel for 3 d after receiving the diagnosis of intraperitoneal paragonimiasis, and no recurrence was observed for 2 years thereafter.
Even with normal stool tests and eosinophil counts on complete blood count, preoperative serologic antibody tests against Paragonimus may be helpful in diagnosing intraperitoneal paragonimiasis without other organ involvement in patients who require diagnostic laparoscopy for the differential diagnosis of tuberculous peritonitis and peritoneal carcinomatosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu YC, China S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Kim AY. [Heterotopic paragonimiasis presented by intra-abdominal masses]. Korean J Gastroenterol. 2013;61:351-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Jeong WK, Kim Y, Kim YS, Park DW, Park CK, Baek HK, Park YW. Heterotopic paragonimiasis in the omentum. J Comput Assist Tomogr. 2002;26:1019-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kim MJ, Kim SH, Lee SO, Choi SH, Kim YS, Woo JH, Yoon YS, Kim KW, Cho J, Chai JY, Chong YP. A Case of Ectopic Peritoneal Paragonimiasis Mimicking Diverticulitis or Abdominal Abscess. Korean J Parasitol. 2017;55:313-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Kim JY, Kang CM, Choi GH, Yang WI, Sim SB, Kwon JE, Kim KS, Choi JS, Lee WJ, Kim BR. Laparoscopic excision of intra-abdominal paragonimiasis. Surg Laparosc Endosc Percutan Tech. 2007;17:556-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Lee CH, Kim JH, Moon WS, Lee MR. Paragonimiasis in the abdominal cavity and subcutaneous tissue: report of 3 cases. Korean J Parasitol. 2012;50:345-347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |